Abstract
Objective
Several issues relevant to the care of Asian Indian patients remain poorly explored. Little is known about the practice patterns of psychiatrists in India, such as daily practice routines or treatment approaches, which we describe in New Delhi, India.
Methods
We focused on psychiatric practice, as perceived by Indian psychiatrists, using a sample from the USA as a comparison group. We used triangulated, qualitative methods from data gathered in India (ethnographic interviews with 16 Delhi psychiatrists, observation of treatment in India, and treatment of Indian patients) to design and validate a survey distributed to a sample of 34 psychiatrists in New Delhi and 34 in Baltimore, Maryland who treat Indian patients.
Results
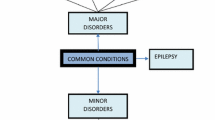
Delhi psychiatrists saw more patients daily (24.3 vs. 11, P < 0.001), and spent less time on new evaluations (33.3 vs. 69 min, P < 0.001). Both groups had similar approaches to major disorders. But, Delhi psychiatrists were less likely to combine medication treatment with psychotherapy (P < 0.05), and more likely to advise families to secretly administer medications in treatment refusal, such as in acute schizophrenia (P < 0.001) or major depression (P < 0.01).
Conclusions
These differences highlight the salience of local cultural context in the practice of psychiatry and in the treatment of Indian patients. Delhi psychiatrists are overwhelmed by the epidemic levels of untreated illness, spend less time with patients, and rely more heavily on medication treatment. Delhi psychiatrists employ unique approaches to handling difficult treatment issues, such as treatment refusal, intensive involvement of the family, and recommendations to the family about suitability for marriage for a patient.
Similar content being viewed by others
References
Agarwal AK, Katiyar M (2004) Chap. 26: status of psychiatric education at the postgraduate level. In: Agarwal SP (ed) Mental health: an Indian perspective 1946–2003. Ministry of Health and Family Welfare, New Delhi, pp 215–217
Bhatia MS (1999) An analysis of 60 cases of culture bound syndromes. Indian J Med Sci 53(4):149–152
Bhatia MS, Malik SC (1991) Dhat syndrome: a useful diagnostic entity in Indian culture. Br J Psychiatry 159:691–695
Chadda RK, Singh TB, Ganguly KK (2007) Caregiver burden and coping: a prospective study of relationship between burden and coping in cagregivers of patients with schizophrenia and bipolar affective disorder. Soc Psychiatry Psychiatr Epidemiol 42:923–930
Chakrabarti S, Kulhara P (2000) Patterns of antidepressant prescriptions: II continuation phase treatments. Indian J Psychiatry 42(1):29–33
Chakrabarti S, Kulhara P, Verma SK (1993) The pattern of burden in families of neurotic patients. Soc Psychiatry Psychiatr Epidemiol 28:172–177
Chakraborty A (1992) Psychiatry in India. Natl Med J India 5(4):184–186
Dongre N, D’Souza A, Shahain S, Ballary C, Poojary S, Ghai H, Rohira P (2001) Drug utilization study in psychiatry OPD of teaching hospital Indian pract. Indian Practitioner 54(2):77–81
Etzersdorfer E, Vijayakumar L, Schony W, Grausgruber A, Sonneck G (1998) Attitudes towards suicide among medical students: comparison between Madras (India) and Vienna (Austria). Soc Psychiatry Psychiatr Epidemiol 33:104–110
Gada MT, Agrawal BR, Pradhan PV, Shah LP, Bagadia VN (1984) Report from a World Health Organization (WHO) collaborative centre for psychopharmacology in India: survey of antipsychotic drugs use. Phychopharmacol Bull 20:180–184
Khandewal SK, Jhingan HP, Ramesh S, Rajesh K, Srivastava VK (2004) India mental health country profile. Int Rev Psychiatry 16(1/2):126–141
Martin DP, Engelberg R, Agel J, Snapp D, Swiontkowski MF (1996) Development of a musculoskeletal extremity health status instrument: the musculoskeletal function assessment instrument. J Orthop Res 14(2):173–181
Mohan D (2004) Chap. 27: general hospital-based psychiatric training: the All India Institute of Medical Sciences experience. In: Agarwal SP (ed) Mental health: an Indian perspective 1946–2003. Ministry of Health and Family Welfare, New Delhi
Mumford DB, Bavington JT, Bhatnagar KS, Hussain Y, Mirza S, Naraghi MM (1991) The Bradford somatic inventory: a multi-ethnic inventory of somatic symptoms reported by anxious and depressed patients in Britain and the Indo-Pakistan subcontinent. Br J Psychiatry 158:379–386
Nunley M (1988) The involvement of families in Indian psychiatry. Cult Med Psychiatry 22(3):317–353
Nunley M (1996) Why psychiatrists in India prescribe so many drugs. Cult Med Psychiatry 20(2):165–197
Paralikar V, Sarmukaddam S, Agashe M, Weiss MG (2007) Diagnostic concordance of neurasthenia spectrum disorders in Pune, India. Soc Psychiatry Psychiatr Epidemiol 42:561–572
Raguram R, Mitchell GW, Channabasavanna SM, Devins G (1996) Stigma, depression, and somatization in South India. Am J Psychiatry 153:1043–1049
Raguram R, Mitchell GW, Harshad K, Channabasavanna SM (2001) Cultural dimensions of clinical depression in Bangalore, India. Anthropol Med 8(1):31–46
Saravanan B, Jacob KS, Deepak MG, Prince M, David AS, Bhugra D (2008) Perceptions about psychosis and psychiatric services: a qualitative study from Vellore, India. Soc Psychiatry Psychiatr Epidemiol 43:231–238
Thara R, Padmavati R, Nagaswami V (1993) Schizophrenia in India. Epidemiology, phenomenology, course and outcome. Int Rev Psychiatry 5:157–164
Thara R, Padmavati R, Srinivasan TN (2004) Focus on psychiatry in India. Br J Psychiatry 184:366–373
Thara R, Srinivasan TN (1997) Outcome of marrige in schizophrenia. Soc Psychiatry Psychiatr Epidemiol 32:416–420
Weiss MG, Raguram R, Channabasavanna SM (1995) Cultural dimensions of psychiatric diagnosis: a comparison of DSM-III-R and illness explanatory models in South India. Br J Psychiatry 166:353–359
Wig NN (1999) Mental health and spiritual values. A view from the east. Int Rev Psychiatry 11:92–96
Williamson GR (2005) Illustrating triangulation in mixed-methods nursing research. Nurse Res 12(4):7–18
Wittchen HU (1994) Reliability and validity studies of the WHO–composite international diagnostic interview (CIDI): a critical review. J Psychiatr Res 28(1):57–84
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wasan, A.D., Neufeld, K. & Jayaram, G. Practice patterns and treatment choices among psychiatrists in New Delhi, India. Soc Psychiat Epidemiol 44, 109–119 (2009). https://doi.org/10.1007/s00127-008-0408-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0408-z