Abstract
Aims/hypothesis
Exposure to artificial light at night (LAN) disrupts the circadian timing system and might be a risk factor for diabetes. Our aim was to estimate the associations of chronic exposure to outdoor LAN with glucose homoeostasis markers and diabetes prevalence based on a national and cross-sectional survey of the general population in China.
Methods
The China Noncommunicable Disease Surveillance Study was a nationally representative study of 98,658 participants aged ≥18 years who had been living in their current residence for at least 6 months recruited from 162 study sites across mainland China in 2010. Diabetes was defined according to ADA criteria. Outdoor LAN exposure in 2010 was estimated from satellite data and the participants attending each study site were assigned the same mean radiance of the outdoor LAN at the study site. The linear regression incorporating a restricted cubic spline function was used to explore the relationships between LAN exposure and markers of glucose homoeostasis. Cox regression with a constant for the time variable assigned to all individuals and with robust variance estimates was used to assess the associations between the levels of outdoor LAN exposure and the presence of diabetes by calculating the prevalence ratios (PRs) with adjustment for age, sex, education, smoking status, drinking status, physical activity, family history of diabetes, household income, urban/rural areas, taking antihypertensive medications, taking lipid-lowering medications, and BMI.
Results
The mean age of the study population was 42.7 years and 53,515 (weighted proportion 49.2%) participants were women. Outdoor LAN exposure levels were positively associated with HbA1c, fasting and 2 h glucose concentrations and HOMA-IR and negatively associated with HOMA-B. Diabetes prevalence was significantly associated with per-quintile LAN exposure (PR 1.07 [95% CI 1.02, 1.12]). The highest quintile of LAN exposure (median 69.1 nW cm−2 sr−1) was significantly associated with an increased prevalence of diabetes (PR 1.28 [95% CI 1.03, 1.60]) compared with the lowest quintile of exposure (median 1.0 nW cm−2 sr−1).
Conclusions/interpretation
There were significant associations between chronic exposure to higher intensity of outdoor LAN with increased risk of impaired glucose homoeostasis and diabetes prevalence. Our findings contribute to the growing evidence that LAN is detrimental to health and point to outdoor LAN as a potential novel risk factor for diabetes.
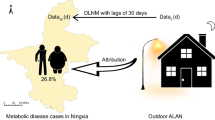
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Nocturnal exposure to outdoor artificial light from various light sources is a ubiquitous environmental risk factor in modern societies [1]. Urban light pollution can affect not only residents in big cities but also those in distant areas such as suburbs and forest parks, which are hundreds of kilometres from the light source. Despite over 80% of the world’s population being exposed to light pollution at night [1], this problem has gained limited attention from scientists until recent years [2].
Under nature’s 24 h light–dark cycle, most organisms, including mammals, have developed an endogenous circadian timing system adapted to the regular alternation of light and dark phases. Exposure to artificial light at night (LAN) may suppress the nocturnal secretion of pineal melatonin [3] and animal experiments have discovered that light pollution alters the circadian rhythm of insects, birds and other animals, resulting in premature death and loss of biodiversity [4]. Exposure to artificial LAN may disrupt the typical timing of food intake and subsequently induce metabolic dysregulation [5]. In experiments with rats, acute exposure to LAN induced glucose intolerance, as demonstrated by increased plasma glucose levels at the start of exposure and subsequently increased plasma insulin [6]. However, another animal study showed that 12 h exposure to dim white light (5 lx) at night strongly reduced the daily rhythms in sleep–wake behaviour but did not affect body weight or glucose tolerance [7]. The effects of chronic LAN exposure have also been assessed in mice. Mice exposed to as little as 5 lx of light for 4 weeks had increased body mass and reduced glucose tolerance compared with mice housed in the dark at night, despite displaying equivalent energy consumption and expenditure [8].
Night-shift workers exposed to higher levels of LAN were found to be at higher risks of disrupted circadian rhythms and CHD [9, 10]. Another meta-analysis summarised that a higher LAN exposure was consistently associated with 13% and 22% higher odds of being overweight and obese, respectively [11]. In a cross-sectional study conducted among adults in South India, LAN exposure measured by satellite was found to be positively associated with BMI, systolic BP and LDL-cholesterol but not with fasting glucose [12]. However, bedroom LAN exposure was reported to be positively associated with the development of diabetes in a general elderly population [13].
Diabetes is a critical public health problem in China [14]. The onset and progression of diabetes is ascribed largely to behavioural and environmental risk factors [15]. With the rapid development of urbanisation and economies, urban artificial lighting has greatly increased in China [16]. People living in cities are more prone to being shifted away from nature’s 24 h day–night rhythm towards a pattern of working around the clock, staying out late and exposure to artificial LAN. It is therefore essential to assess the extent of the artificial LAN leading to or related to diabetes so as to implement effective prevention strategies. We aimed to estimate the associations between chronic exposure to outdoor artificial LAN and glucose homoeostasis markers and diabetes prevalence based on a national and cross-sectional survey of the general population in China.
Methods
Study design and participants
We used data from a nationally representative sample of the general population in China. Details of the study design and protocol have been described previously [17]. Briefly, the China Noncommunicable Disease Surveillance Study was conducted in 2010 within the National Disease Surveillance Point System of Chinese Center for Disease Control and Prevention, and included 162 study sites covering various geographical areas of all 31 provinces, autonomous regions and municipalities in mainland China.
A complex, multistage, probability sampling design was used at each study site to select a general population that was representative of civilian, non-institutionalised Chinese adults aged ≥18 years. At the first stage of sampling, four subdistricts were selected at each site with probability proportional to size. At the second stage, three neighbourhood communities or administrative villages were selected proportional to size within each subdistrict. At the third stage, 50 households within each community or village were randomly selected. Only one local permanent resident was selected at random from each household using a Kish selection table [18]. A total of 109,023 adults living in their current residence for at least 6 months were selected. Finally, 98,658 Chinese adults responded and participated in the survey. The study protocol was approved by the ethical review committee of the Chinese Center for Disease Control and Prevention and other participating centres. Written informed consent was obtained from all study participants.
Data collection
The 2010 China Noncommunicable Disease Surveillance Study was conducted in the examination centres at local health stations or community clinics by trained staff according to a standardised protocol. A face-to-face interview was conducted to collect information on demographic characteristics, education, household income, lifestyle habits, disease history and current medications, and family history of diabetes, etc., using a standard questionnaire. Household income was recorded for the year of 2009 (the previous year of the survey). Current smoking was defined as having smoked at least 100 cigarettes in one’s lifetime and currently smoking cigarettes. Current drinking was defined as alcohol intake more than once per month during the past 12 months. Physical activity was estimated from responses to the Global Physical Activity Questionnaire, which included questions on intensity, duration and frequency of physical activity. Total metabolic equivalents minutes per week were calculated to provide a measurement of physical activity levels. A high level of physical activity was defined as follows: ≥150 min/week moderate intensity; ≥75 min/week vigorous intensity; or ≥150 min/week moderate or vigorous intensity. Body weight and height were measured according to a standard protocol and BMI was calculated as weight (kg) divided by height squared (m2). