Abstract
Background
Hemiarthroplasty is an established treatment for femoral neck fractures (FNF) in old age; however, approximately 20–30% of patients die within 1 year after surgery. Periprosthetic joint infections (PJI) are one of the severest complications and associated with a high mortality rate. In this retrospective study of aged patients with FNF treated with hemiarthroplasty, the incidence of PJI was evaluated with respect to the influence of the delay to and timing of surgical treatment.
Patients and methods
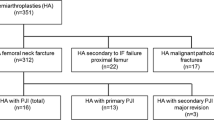
The data of patients suffering from FNF and admitted to this hospital between January 2012 and December 2014 were evaluated. Demographic data, timing of surgery, intraoperative complications, PJI and other general complications, hospitalization time and mortality were recorded.
Results
In this study 178 patients were included in the follow-up (114 women and 64 men). The median age of the patients was 83 years (range 55–105 years). The rate of PJI was 3.9% (7/178) and mortality was 5.6% (10/178). Patients with PJI after hemiarthroplasty had a significantly longer hospital stay (17 vs. 10 days, p < 0.001) and a higher mortality (28% vs. 4.7%). No significant differences were found between the groups with respect to the time from admission to surgery.
Conclusion
The occurrence of PJI after hip joint fractures treated with hemiarthroplasty in aged patients is associated with a significant increase in mortality. Risk factors include a longer surgery time, diabetes, intraoperative complications, postoperative bleeding and wound healing disorders. Surgical treatment within the first 24 h should be aimed for but not at the expense of adequate patient preparation or neglecting the patient’s individual risk factors.
Zusammenfassung
Hintergrund
Die Hemiarthroplastik ist eine etablierte Behandlungsmethode bei einem Oberschenkelhalsbruch (Schenkelhalsfraktur, SHF) im hohen Alter, jedoch versterben 20–30 % der Patienten innerhalb eines Jahres nach der Operation. Periprothetische Gelenkinfektionen (PGI) stellen eine der schwersten Komplikationen dar und sind mit einer hohen Mortalitätsrate assoziiert. In dieser retrospektiven Studie zu Patienten fortgeschrittenen Alters mit SFH, die mit einer Hemiarthroplastik versorgt wurden, wurde die Inzidenz einer PGI hinsichtlich des Einflusses der Verzögerung der operativen Versorgung sowie des Operationszeitpunkts evaluiert.
Patienten und Methoden
Die Daten von Patienten mit SHF, die diesem Krankenhaus zwischen Januar 2012 und Dezember 2014 zugewiesenen worden waren, wurden ausgewertet. Demographische Daten, Operationszeitpunkt, intraoperative Komplikationen, PGI und andere allgemeine Komplikationen, Hospitalisationsdauer und Mortalität wurden erfasst.
Ergebnisse
In diese Studie wurden 178 Patienten in das Follow-up eingeschlossen (114 Frauen und 64 Männer). Das mittlere Alter der Patienten betrug 83 Jahre (Range: 55–105 Jahre). Die PGI-Rate lag bei 3,9 % (7/178), und die Mortalität bei 5,6 % (10/178). Patienten mit PGI nach Hemiarthroplastik hatten einen signifikant längeren Krankenhausaufenthalt (17 vs. 10 Tage; p < 0,001) und eine höhere Mortalitätsrate (28 % vs. 4,7 %). Es wurde keine signifikanten Unterschiede zwischen den Gruppen hinsichtlich der Zeit von der Einweisung bis zur Operation festgestellt.
Schlussfolgerung
Das Auftreten einer PGI nach Hüftgelenkfrakturen bei älteren Patienten, die mit einer Hemiarthroplastik versorgt wurden, ist mit einer signifikant höheren Mortalität assoziiert. Risikofaktoren sind eine längere Operationszeit, Diabetes, intraoperative Komplikationen, postoperative Blutungen und Wundheilungsstörungen. Eine operative Versorgung innerhalb der ersten 24 h sollte angestrebt werden, allerdings nicht auf Kosten einer adäquaten Vorbereitung des Patienten und unter Beachtung der individuellen Risikofaktoren.
