Abstract
Introduction
Initial clinical observation of Somali patients seen at a busy inner-city community clinic (CUHCC) suggested that, in addition to the expected pictures of Posttraumatic Stress Disorder (PTSD) and depression previously seen in the clinic’s Southeast Asian refugee population from 1980 to 2000, there was an unusually high number of young Somali men presenting with acute psychotic disturbances.
Objectives
The aim of this study of health care utilization of Somali refugees (N = 600) seen in the mental health unit of the clinic from 2001 to 2009 was to investigate the major patterns of psychiatric disorders in this outpatient population and compare these findings with a cohort of non-Somali patients (N = 3,009) seen at the same outpatient clinic during the years 2007–2009. If the results supported the initial clinical observations that the rate of psychoses was higher among young Somali men than non-Somali men attending CUHCC clinic, then several areas of further research would recommend itself. First, since this study was not a study of prevalence of mental illness in the Somali community, the next step would be to undertake a study of community prevalence of mental illness among different age and gender cohorts. Second, further research should look into likely causative and contributory risk factors to explain the development of psychoses among Somali young men.
Methods
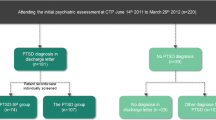
Somali and non-Somali patients were diagnosed according to DSM-IV-R criteria. Main outcome measures (diagnoses, age cohort, sex) were analyzed by Chi-square tests. Patterns of illness and adjustment varied significantly by age and gender cohorts, reflecting the relevance of age and gender at time of trauma on different trauma and loss experiences and cultural and religious shaping of subsequent adjustment and symptoms.
Results
The study confirmed that almost half of the Somali male patients are under age 30, 80% of whom presented with psychoses, compared with the rate of psychosis (13.7%) in the non-Somali control group of same-aged males at the clinic. The older male, and the majority of Somali female patients, show predominantly depressive and PTSD symptomatology.
Conclusions
War trauma experienced in childhood, early malnutrition from famines, head trauma, and excess Khat use in male adolescents provide partial explanations for the large number of young psychotic Somali men seen in the clinic from 2001 to 2009.
Similar content being viewed by others
References
Population Notes, Minnesota State Demographics Center, June 2004. http://www.demography.state.mn.us/PopNotes/EvaluatingEstimates.pdf. Accessed 23 December 2009
Lewis IM (2002) A modern history of the Somali, 4th edn. Ohio University Press, Athens
Besteman C (1999) Unraveling Somalia: race, violence and the legacy of slavery. University of Pennsylvania Press, Philadelphia
Feyissa AM, Kelly JP (2008) A review of the neuropharmacological properties of khat. Prog Neuropsychopharmacol Biol Psychiatry 32:1147–1166
Al-Motarreb A, Baker K, Broadley KJ (2002) Khat: pharmacological and medical aspects and its social use in Yemen. Phytother Res 16:403–413
Cox G, Rampes H (2003) Adverse effects of khat: a review. Adv Psychiatr Treat 9:456–463
Anthony C (2009) Africa’s displaced peoples: State-building realpolitik and stunted globalization. Harvard Int Rev 31(3):50–54
The 2009 HHS Poverty Guidelines. Federal Register Notice, 23 Jan 2009. http://aspe.hhs.gov/poverty/09poverty.shtml. Accessed 11 November 2009
Al-Saffar S, Borga P, Edman G, Hallstrom T (2003) The aetiology of posttraumatic stress disorder in four ethnic groups in outpatient psychiatry. Soc Psychiatry Psychiatr Epidemiol 38:456–462
Yeomans PD, Herbert JD, Forman EM (2008) Symptom comparison across multiple solicitation methods among Burundians with traumatic event histories. J Trauma Stress 21:231–234
Ichikawa M, Nakahara S, Wakai S (2006) Cross-cultural use of the predetermined scale cutoff points in refugee mental health research. Soc Psychiatry Psychiatr Epidemiol 41:248–250
Bhui K, Abdi A, Abdi M, Pereira S, Dualeh M, Robertson D, Sathyamoorthy G, Ismail H (2003) Traumatic events, migration characteristics and psychiatric symptoms among Somali refugees. Soc Psychiatry Psychiatr Epidemiol 38:35–43
Kroll J (2003) Posttraumatic symptoms and the complexity of responses to trauma. JAMA 290:667–670
Briggs L, Macleod AD (2006) Demoralisation—a useful conceptualization of non-specific psychological distress among refugees attending mental health services. Int J Soc Psychiatry 52:512–524
