Abstract
Purpose
The objectives of this review were to understand the prevalence of cannabis use and how cannabis is associated with transition to psychosis, symptoms, cognition, trauma and family history in clinical high risk (CHR) for psychosis individuals.
Method
A systematic literature review was conducted to find studies that examined cannabis use in CHR individuals, with no limitations on the geographical area, and included publications up to November 2018. Studies were screened for inclusion based on detailed criteria, and data were extracted on cannabis use and associated outcomes. A quantitative synthesis by meta-analysis was performed where appropriate, otherwise, a qualitative synthesis was conducted.
Results
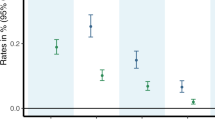
Overall, 36 studies met inclusion criteria with an average age of 20.1 years and 58.4% males. Prevalence of lifetime cannabis use was 48.7%, whereas current cannabis use was 25.8% and the prevalence of cannabis use disorder/abuse or dependence was 14.9% across the studies. All cannabis use results had statistically significant heterogeneity ranging from 75.7 to 92.8%. The most commonly reported association with cannabis use was transition to psychosis, although the pooled relative risk (RR) was not statistically significant (RR = 1.11, 95% confidence interval = 0.89–1.37). For all other outcomes including symptoms, cognition, trauma, and family history, the evidence was limited, and therefore, the results were synthesized qualitatively.
Conclusion
Almost half of CHR individuals have ever used cannabis. However, cannabis use has not been thoroughly researched regarding frequency and dose of use, and how other factors, such as symptoms, are associated with cannabis in CHR individuals.




Similar content being viewed by others
References
United Nations Office on Drugs and Crime (2019) World Drug Report 2019: 35 million people worldwide suffer from drug use disorders while only 1 in 7 people receive treatment
Hall W, Degenhardt L (2009) Adverse health effects of non-medical cannabis use. Lancet 374(9698):1383–1391. https://doi.org/10.1016/s0140-6736(09)61037-0
Lowe DJE, Sasiadek JD, Coles AS, George TP (2019) Cannabis and mental illness: a review. Eur Arch Psychiatry Clin Neurosci 269(1):107–120. https://doi.org/10.1007/s00406-018-0970-7
Leyton M (2019) Cannabis legalization: did we make a mistake? Update 2019. J Psychiatry Neurosci 44(5):291–293. https://doi.org/10.1503/jpn.190136
Arseneault L, Cannon M, Witton J, Murray RM (2004) Causal association between cannabis and psychosis: examination of the evidence. Br J Psychiatry 184:110–117. https://doi.org/10.1192/bjp.184.2.110
Ksir C, Hart CL (2016) Cannabis and psychosis: a critical overview of the relationship. Curr Psychiatry Rep 18(2):12. https://doi.org/10.1007/s11920-015-0657-y
Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques TR, Handley R, Luzi S, Russo M, Paparelli A, Butt A, Stilo SA, Wiffen B, Powell J, Murray RM (2009) High-potency cannabis and the risk of psychosis. Br J Psychiatry 195(6):488–491. https://doi.org/10.1192/bjp.bp.109.064220
Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E (2016) Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull 42(5):1262–1269. https://doi.org/10.1093/schbul/sbw003
Fusar-Poli P (2017) The clinical high-risk state for psychosis (CHR-P), version II. Schizophr Bull 43(1):44–47. https://doi.org/10.1093/schbul/sbw158
Addington J, Case N, Saleem MM, Auther AM, Cornblatt BA, Cadenhead KS (2014) Substance use in clinical high risk for psychosis: a review of the literature. Early Interv Psychiatry 8(2):104–112. https://doi.org/10.1111/eip.12100
Carney R, Cotter J, Firth J, Bradshaw T, Yung AR (2017) Cannabis use and symptom severity in individuals at ultra high risk for psychosis: a meta-analysis. Acta Psychiatr Scand 136(1):5–15. https://doi.org/10.1111/acps.12699
