Abstract
Background
Psychiatric disorders and hypertension both independently increase risk for heart disease, cardiac events, and healthcare utilization. However, the contribution of specific psychiatric disorders to healthcare utilization in persons with hypertension is unknown.
Objective
To evaluate associations between psychiatric disorders and receipt of hospital care in people with hypertension.
Design
Cross-sectional epidemiologic survey.
Subjects
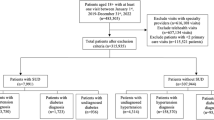
A total of 8,812 hypertensive individuals drawn from a randomly selected sample of 43,093 US adults.
Main outcomes
Participants were assessed in-person for a range of mental disorders (using the Diagnostic and Statistical Manual of Mental Disorders-IV), hypertension status (self-report), and past-year occurrence of emergency room treatment and overnight hospital stay (self-report).
Results
After controlling for demographics and clinical variables, persons having any lifetime mood, anxiety, or personality disorders had increased likelihood of emergency room treatment [odds ratios (ORs) = 1.26, 1.18, and 1.47, respectively]. Persons having any mood or personality disorder had increased likelihood of overnight hospital stay (ORs = 1.24 and 1.31, respectively). The specific disorders significantly associated with emergency room treatment were lifetime major depression, lifetime manic disorder, past-year major depression, past-year manic disorder, past-year panic disorder without agoraphobia, and paranoid, histrionic, antisocial, obsessive–compulsive personality disorders, with ORs ranging from 1.25 to 2.41. The specific disorders significantly associated with overnight hospital stay were lifetime dysthymia, lifetime manic disorder, past-year major depression, past-year manic disorder, and histrionic, antisocial, and paranoid personality disorders, with ORs ranging from 1.40 to 1.87.
Conclusion
Results suggest that addressing mental health problems in persons with hypertension may decrease healthcare utilization.
Similar content being viewed by others
References
Agatisa PK, Matthews KA, Bromberger JT et al (2005) Coronary and aortic calcification in women with a history of major depression. Arch Intern Med 165:1229–1236
CDC (2005) Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999–2002. MMWR 54:7–9
Carnethon MR, Biggs ML, Barzilay JI et al (2007) Longitudinal association between depressive symptoms and incident type 2 diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med 167:802–807
Agency for Healthcare Research Quality, Center for Delivery, Organization, and Markets, Healthcare utilization Project, Nationwide Inpatient Sample (2003)
Kozak LJ, Owings MF, Hall MJ (2005) National hospital discharge summary: 2002 annual summary with detailed diagnosis and procedure data. National Center for Health Statistics. Vital Health Stat 2005;13(158)
Ciechanowski P, Russo J, Katon W et al (2006) Where is the patient? The association of psychosocial factors and missed primary care appointments in patients with diabetes. Gen Hosp Psychiatr 28:9–17
Cowie C, Harris M (1997) Ambulatory medical care for non-Hispanic Whites, African Americans and Mexican Americans in the US. Diabetes Care 20:142–147
Merrill CT, Elixhauser A (2005) Hospitalization in the United States, 2002: HCUP Fact Book No. 6. AHRQ Publication No. 05-0056, June 2005. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/data/hcup/factbk6/
Fifield J, Tennen H, Reisine S et al (1998) Depression and the long-term risk of pain, fatigue, and disability in patients with rheumatoid arthritis. Arthritis Rheum 41:1851–1857
Frasure-Smith N, Lesperance F (2005) Reflections on depression as a cardiac risk factor. Psychosom Med 67(suppl 1):S19–S25
Grant BF, Dawson DA, Stinson FS et al (2003) the alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend 71:7–16
Grant BF, Harford TC, Dawson DA et al (1995) The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend 39:37–44
Grant BF, Hasin DS (1991) The alcohol use disorders and associated disabilities interview schedule (AUDADIS). National Institute on Alcohol Abuse and Alcoholism, Rockville
Grant BF, Moore TC, Kaplan K (2003) Source and accuracy statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). National Institute on Alcohol Abuse and Alcoholism, Bethesda
Hasin D, Carpenter KM, McCloud S et al (1997) The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend 44:133–141
Henk HJ, Katzelnikc DJ, Kobak KA et al (1996) Medical costs attributed to depression among patients with a history of high medical expenses in a health maintenance organization. Arch Gen Psychiatr l53:899–904
Himelhoch S, Weller WE, Wu AW et al (2004) Chronic medical illness, depression, and use of acute medical services among medicare beneficiaries. Med Care 42:512–521
Jones DJ, Bromberger JT, Sutton-Tyrrell K et al (2003) Lifetime history of depression and carotid atherosclerosis in middle-aged women. Arch Gen Psychiatry 60(2):153–160
Kennedy N, Paykel ES (2004) Residual symptoms at remission from depression: impact on long term outcome. J Affect Disord 80:135–144
Kessler LG, Burns B, Shapiro S et al (1987) Psychiatric diagnoses of medical service users: evidence from the Epidemiological Catchment Area program. AJPH 77:18–24
Machlin SR (2006) Expenses for a hospital emergency room visit, 2003. Statistical brief #111 (Agency for Healthcare Research and Quality website). Available at: http://www.meps.ahrq.gov/papers/st111/stat111.pdf. Accessed June 26, 2007
Machlin SR, Carper K (2007) Expenses for inpatient hospital stays, 2004. Statistical brief #164 (Agency for Healthcare Research and Quality website). Available at: http://www.meps.ahrq.gov/mepsweb/data_files/publications/st164/stat164.pdf. Accessed June 26, 2007
National Heart Lung and Blood Institute (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res 6(suppl 2):51S–209S
Pirraglia PA, Rosen AB, Hermann RC et al (2004) Cost-utility analysis studies of depression management: a systematic review. Am J Psychiatr 161:2155–2162
Post R (1992) Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry 149:999–1010
Research Triangle Institute (2003) Software for survey data analysis (SUDAAN). Research Triangle Institute, Research Triangle Park
Sheline YI, Sanghavi M, Mintun MA et al (1999) Depression duration but not age predicts hippocampal volume loss in medically healthy women with recurrent major depressive depression. J Neurosci 19:5034–5043
Simon G, VonKorff M, Barlow W (1995) Healthcare costs of primary care patients with recognized depression. Arch Gen Psychiatr 52:850–856
Unutzer J, Patrick D, Simon G et al (1997) Depressive symptoms and the cost of health services in HMO patients aged 65 years and older: a 4-year prospective study. JAMA 277:1618–1623
Wagner J, Tennen H (2007) History of major depressive disorder and diabetes outcomes among diet and tablet treated postmenopausal women: a case control study. Diabet Med 24: 211–216
Wagner J, Tennen H, Mansoor G et al (2006) History of depression and endothelial function in post-menopausal women. Psychosom Med 68: 80–86
Wolf-Maier K, Cooper RS, Banegas J et al (2003) Hypertension prevalence and blood pressure in 6 European countries, Canada, and the United States. JAMA 289:2363–2369
Acknowledgments
Preparation of this report was supported in part by NIH grants R01-MH60417, R01-MH60417-Supp, R01-DA13444, R01-DA018883, R01-DA14618, R01-DA016855, P50-AA03510, P50-DA09241, R21-DK074468, and grants from the American Heart Association and the American Diabetes Association. We thank NIAAA and the U.S. Census Bureau field representatives who administered the NESARC interview.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wagner, J.A., Pietrzak, R.H. & Petry, N.M. Psychiatric disorders are associated with hospital care utilization in persons with hypertension. Soc Psychiat Epidemiol 43, 878–888 (2008). https://doi.org/10.1007/s00127-008-0377-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0377-2