Abstract
Purpose
Health care professionals, including pharmacists, have the potential to recognise and assist those at risk of suicide. The primary aim of this study was to assess the impact of utilising people with a lived experience of mental illness as simulated patients on final year pharmacy students’ attitudes toward and confidence in caring for people at risk of suicide after first receiving Mental Health First Aid (MHFA) training.
Methods
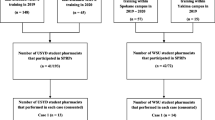
A parallel group repeated measures design was used. People with a lived experience of mental illness enacted patients experiencing a mental health crisis, including possible suicidal ideation. Following MHFA training, the first group directly participated in the simulation, the second group observed, and the final group had no exposure to the simulation. Validated surveys measuring student attitudes and confidence were conducted at three time points; pre and post MHFA, and then at 2–4 weeks follow-up.
Results
Full datasets of survey responses were received from 34/40 direct participants (85%), 104/146 observers (71%) and 50/66 comparison students (76%). Mean confidence scores significantly improved for all groups post MHFA training (p < 0.05). At follow-up, all 8 confidence items for the direct participant and observer group maintained significance from baseline to post intervention (p < 0.05). Mixed results in relation to attitudes towards suicide were evident at each time point and among each participant group.
Conclusions
Utilising people with a lived experience of mental illness as simulated patients has a positive effect on sustaining pharmacy student confidence in discussing suicidal behaviour post MHFA training. The inconsistency in attitudes towards suicide suggests that attitudes are complex in nature, involving multiple dynamic influences.

Similar content being viewed by others
References
Mathers C, Stevens G, Ma Fat D, Ho Wahyu J, Mahanani R (2014) WHO methods and data sources for country-level causes of death 2000–2012. World Health Organisation. http://www.who.int/healthinfo/global_burden_disease/GlobalCOD_method_2000_2012.pdf?ua=1. Accessed 29 October 2016
Australian Bureau of Statistics (2016) Causes of death, Australia, 2015. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/3303.0~2015~Main%20Features~Intentional%20self-harm:%20key%20characteristics~8. Accessed 29 October 2016
Sher L (2012) Teaching medical professionals and trainees about adolescent suicide prevention: five key problems. Int J Adolesc Med Health 24:121–123. https://doi.org/10.1515/ijamh.2012.018
Murphy AL, Gardner DM, Chen TF, O’Reilly C, Kutcher SP (2015) Community pharmacists and the assessment and management of suicide risk. Can Pharm J 148:171–175. https://doi.org/10.1177/1715163515587554
Murphy AL, Hillier K, Ataya R, Thabet P, Whelan AM, O’Reilly C, Gardner D (2017) A scoping review of community pharmacists and patients at risk of suicide. Can Pharm J 150:366–379. https://doi.org/10.1177/1715163517733482
Black E, Murphy AL, Gardner DM (2009) Community pharmacist services for people with mental illnesses: preferences, satisfaction, and stigma. Psychiatr Serv 60:1123–1127
O’Reilly CL, Wong E, Chen TF (2015) A feasibility study of community pharmacists performing depression screening services. Res Soc Adm Pharm 11:364–381. https://doi.org/10.1016/j.sapharm.2014.08.013
Kirschbaum M, Peterson G, Bridgman H (2016) Mental health first aid training needs of Australian community pharmacists. Curr Pharm Teach Learn 8:279–288. https://doi.org/10.1016/j.cptl.2016.02.015
Hawgood JL, Krysinska KE, Ide N, Leo DD (2008) Is suicide prevention properly taught in medical schools? Med Teach 30:287–295. https://doi.org/10.1080/01421590701753542
Jorm AF, Blewitt KA, Griffiths KM, Kitchener BA, Parslow RA (2005) Mental health first aid responses of the public: results from an Australian national survey. BMC Psychiatr 5:9. https://doi.org/10.1186/1471-244x-5-9
O’Reilly CL, Bell JS, Chen TF (2010) Pharmacists’ beliefs about treatments and outcomes of mental disorders: a mental health literacy survey. Austr N Z J Psychiatry 44:1089–1096. https://doi.org/10.3109/00048674.2010.512864
Jorm AF, Kitchener BA (2011) Noting a landmark achievement: mental health first aid training reaches 1% of Australian adults. Austr N Z J Psychiatry 45:808–813. https://doi.org/10.3109/00048674.2011.594785
O’Reilly CL, Bell JS, Kelly PJ, Chen TF (2011) Impact of mental health first aid training on pharmacy students’ knowledge, attitudes and self-reported behaviour: a controlled trial. Austr N Z J Psychiatry 45:549–557. https://doi.org/10.3109/00048674.2011.585454