Kraan T, Velthorst E, Koenders L, Zwaart K, Ising HK, van den Berg D, de Haan L, van der Gaag M (2016) Cannabis use and transition to psychosis in individuals at ultra-high risk: review and meta-analysis. Psychol Med 46(4):673–681. https://doi.org/10.1017/s0033291715002329
Verweij KJ, Abdellaoui A, Nivard MG, Sainz Cort A, Ligthart L, Draisma HH, Minica CC, Gillespie NA, Willemsen G, Hottenga JJ, Boomsma DI, Vink JM (2017) Short communication: genetic association between schizophrenia and cannabis use. Drug Alcohol Depend 171:117–121. https://doi.org/10.1016/j.drugalcdep.2016.09.022
Henquet C, Di Forti M, Morrison P, Kuepper R, Murray RM (2008) Gene-environment interplay between cannabis and psychosis. Schizophr Bull 34(6):1111–1121. https://doi.org/10.1093/schbul/sbn108
O’Donoghue B, McHugh M, Nelson B, McGorry P (2018) Effects of cannabis use in those at ultra-high risk for psychosis. The complex connection between cannabis and schizophrenia. Elsevier, New York, pp 167–181
Ortiz-Medina MB, Perea M, Torales J, Ventriglio A, Vitrani G, Aguilar L, Roncero C (2018) Cannabis consumption and psychosis or schizophrenia development. Int J Soc Psychiatry 64(7):690–704. https://doi.org/10.1177/0020764018801690
Freeman M, Tukey J (1950) Transformations related to the angular and the square root. Ann Math Stat 21:607–611
Higgins J, Thompson S, Deeks J, Altman D (2003) Measuring inconsistency in meta-analyses. Br Med J 327(7414):557
Amminger GP, Schafer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, Mackinnon A, McGorry PD, Berger GE (2010) Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry 67(2):146–154. https://doi.org/10.1001/archgenpsychiatry.2009.192
Auther AM, McLaughlin D, Carrion RE, Nagachandran P, Correll CU, Cornblatt BA (2012) Prospective study of cannabis use in adolescents at clinical high risk for psychosis: impact on conversion to psychosis and functional outcome. Psychol Med 42(12):2485–2497. https://doi.org/10.1017/s0033291712000803
Barglow J, Dole T, Birnbaum M (2013) Effectiveness of a community-based early intervention program for psychosis: baseline characteristics and 3-month follow-up. Eur Arch Psychiatry Clin Neurosci 1:S65. https://doi.org/10.1007/s00406-013-0433-0
Bechdolf A, Muller H, Stutzer H, Wagner M, Maier W, Lautenschlager M, Heinz A, de Millas W, Janssen B, Gaebel W, Michel TM, Schneider F, Lambert M, Naber D, Brune M, Kruger-Ozgurdal S, Wobrock T, Riedel M, Klosterkotter J (2011) Rationale and baseline characteristics of PREVENT: a second-generation intervention trial in subjects at-risk (prodromal) of developing first-episode psychosis evaluating cognitive behavior therapy, aripiprazole, and placebo for the prevention of psychosis. Schizophr Bull 37(Suppl 2):S111–S121. https://doi.org/10.1093/schbul/sbr083
Bloemen OJ, de Koning MB, Schmitz N, Nieman DH, Becker HE, de Haan L, Dingemans P, Linszen DH, van Amelsvoort TA (2010) White-matter markers for psychosis in a prospective ultra-high-risk cohort. Psychol Med 40(8):1297–1304. https://doi.org/10.1017/s0033291709991711
Brucato G, Masucci MD, Arndt LY, Ben-David S, Colibazzi T, Corcoran CM, Crumbley AH, Crump FM, Gill KE, Kimhy D, Lister A, Schobel SA, Yang LH, Lieberman JA, Girgis RR (2017) Baseline demographics, clinical features and predictors of conversion among 200 individuals in a longitudinal prospective psychosis-risk cohort. Psychol Med 47(11):1923–1935. https://doi.org/10.1017/s0033291717000319
Buchy L, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Heinssen R, Bearden CE, Mathalon D, Addington J (2015) Substance use in individuals at clinical high risk of psychosis. Psychol Med 45(11):2275–2284. https://doi.org/10.1017/s0033291715000227
Buchy L, Perkins D, Woods SW, Liu L, Addington J (2014) Impact of substance use on conversion to psychosis in youth at clinical high risk of psychosis. Schizophr Res 156(2–3):277–280. https://doi.org/10.1016/j.schres.2014.04.021