Scuglik DL, Alarcon RD, Lapeyre AC, Williams MD, Logan KM (2007) When the poetry no longer rhymes: mental health issues among Somali immigrants in the USA. Transcult Psychiatry 44:581–595
Kroll J, Habenicht M, Mackenzie T, Yang M, Chan S, Vang T, Nguyen T, Ly M, Phommasouvanh B, Nguyen H, Vang Y, Cabugao R (1989) Depression and post-traumatic stress disorder in Southeast Asian refugees. Am J Psychiatry 146:1592–1597
Ellis BH, MacDonald HZ, Lincoln AK, Cabral HJ (2008) Mental health of Somali adolescent refugees: the role of trauma, stress, and perceived discrimination. J Consult Clin Psychol 76:184–193
Odenwald M, Schauer M, Neuner F, Lingenfelder B, Horn R, Catani C, Klaschik C, Elbert T (2002) War trauma, Khat abuse and psychosis: mental health in the demobilization and reintegration program Somaliland. Final Report of the vivo mission 2 within the EC/GTZ, Sept–Nov. http://www.vivo.org. Accessed 27 August 2006
Bhui K, Warfa N (2007) Drug consumption in conflict zones in Somalia. PLoS Med 4(12):e354. doi:10.1371/journal.pmed.0040354
Odenwald M, Hinkle H, Schauer E, Neuner F, Schauer M, Elbert TR, Rockstroh B (2007) The consumption of Khat and other drugs in Somali combatants: a cross-sectional study. PLoS Med 4(12):e341. doi:10.1371/journal.pmed.0040341
Odenwald M, Hinkle H, Schauer E, Schauer M, Elbert TR, Neuner F, Rockstroh B (2009) Use of khat and posttraumatic stress disorder as risk factors for psychotic symptoms: a study of Somali combatants. Soc Sci Med 69:1040–1048
Bhui K, Craig T, Mohamud S, Warfa N, Standfeld SA, Thornicroft G, Curtis S, McCrone P (2006) Mental disorders among Somali refugees: developing culturally appropriate measures and assessing socio-cultural risk factors. Soc Psychiatry Psychiatr Epidemiol 41:400–408
Mavreas V, Bebbington P (1989) Does the act of immigration provoke psychiatric breakdown? A study of Greek Cypriote immigrants. Acta Psychiatrica Scand 80:469–473
Selten JP, Sijben N (1994) First admission rates for schizophrenia in immigrants to the Netherlands: the Dutch National Registrar. Soc Psychiatry Psychiatr Epidemiol 29:71–77
Cantor-Graae E, Pedersen CB, McNeil TF, Mortensen PB (2003) Migration as a risk factor for schizophrenia: a Danish population based cohort study. Br J Psychiatry 182:117–122
Leao TS, Sundquist J, Frank G, Johansson L-M, Johansson E-S, Sundquist K (2006) Incidence of schizophrenia or other psychoses in first-and second-generation immigrants, a national cohort study. J Nerv Ment Dis 194:27–33
Coid JW, Kirkbride JB, Barker D, Cowden F, Stamps R, Yang M, Jones PB (2008) Raised incidence rates of all psychoses among migrant groups. Arch Gen Psychiatry 65:1250–1258
Lataster T, Van Os J, Drukker M, Henquet C, Feron F, Gunther N, Myin-Germeys I (2006) Childhood victimization and developmental expression of non-clinical delusional ideation and hallucinatory experiences: victimization and non-clinical psychotic experiences. Social Psychiatry Psychiatr Epidemiol 41:423–428
Kilcommons AM, Morrison AP (2005) Relationships between trauma and psychosis: an exploration of cognitive and dissociative factors. Acta Psychiatr Scand 112:351–359
Shevlin M, Dorahy MJ, Adamson G (2007) Trauma and psychosis: an analysis of the National Comorbidity Study. Am J Psychiatry 164:166–169
Moore THM, Zammit S, Lingford-Hughes A, Barnes TRE, Jones PB, Burke M, Lewis G (2007) Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet 370:319–328
Degenhardt L, Hall W (2006) Is cannabis use a contributory cause of psychosis? Can J Psychiatry 51:556–565
Degenhardt L, Tennant C, Gilmour S, Schofield D, Nash L, Hall W, McKay D (2007) The temporal dynamics of relationships between cannabis, psychosis and depression among young adults with psychotic disorders: findings from a 10-month prospective study. Psychol Med 37:927–934
Henquet C, Krabbendam L, Spauwen J, Kaplan C, Lieb R, Wittchen H-U, van Os J (2005) Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. Br Med J 330:11–14
Schweinsburg AD, Brown SA, Tapert SF (2008) The influence of marijuana use on neurocognitive functioning in adolescents. Curr Drug Abuse Rev 1:99–111
Warfa N, Klein A, Bhui K, Leavey G, Craig T, Stansfeld A (2007) Khat use and mental illness: a critical review. Soc Sci Med 65:309–318
Odenwald M (2007) Chronic khat use and psychotic disorder: a review of the literature and future prospects. Sucht 53:9–22
Randall T (1993) Khat abuse fuels Somali conflict, drains economy. JAMA 269:12–13
Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, Gorman JM (1996) Schizophrenia after prenatal famine. Arch Gen Psychiatry 53:25–31
St. Clair D, Xu M, Wang P, Yu Y, Fang Y, Zhang F, Zheng X, Gu N, Feng G, Sham P, He L (2005) Rates of adult schizophrenia following prenatal exposure to the Chinese famine of 1959–61. JAMA 294:557–562
McClennan JM, Susser E, King M-C (2006) Maternal famine, de novo mutations, and schizophrenia. JAMA 296:582–584
Internal Displacement Monitoring Centre (iDMC): Somalia: Window of opportunity for addressing one of the world’s worst internal displacement crises. 10 January 2006, http://www.internal-displacement.org. Accessed 23 August 2006
Sargent J, Michael K (2005) The need for a digital aid framework in humanitarian relief. The 9th World Multi-Conference on Systematics, Cybernetics and Informatics, Orlando, FL, 10–13 July 2005. http://ro.uow.edu/infopapers/377. Accessed 26 August 2006
IRINnews: Somalia. All-out war catastrophic for southern Somalia––famine watchdog. 12 January 2007. http://www.IRINnews.org. Accessed 12 January 2007
Patman RG (1997) Disarming Somalia: the contrasting fortunes of US and Australian peacekeepers during UN intervention 1992–93. Afr Aff 96:509–533
Moore PS, Marfin AA, Quenemoen LE, Gessner BD, Ayub YS, Miller DS, Sullivan KM, Toole MJ (1993) Mortality rates in displaced and resident populations of central Somalia during 1992 famine. Lancet 341:935–938
Seal AJ, Creeke PI, Mirghani Z, Abdalla F, McBurney RP, Pratt LS, Brookes D, Ruth LJ, Marchand E (2005) Iron and vitamin A deficiency in long-term African refugees. J Nutr 135:808–813
Collins S, Myatt M (2000) Short-term prognosis in severe adult and adolescent malnutrition during famine. JAMA 284:621–626
McGrath J (1999) Hypothesis: is low prenatal vitamin D a risk-modifying factor for schizophrenia? Schizophrenia Res 40:173–177
Dealburto MJ (2007) Why are immigrants at increased risk for psychosis? Vitamin D insufficiency, epigenetic mechanisms, or both? Med Hypotheses 68:259–267
Insel BJ, Schaefer CA, McKeague IW, Susser ES, Brown AS (2008) Maternal iron deficiency and the risk of schizophrenia in offspring. Arch Gen Psychiatry 65:1136–1144
Onyut LP, Neuner F, Ertl V, Schauer E, Odenwald M, Elbert T (2009) Trauma, poverty and mental health among Somali and Rwandese refugees living in an African refugee settlement––an epidemiological study. Confl Health 3. doi:10.1186/1752-1505-3-6 (electronic version)
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The mini-international neuropsychiatric interview (MINI): the development and validation of a structured diagnostic interview for DSM-IV and ICD-10. J Clin Psychiatry 59(20):22–33
Gerritsen AAM, Bramsen I, Deville W, van Willigen LHM, Hovens JE, vander Ploeg HM (2006) Physical and mental health of Afghan, Iranian, and Somali asylum seekers and refugees living in the Netherlands. Soc Psychiatry Psychiatr Epidemiol 41:18–26
Silove D, Steel Z, Bauman A, Chey T, McFarlane A (2007) Trauma, PTSD and the longer-term mental health burden amongst Vietnamese refugees. Soc Psychiatry Psychiatr Epidemiol 42:467–476
Al-Saffar S, Borga P, Hallstrom T (2002) Long-term consequences of unrecognized PTSD in general outpatient psychiatry. Soc Psychiatry Psychiatr Epidemiol 37:580–585
Cougnard A, Marcelis M, Myin-Germeys I, De Graaf R, Vollebergh W, Krabbendam L, Lieb R, Wittchen HU, Henquet C, Spauwen J, Van Os J (2007) Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis? A psychosis proneness-persistence model. Psychol Med 37:513–527
Acknowledgments
This study was approved by the IRB Human Subjects Committee of the University of Minnesota Medical School. Dr. Fujiwara was supported in part by shared resources through the NIDA grant R21DA024626 (Khat Research Program: Neurobehavioral Impact of Long-Term Use; PI: Mustafa al’Absi). The authors thank Auke Tellegen, Ph.D. and Mustafa al’Absi, Ph.D. for discussion and analysis of the manuscript, Essa Hassan, Awo Qasim, Aisha Mohamed, Tahir Hassan, and Abdulahi Mohamed for dedicated involvement in this project and in the care of their patients at all times, and Amy Shellabarger for organizing the data retrieval of the control group.
Conflict of interest statement
The authors report no conflict of interest in this research project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kroll, J., Yusuf, A.I. & Fujiwara, K. Psychoses, PTSD, and depression in Somali refugees in Minnesota. Soc Psychiatry Psychiatr Epidemiol 46, 481–493 (2011). https://doi.org/10.1007/s00127-010-0216-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0216-0