El-Den S, Chen TF, Moles RJ, O’Reilly C (2017) Assessing mental health first aid skills using simulated patients. Am J Pharm Educ 82:6222. https://doi.org/10.5688/ajpe6222
Bond KS, Jorm AF, Kitchener BA, Reavley NJ (2015) Mental health first aid training for australian medical and nursing students: an evaluation study. BMC Psychol 3:11. https://doi.org/10.1186/s40359-015-0069-0
Kato TA, Suzuki Y, Sato R, Fujisawa D, Uehara K, Hashimoto N, Sawayama Y, Hayashi J, Kanba S, Otsuka K (2010) Development of 2-hour suicide intervention program among medical residents: first pilot trial. Psychiatr Clin Neurosci 64:531–540. https://doi.org/10.1111/j.1440-1819.2010.02114.x
O’Reilly CL, Bell JS, Chen TF (2010) Consumer-led mental health education for pharmacy students. Am J Pharm Educ 74:167
Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, Koschorke M, Shidhaye R, O’Reilly C, Henderson C (2016) Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet 387:1123–1132. https://doi.org/10.1016/S0140-6736(15)00298-6
Miller GE (1990) The assessment of clinical skills/competence/performance. Acad Med 65:63–67
Mental Health First Aid Australia (2016). https://mhfa.com.au. Accessed 29 October 2016
Renberg ES, Jacobsson L (2003) Development of a questionnaire on attitudes towards suicide (ATTS) and its application in a Swedish population. Suicide Life Threat Behav 33:52–64. https://doi.org/10.1521/suli.33.1.52.22784
Field AP (2009) Discovering statistics using SPSS, vol 3rd. SAGE, London
Pettigrew TF, Tropp LR (2006) A meta-analytic test of intergroup contact theory. J Pers Soc Psychol 90:751–783
Knaak S, Modgill G, Patten SB (2014) Key ingredients of anti-stigma programs for health care providers: a data synthesis of evaluative studies. Can J Psychiatry Revue Can de Psychiatrie 59:S19–S26
Bond KS, Jorm AF, Kitchener BA, Reavley NJ (2016) Mental health first aid training for australian financial counsellors: an evaluation study. Adv Mental Health 14:65. https://doi.org/10.1080/18387357.2015.1122704
Seale C (2009) Legalisation of euthanasia or physician-assisted suicide: survey of doctors’ attitudes. Palliat Med 23:205–212. https://doi.org/10.1177/0269216308102041
Hains C-AM, Hulbert-Williams NJ (2013) Attitudes toward euthanasia and physician-assisted suicide: a study of the multivariate effects of healthcare training, patient characteristics, religion and locus of control. J Med Ethics 39:713–716. https://doi.org/10.1136/medethics-2012-100729
Kopp SW (2009) The influence of death attitudes and knowledge of end of life options on attitudes toward physician-assisted suicide. OMEGA J Death Dying 58:299–311. https://doi.org/10.2190/OM.58.4.c
Nordstrand MA, Nordstrand SJ, Materstvedt LJ, Nortvedt P, Magelssen M (2013) Medical students’ attitudes towards legalisation of euthanasia and physician-assisted suicide. Tidsskrift For Den Norske Lægeforening Tidsskrift For Praktisk Medicin Ny Række 133:2359–2363. https://doi.org/10.4045/tidsskr.13.0439
Fairman N, Thomas LP, Whitmore S, Meier EA, Irwin SA (2014) What did I miss? A qualitative assessment of the impact of patient suicide on hospice clinical staff. J Palliat Med 17:832–836
Osafo J, Knizek B, Akotia C, Hjelmeland H (2012) Attitudes of psychologists and nurses toward suicide and suicide prevention in Ghana: a qualitative study. Int J Nurs Stud 49:691–700
Sun FK, Long A, Boore J (2007) The attitudes of casualty nurses in Taiwan to patients who have attempted suicide. J Clin Nurs 16:255–263. https://doi.org/10.1111/j.1365-2702.2005.01479.x
Bearman M, Nestel D (2014) Learning theories and simulated patient methodology. In: Simulated patient methodology. Wiley, New York, pp 31–38. https://doi.org/10.1002/9781118760673.ch5
Kalaniti K, Campbell DM (2015) Simulation-based medical education: Time for a pedagogical shift. Indian Pediatr 52:41–45. https://doi.org/10.1007/s13312-015-0565-6
Acknowledgements
The authors thank the study participants and are grateful to One Door Mental Health for their assistance in developing and implementing the mental health consumer-led patient scenarios.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Boukouvalas, E.A., El-Den, S., Chen, T.F. et al. Confidence and attitudes of pharmacy students towards suicidal crises: patient simulation using people with a lived experience. Soc Psychiatry Psychiatr Epidemiol 53, 1185–1195 (2018). https://doi.org/10.1007/s00127-018-1582-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-018-1582-2