Bugra H, Studerus E, Rapp C, Tamagni C, Aston J, Borgwardt S, Riecher-Rossler A (2013) Cannabis use and cognitive functions in at-risk mental state and first episode psychosis. Psychopharmacology 230(2):299–308. https://doi.org/10.1007/s00213-013-3157-y
Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, Heinssen R (2008) Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry 65(1):28–37. https://doi.org/10.1001/archgenpsychiatry.2007.3
Carney R, Yung AR, Amminger GP, Bradshaw T, Glozier N, Hermens DF, Hickie IB, Killackey E, McGorry P, Pantelis C, Wood SJ, Purcell R (2017) Substance use in youth at risk for psychosis. Schizophr Res 181:23–29. https://doi.org/10.1016/j.schres.2016.08.026
Carol EE, Mittal VA (2014) Self-reported cannabis use is inconsistent with the results from drug-screening in youth at ultra high-risk for psychosis in Colorado. Schizophr Res 157(1–3):317–318. https://doi.org/10.1016/j.schres.2014.05.032
Dragt S, Nieman DH, Becker HE, van de Fliert R, Dingemans PM, de Haan L, van Amelsvoort TA, Linszen DH, Dragt S, Nieman DH, Becker HE, van de Fliert R, Dingemans PM, de Haan L, van Amelsvoort TA, Linszen DH (2010) Age of onset of cannabis use is associated with age of onset of high-risk symptoms for psychosis. Can J Psychiatry 55(3):165–171
Dragt S, Nieman DH, Schultze-Lutter F, van der Meer F, Becker H, de Haan L, Dingemans PM, Birchwood M, Patterson P, Salokangas RK, Heinimaa M, Heinz A, Juckel G, Graf von Reventlow H, French P, Stevens H, Ruhrmann S, Klosterkotter J, Linszen DH (2012) Cannabis use and age at onset of symptoms in subjects at clinical high risk for psychosis. Acta Psychiatr Scand 125(1):45–53. https://doi.org/10.1111/j.1600-0447.2011.01763.x
Gawlowska M, Rabe-Jablonska J, Pawelczyk T, Pawelczyk A (2010) Assessment of independent risk factors of conversion into psychosis in the ultra-high risk state group of patients (Ocena niezaleznych czynnikow ryzyka konwersji w psychoze w grupie osob z wysokim ryzykiem rozwoju zaburzen psychotycznych). Psychiatr Psychol Klin 10(4):254–266
Gill KE, Poe L, Azimov N, Ben-David S, Vadhan NP, Girgis R, Moore H, Cressman V, Corcoran CM (2015) Reasons for cannabis use among youths at ultra high risk for psychosis. Early Interv Psychiatry 9(3):207–210. https://doi.org/10.1111/eip.12112
Hagenmuller F, Heekeren K, Meier M, Theodoridou A, Walitza S, Haker H, Rossler W, Kawohl W (2016) The Loudness Dependence of Auditory Evoked Potentials (LDAEP) in individuals at risk for developing bipolar disorders and schizophrenia. Clin Neurophysiol 127(2):1342–1350. https://doi.org/10.1016/j.clinph.2015.10.050
Kristensen K, Cadenhead KS (2007) Cannabis abuse and risk for psychosis in a prodromal sample. Psychiatry Res 151(1–2):151–154. https://doi.org/10.1016/j.psychres.2006.10.001
Machielsen M, van der Sluis S, de Haan L (2010) Cannabis use in patients with a first psychotic episode and subjects at ultra high risk of psychosis: impact on psychotic- and pre-psychotic symptoms. Aust N Z J Psychiatry 44(8):721–728. https://doi.org/10.3109/00048671003689710
Magaud E, Kebir O, Gut A, Willard D, Chauchot F, Olie JP, Kazes M, Krebs MO (2010) Altered semantic but not phonological verbal fluency in young help-seeking individuals with ultra high risk of psychosis. Schizophr Res 123(1):53–58. https://doi.org/10.1016/j.schres.2010.05.005
Marshall C, Addington J, Epstein I, Liu L, Deighton S, Zipursky RB (2012) Treating young individuals at clinical high risk for psychosis. Early Interv Psychiatry 6(1):60–68. https://doi.org/10.1111/j.1751-7893.2011.00299.x
McHugh M, McGorry P, Yung A, Lin A, Wood S, Hartmann J, Nelson B (2017) Cannabis-induced attenuated psychotic symptoms: implications for prognosis in young people at ultra-high risk for psychosis. Psychol Med 47(4):616–626. https://doi.org/10.1017/S0033291716002671
Mizrahi R, Kenk M, Suridjan I, Boileau I, George TP, McKenzie K, Wilson AA, Houle S, Rusjan P (2014) Stress-induced dopamine response in subjects at clinical high risk for schizophrenia with and without concurrent cannabis use. Neuropsychopharmacology 39(6):1479–1489. https://doi.org/10.1038/npp.2013.347
