Abstract
Hypothesis.
Mortality in children with shock is more closely related to the nature, rather than the magnitude (base deficit/excess), of a metabolic acidosis.
Objective.
To examine the relationship between base excess (BE), hyperlactataemia, hyperchloraemia, 'unmeasured' strong anions, and mortality.
Design.
Prospective observational study set in a multi-disciplinary Paediatric Intensive Care Unit (PICU).
Patients.
Forty-six children, median age 6 months (1.5–14.4), median weight 5 kg (3.2–8.8), admitted to PICU with shock.
Interventions.
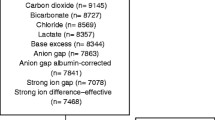
Predicted mortality was calculated from the paediatric index of mortality (PIM) score. The pH, base excess, serum lactate, corrected chloride, and 'unmeasured' strong anions (Strong Ion Gap) were measured or calculated at admission and 24 h.
Measurements and results.
Observed mortality (n=16) was 35%, with a standardised mortality ratio (SMR) of 1.03 (95% CI 0.71–1.35). There was no significant difference in admission pH or BE between survivors and nonsurvivors. There was no association between elevation of 'unmeasured' anions and mortality, although there was a trend towards hyperchloraemia in survivors (P=0.08). Admission lactate was higher in nonsurvivors (median 11.6 vs 3.3 mmol/l; P=0.0003). Area under the mortality receiver operating characteristic curve for lactate was 0.83 (955 CI 0.70–0.95), compared to 0.71 (95% CI 0.53–0.88) for the PIM score. Admission lactate level >5 mmol/l had maximum diagnostic efficiency for mortality, with a likelihood ratio of 2.0.
Conclusion.
There is no association between the magnitude of metabolic acidosis, quantified by the base excess, and mortality in children with shock. Hyperlactataemia, but not elevation of 'unmeasured' anions, is predictive of a poor outcome.

Similar content being viewed by others
References
Davis JW, Shackford SR, Holbrook TL (1991) Base deficit as a sensitive indicator of compensated shock and tissue oxygen utilization. Surg Gynecol Obstet 173:473–476
Siegel JH, Rivkind AI, Dalal S, Goodarzi S (1990) Early physiologic predictors of injury severity and death in blunt multiple trauma. Arch Surg 125:498–508
Smith I, Kumar P, Molloy S, Rhodes A, Newman PJ, Grounds RM, Bennett ED (2001) Base excess and lactate as prognostic indicators for patients admitted to intensive care. Intensive Care Med 27:74–83
Rixen D, Raum M, Bouillon B, Lefering R, Neugebauer E (2001) Base deficit development and its prognostic significance in post-trauma critical illness: an analysis by the trauma registry of the Deutsche Gesellschaft fur unfallchirurgie. Shock 15:83–89
Boyd O, Mackay CJ, Lamb G, Bland JM, Grounds RM, Bennett ED (1993) Comparison of clinical information gained from routine blood-gas analysis and from gastric tonometry for intramural pH. Lancet 341:142–146
Shann F, Pearson G, Slater A, Wilkinson K (1997) Paediatric index of mortality (PIM): a mortality prediction model for children in intensive care. Intensive Care Med 23:201–207
The Advanced Life Support Group (2001) Acid-base balance. In: Advanced paediatric life support. The practical approach (3rd edn). BMJ Books, London, pp 265–266
Bakker J, Coffernils M, Leon M, Gris P, Vincent J-L (1991) Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock. Chest 99:956–962
Hatherill M, Sajjanhar T, Tibby SM, Champion MP, Anderson D, Marsh MJ, Murdoch IA (1997) Serum lactate as a predictor of mortality after paediatric cardiac surgery. Arch Dis Child 77:235–238
Deshpande SA, Ward Platt MP (1997) Association between blood lactate and acid-base status and mortality in ventilated babies. Arch Dis Child 76:F15–F20
Hatherill M, McIntyre AG, Wattie M, Murdoch IA (2000) Early hyperlactataemia in critically ill children. Intensive Care Med 26:314–318
Weil MH, Afifi AA (1970) Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock). Circulation 41:989–1001
Stacpoole PW, Wright EC, Baumgartner TG, Bersin RM, Buchalter S, Curry SH (1994) Natural history and course of acquired lactic acidosis in adults. AM J Med 97:47–54