Similar content being viewed by others
Abbreviations
- AWMF:
-
Association of the Scientific Medical Societies of Germany
- CI:
-
Confidence interval
- DGU:
-
German Society of Trauma Surgery
- FNF:
-
Femoral neck fractures
- ICMPJI:
-
International consensus meeting on periprosthetic joint infection
- ÖGU:
-
Austrian Society of Trauma Surgery
- PJI:
-
Periprosthetic joint infections
- RR:
-
Relative risk
- SOP:
-
Standard operating procedures
References
Beringer TR, Crawford VL, Brown JG (1996) Audit of surgical delay in relationship to outcome after proximal femoral fracture. Ulster Med J 65(1):32–38
Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P, Obremskey W, Koval KJ, Nork S, Sprague S, Schemitsch EH, Guyatt GH (2003) Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am 85-A(9):1673–1681
Bhandari M, Devereaux PJ, Tornetta P, Swiontkowski MF, Berry DJ, Haidukewych G, Schemitsch EH, Hanson BP, Koval K, Dirschl D, Leece P, Keel M, Petrisor B, Heetveld M, Guyatt GH (2005) Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am 87(9):2122–2130. https://doi.org/10.2106/JBJS.E.00535
Bonnaire F, Lein T, Hohaus T, Weber A (2005) Prosthetic care of proximal femur fractures. Unfallchirurg 108(5):387–399. https://doi.org/10.1007/s00113-005-0942-z (quiz 400)
Bonnaire F, Weber A et al (2015) S2e-Leitlinie 012/001: Schenkelhalsfraktur des Erwachsenen. http://www.awmf.org/leitlinien/detail/ll/012-001.html. Accessed: 9 Oct 2018
Buecking B, Eschbach D, Bliemel C, Knobe M, Aigner R, Ruchholtz S (2017) Endoprostheses in geriatric traumatology. Orthopade 46(1):48–53. https://doi.org/10.1007/s00132-016-3369-z
Chen AF, Kheir MM, Greenbaum JM, Restrepo C, Maltenfort MG, Parvizi J (2017) Surgical case order has an effect on the risk of subsequent periprosthetic joint infection. J Arthroplasty. https://doi.org/10.1016/j.arth.2017.02.029
Edwards C, Counsell A, Boulton C, Moran CG (2008) Early infection after hip fracture surgery: risk factors, costs and outcome. J Bone Joint Surg Br 90(6):770–777. https://doi.org/10.1302/0301-620X.90B6.20194
Frihagen F, Nordsletten L, Madsen JE (2007) Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ 335(7632):1251–1254. https://doi.org/10.1136/bmj.39399.456551.25
Garden RS (1964) Stability and union in subcapital fractures of the femur. J Bone Joint Surg Br 46:630–647
Harrison T, Robinson P, Cook A, Parker MJ (2012) Factors affecting the incidence of deep wound infection after hip fracture surgery. J Bone Joint Surg Br 94(2):237–240. https://doi.org/10.1302/0301-620X.94B1.27683
de Jong L, Klem TMAL, Kuijper TM, Roukema GR (2017) Factors affecting the rate of surgical site infection in patients after hemiarthroplasty of the hip following a fracture of the neck of the femur. Bone Joint J 99-B(8):1088–1094. https://doi.org/10.1302/0301-620X.99B8.BJJ-2016-1119.R1
Keating JF, Grant A, Masson M, Scott NW, Forbes JF (2005) Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technol Assess. https://doi.org/10.3310/hta9410
Knobe M, Siebert CH (2014) Hip fractures in the elderly. Osteosynthesis versus joint replacement. Orthopade 43(4):314–324. https://doi.org/10.1007/s00132-014-2265-7
Lichtblau S (2002) Treatment of hip fractures in the elderly—the decision process. Mt Sinai J Med 69(4):250–260
Lin Z‑Z, Wang J‑J, Chung C‑R, Huang P‑C, Su B‑A, Cheng K‑C, Chio C‑C, Chien C‑C (2014) Epidemiology and mortality of hip fracture among patients on dialysis: Taiwan National Cohort Study. Bone 64:235–239. https://doi.org/10.1016/j.bone.2014.04.017
Lohmann R, Frerichmann U, Stockle U, Riegel T, Raschke MJ (2007) Proximal femoral fractures in the elderly. Analysis of data from health insurance providers on more than 23 million insured persons—part 1. Unfallchirurg 110(7):603–609. https://doi.org/10.1007/s00113-007-1257-z
Mellner C, Eisler T, Knutsson B, Mukka S (2017) Early periprosthetic joint infection and debridement, antibiotics and implant retention in arthroplasty for femoral neck fracture. Hip Int. https://doi.org/10.5301/hipint.5000467
Parker MJ, Gurusamy K (2005) Modern methods of treating hip fractures. Disabil Rehabil 27(18–19):1045–1051
Pourabbas B, Emami MJ, Vosoughi AR, Namazi H (2016) Does mobility of the elderly with hip fractures improve at one year following surgery? A 5‑year prospective survey. Ortop Traumatol Rehabil 18(4):311–316. https://doi.org/10.5604/15093492.1220822
Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R (2005) Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br 87(6):844–850. https://doi.org/10.1302/0301-620X.87B6.15121
Sharma V, Awasthi B, Kumar K, Kohli N, Katoch P (2016) Outcome analysis of hemiarthroplasty vs. total hip replacement in displaced femoral neck fractures in the elderly. J Clin Diagn Res 10(5):RC11–RC13. https://doi.org/10.7860/JCDR/2016/18638.7877
Simon P, Gouin F, Veillard D, Laffargue P, Ehlinger M, Bel J‑C, Lopez R, Beaudet P, Luickx F, Molina V, Pidhorz L‑E, Bigorre N, Rochwerger A, Azam F, Louis M‑L, Cottias P, Hamonic S, Vogt F, Cambas P‑M, Tabutin J, Bonnevialle P, Lecoq M, Court C, Sitbon P, Lacoste S, Gagey O, Dujardin F, Gilleron M, Brzakala V, Roussignol X (2008) Femoral neck fractures in patients over 50 years old. Rev Chir Orthop Reparatrice Appar Mot 94(Suppl 6):S108–S132. https://doi.org/10.1016/j.rco.2008.06.006
Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, Bhandari M (2010) Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 182(15):1609–1616. https://doi.org/10.1503/cmaj.092220
Smektala R, Endres HG, Dasch B, Maier C, Trampisch HJ, Bonnaire F, Pientka L (2008) The effect of time-to-surgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskelet Disord 9:171. https://doi.org/10.1186/1471-2474-9-171
Templeman D, Baumgaertner MR, Leighton RK, Lindsey RW, Moed BR (2005) Reducing complications in the surgical treatment of intertrochanteric fractures. Instr Course Lect 54:409–415
Tran T, Delluc A, de Wit C, Petrcich W, Le Gal G, Carrier M (2015) The impact of oral anticoagulation on time to surgery in patients hospitalized with hip fracture. Thromb Res 136(5):962–965. https://doi.org/10.1016/j.thromres.2015.09.017
Westberg M, Snorrason F, Frihagen F (2013) Preoperative waiting time increased the risk of periprosthetic infection in patients with femoral neck fracture. Acta Orthop 84(2):124–129. https://doi.org/10.3109/17453674.2013.775044
Yoo J‑H, Kim K‑T, Kim T‑Y, Hwang J‑H, Chang J‑D (2017) Postoperative fever after hemiarthroplasty in elderly patients over 70 years of age with displaced femoral neck fracture: necessity of routine workup? Injury 48(2):441–446. https://doi.org/10.1016/j.injury.2016.12.013
Youssef B, Pavlou G, Tsiridis E (2014) Philadelphia 2013. International consensus meeting on periprosthetic joint infection. Hip Int 24(1):3–4. https://doi.org/10.5301/hipint.5000127
Zajonz D, Wuthe L, Tiepolt S, Brandmeier P, Prietzel T, von Salis-Soglio GF, Roth A, Josten C, Heyde C‑E, Ghanem M (2015) Diagnostic work-up strategy for periprosthetic joint infections after total hip and knee arthroplasty: a 12-year experience on 320 consecutive cases. Patient Saf Surg 9:20. https://doi.org/10.1186/s13037-015-0071-8
Zajonz D, Wuthe L, Rodloff AC, Prietzel T, von Salis-Soglio GF, Roth A, Heyde C‑E, Josten C, Ghanem M (2016) Infections of hip and knee endoprostheses. Spectrum of pathogens and the role of multiresistant bacteria. Chirurg 87(4):332–339. https://doi.org/10.1007/s00104-015-0126-5
Zajonz D, Brand A, Lycke C, Özkurtul O, Theopold J, Spiegl UJA, Roth A, Josten C, Fakler JKM (2018) Risk factors for early infection following hemiarthroplasty in elderly patients with a femoral neck fracture. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-018-0909-8
Zeltzer J, Mitchell RJ, Toson B, Harris IA, Close J (2014) Determinants of time to surgery for patients with hip fracture. ANZ J Surg 84(9):633–638. https://doi.org/10.1111/ans.12671
Acknowledgements
The authors thank the participating patients and the clinicians in the research network of the University of Leipzig.
Author contributions
C. Josten and A. Roth initiated the work. J. Behrens performed the data analysis. D. Zajonz and J. Behrens wrote the manuscript. A. G. Brand and A. Höch were significantly involved in the production of the figures and tables as well as the statistical analysis. D. Zajonz contributed to designing the statistical analysis. All authors were involved in the design of the study, interpretation of data, revision of the manuscript and all read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Zajonz, J. Behrens, A.G. Brand, A. Höch, J.K. M. Fakler, A. Roth, C. Josten and M. Ghanem declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors. All procedures reported in this article were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All participants gave written, informed consent within the scope of the treatment contract. The study was approved by the university ethics committee (number: 171-16/ek25042016).
Additional information
The authors D. Zajonz and J. Behrens contributed equally to the manuscript.
M. Ghanem and C. Josten are joint senior authors.
Availability of data and materials
The data and material are stored in the archive of the University of Leipzig within the framework of the legal provisions (data protection). They are available from the corresponding author on reasonable request.
Rights and permissions
About this article
Cite this article
Zajonz, D., Behrens, J., Brand, A.G. et al. Femoral neck fractures in old age treated with hemiarthroplasty. Orthopäde 48, 224–231 (2019). https://doi.org/10.1007/s00132-018-03664-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-018-03664-8