Nieman DH, Dragt S, van Duin EDA, Denneman N, Overbeek JM, de Haan L, Rietdijk J, Ising HK, Klaassen RMC, van Amelsvoort T, Wunderink L, van der Gaag M, Linszen DH (2016) COMT Val(158)Met genotype and cannabis use in people with an at Risk Mental State for psychosis: exploring Gene × Environment interactions. Schizophr Res 174(1–3):24–28. https://doi.org/10.1016/j.schres.2016.03.015
Pardo M, Tor J, Munoz D, Rodriguez M, Sanchez B, De La Serna E, Matali JL, Sanchez-Gistau V, Carulla M, Baeza I, Dolz M (2014) Cannabis use in a sample of subjects at risk for developing psychosis. Schizophr Res 1:S244–S245
Pruessner M, Iyer SN, Faridi K, Joober R, Malla AK (2011) Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophr Res 129(1):29–35. https://doi.org/10.1016/j.schres.2011.03.022
Russo DA, Stochl J, Painter M, Jones PB, Perez J (2014) Substance use in people at clinical high-risk for psychosis. BMC Psychiatry 14:361. https://doi.org/10.1186/s12888-014-0361-1
Serpa M, Loch AA, Chianca C, Freitas E, Andrade JC, Alves TM, Hortencio L, Van De Bilt MT, Gattaz W, Rossler W (2018) Illicit drugs use and ultra-high risk (UHR) for psychosis status in a Latin-American sample. Schizophr Bull 44(Supplement 1):S195. https://doi.org/10.1093/schbul/sby016.479
Simon AE, Umbricht D (2010) High remission rates from an initial ultra-high risk state for psychosis. Schizophr Res 116(2–3):168–172. https://doi.org/10.1016/j.schres.2009.10.001
Stain HJ, Bucci S, Baker AL, Carr V, Emsley R, Halpin S, Lewin T, Schall U, Clarke V, Crittenden K, Startup M (2016) A randomised controlled trial of cognitive behaviour therapy versus non-directive reflective listening for young people at ultra high risk of developing psychosis: the detection and evaluation of psychological therapy (DEPTh) trial. Schizophr Res 176(2–3):212–219. https://doi.org/10.1016/j.schres.2016.08.008
Stojanovic A, Martorell L, Montalvo I, Ortega L, Monseny R, Vilella E, Labad J (2014) Increased serum interleukin-6 levels in early stages of psychosis: associations with at-risk mental states and the severity of psychotic symptoms. Psychoneuroendocrinology 41:23–32. https://doi.org/10.1016/j.psyneuen.2013.12.005
Valmaggia L, Day F, Jones C, Bissoli S, Pugh C, Hall D, Bhattacharyya S, Howes O, Stone J, Fusar-Poli P, Byrne M, McGuire P (2014) Cannabis use and transition to psychosis in people at ultra-high risk. Psychol Med 44(12):2503–2512. https://doi.org/10.1017/S0033291714000117
Van Tricht MJ, Harmsen EC, Koelman JHTM, Bour LJ, van Amelsvoort TA, Linszen DH, de Haan L, Nieman DH (2013) Effects of cannabis use on event related potentials in subjects at ultra high risk for psychosis and healthy controls. Int J Psychophysiol 88(2):149–156. https://doi.org/10.1016/j.ijpsycho.2013.03.012
Ward PB, Logan S, Scully A, Mathersul D, Loneragan C, Curtis J, Stain HJ, Michie P, Todd J, Schall U, Landon R, Atkinson R (2014) Age of onset and prevalence of substance use in help-seeking ultra-high risk youth are linked to current psychopathology. Schizophr Res 1:S380
Winton-Brown T, Kumari V, Windler F, Moscoso A, Stone J, Kapur S, McGuire P (2014) Sensory gating, cannabis use and the risk of psychosis. Early Interv Psychiatry 1:60. https://doi.org/10.1111/eip.12186
Woods SW, Breier A, Zipursky RB, Perkins DO, Addington J, Miller TJ, Hawkins KA, Marquez E, Lindborg SR, Tohen M, McGlashan TH (2003) Randomized trial of olanzapine versus placebo in the symptomatic acute treatment of the schizophrenic prodrome. Biol Psychiatry 54(4):453–464. https://doi.org/10.1016/s0006-3223(03)00321-4
Addington J, Piskulic D, Liu L, Lockwood J, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Bearden CE, Mathalon DH, Woods SW (2017) Comorbid diagnoses for youth at clinical high risk of psychosis. Schizophr Res 190:90–95. https://doi.org/10.1016/j.schres.2017.03.043