Mizock BA, Falk JL (1992) Lactic acidosis in critical illness. Crit Care Med 20:80–93
Stewart PA (1983) Modern quantitative acid-base chemistry. Can J Physiol Pharmacol 61:1444–1461
Figge J, Mydosh T, Fencl V (1992) Serum proteins and acid-base equilibria: a follow-up. J Lab Clin Med 120:713–719
Kellum JA, Kramer DJ, Pinsky MR ()1995 Strong ion gap: a methodology for exploring unexplained anions. J Crit Care 10:51–55
Kellum J, Kramer DJ, Pinsky MR (1994) Unexplained positive anion gap metabolic acidosis in end stage liver disease (ESLD). Crit Care Med 22:A209
Kellum JA, Bellomo R, Kramer DJ, Pinsky MR (1995) Hepatic anion flux during acute endotoxemia. J Appl Physiol 78:2212–2217
Kellum JA, Bellomo R, Kramer DJ, Pinsky MR (1997) Fixed acid uptake by visceral organs during early endotoxemia. Adv Exp Med Biol 411:275–279
Balasubramanyan N, Havens PL, Hoffman GM (1999) Unmeasured anions identified by the Fencl-Stewart method predict mortality better than base excess, anion gap, and lactate in patients in the pediatric intensive care unit. Crit Care Med 27:1577–1581
McFarlane C, Lee A (1994) A comparison of Plasmalyte 148 and 0.9% saline for intra-operative fluid replacement. Anaesthesia 49:779–781
Scheingraber S, Rehm M, Sehmisch C, Finsterer U (1999) Rapid saline infusion produces hyperchloremic acidosis in patients undergoing gynecologic surgery. Anesthesiology 90:1265–1270
Skellett S, Mayer A, Durward A, Tibby SM, Murdoch IA (2000) Chasing the base deficit: hyperchloraemic acidosis following 0.9% saline fluid resuscitation. Arch Dis Child 83:514–516
Durward A, Skellett S, Mayer A, Taylor D, Tibby SM, Murdoch IA (2001) The value of the chloride:sodium ratio in differentiating the aetiology of metabolic acidosis. Intensive Care Med 27:828–835
Shann F (1998) Normal values: blood and sweat. In: Drug doses. Collective, Melbourne, p 75
Rapoport J, Teres D, Lemeshow S, Gehlbach S (1994) A method for assessing the clinical performance and cost-effectiveness of intensive care units: a multicenter inception cohort study. Crit Care Med 22:1385–1391
Fencl V, Jabor A, Kazda A, Figge J (2000) Diagnosis of metabolic acid-base disturbances in critically ill patients. Am J Respir Crit Care Med 162:2246–2251
Bakker J, Gris P, Coffernils M, Kahn RJ, Vincent J-L (1996) Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg 171:221–226
Duke TD, Butt W, South M (1997) Predictors of mortality and multiple organ failure in children with sepsis. Intensive Care Med 23:684–692
Friedman G, Berlot G, Kahn RJ, Vincent J-L (1995) Combined measurements of blood lactate concentrations and gastric intramucosal pH in patients with severe sepsis. Crit Care Med 23:1184–1193
Bernardin G, Pradier C, Tiger F, Deloffre P, Mattei M (1996) Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock. Intensive Care Med 22:1725
Gutierrez G, Wulf ME (1996) Lactic acidosis in sepsis: a commentary. Intensive Care Med 22:616
Duke T (1999) Dysoxia and lactate. Arch Dis Child 81:343350
Acknowledgements.
The authors wish to thank Dr Andrew Durward of Guy's Hospital, London, for helpful comment and discussion.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial support. This study was funded in part by a research grant from the Institute of Child Health, University of Cape Town
Appendix 1
Appendix 1
Formulae [17]
Strong ion difference (apparent) (SIDa) = (Na + K + Mg + Ca)−(Cl + lactate)
Strong ion difference (effective) (SIDe) = (1000 × 2.46E-11 × pCO2 / 10−pH) + [albumin × (0.123 × pH −0.631)] + [PO4 × (0.309 × pH −0.469)]
Strong ion gap (SIG) = 'Unmeasured' anions = SIDa−SIDe
Corrected chloride (Clcorr) = Cl × 140 / Na
Rights and permissions
About this article
Cite this article
Hatherill, M., Waggie, Z., Purves, L. et al. Mortality and the nature of metabolic acidosis in children with shock. Intensive Care Med 29, 286–291 (2003). https://doi.org/10.1007/s00134-002-1585-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-002-1585-y