Amminger GP, Schafer MR, Schlogelhofer M, Klier CM, McGorry PD (2015) Longer-term outcome in the prevention of psychotic disorders by the Vienna omega-3 study. Nat Commun 6:7934. https://doi.org/10.1038/ncomms8934
Auther AM, Cadenhead KS, Carrion RE, Addington J, Bearden CE, Cannon TD, McGlashan TH, Perkins DO, Seidman L, Tsuang M, Walker EF, Woods SW, Cornblatt BA (2015) Alcohol confounds relationship between cannabis misuse and psychosis conversion in a high-risk sample. Acta Psychiatr Scand 132(1):60–68. https://doi.org/10.1111/acps.12382
Corcoran CM, Kimhy D, Stanford A, Khan S, Walsh J, Thompson J, Schobel S, Harkavy-Friedman J, Goetz R, Colibazzi T, Cressman V, Malaspina D (2008) Temporal association of cannabis use with symptoms in individuals at clinical high risk for psychosis. Schizophr Res 106(2–3):286–293. https://doi.org/10.1016/j.schres.2008.08.008
Georgopoulos G, Stowkowy J, Liu L, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Bearden CE, Mathalon DH, Addington J (2017) The role of a family history of psychosis for youth at clinical high risk of psychosis. Early Interv Psychiatry. https://doi.org/10.1111/eip.12471
Korver N, Nieman DH, Becker HE, van de Fliert J, Dingemans PH, de Haan L, Spiering M, Schmitz N, Linszen DH (2010) Symptomatology and neuropsychological functioning in cannabis using subjects at ultra-high risk for developing psychosis and healthy controls. Aust N Z J Psychiatry 44(3):230–236. https://doi.org/10.3109/00048670903487118
Lin A, Nelson B, Wood S, Beavan A, McGorry P, Yung A (2012) Outcomes of non-transitioned cases in a sample at ultra-high risk for psychosis: a medium to long-term follow-up study. Early Interv Psychiatry 6(suppl 1):3. https://doi.org/10.1111/j.1751-7893.2012.00392.x
Pardo M, Sintes A, Puig O, Espelt C, De La Serna E, Rodriguez M, Espadas M, Carulla M, Baeza I, Dolz M (2014) Cannabis use and neuropsychological functioning in ultra-high risk for developing psychosis in child and adolescent patients and healthy controls. Schizophr Res 1:S146
Phillips LJ, Curry C, Yung AR, Yuen HP, Adlard S, McGorry PD (2002) Cannabis use is not associated with the development of psychosis in an ‘ultra’ high-risk group. Aust N Z J Psychiatry 36(6):800–806. https://doi.org/10.1046/j.1440-1614.2002.01089.x
Stain HJ, Halpin SA, Baker AL, Startup M, Carr VJ, Schall U, Crittenden K, Clark V, Lewin TJ, Bucci S (2018) Impact of rurality and substance use on young people at ultra high risk for psychosis. Early Interv Psychiatry 12(6):1173–1180. https://doi.org/10.1111/eip.12437
Stowkowy J, Addington J (2013) Predictors of developing a psychosis risk syndrome in youth at family high risk of developing psychosis. Schizophr Bull 1:S305. https://doi.org/10.1093/schbul/sbt011
Ayonrinde OA (2019) Cannabis and psychosis: revisiting a nineteenth century study of ‘Indian Hemp and Insanity’ in Colonial British India. Psychol Med. https://doi.org/10.1017/s0033291719001077
Hathaway AD, Comeau NC, Erickson PG (2011) Cannabis normalization and stigma: contemporary practices of moral regulation. Criminol Crim Justice 11(5):451–469. https://doi.org/10.1177/1748895811415345
Parker H, Williams L, Aldridge J (2002) The normalization of ‘sensible’ recreational drug use: further evidence from the North West England longitudinal study. Sociology 36(4):941–964. https://doi.org/10.1177/003803850203600408
Potvin S, Stip E, Roy JY (2003) Schizophrenia and addiction: an evaluation of the self-medication hypothesis. Encephale 29(3 Pt 1):193–203
Acknowledgements
This work was supported by NIH Grant RO1MH105178 awarded to Dr. Jean Addington.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The manuscript does not contain clinical studies or patient data.
Rights and permissions
About this article
Cite this article
Farris, M.S., Shakeel, M.K. & Addington, J. Cannabis use in individuals at clinical high-risk for psychosis: a comprehensive review. Soc Psychiatry Psychiatr Epidemiol 55, 527–537 (2020). https://doi.org/10.1007/s00127-019-01810-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01810-x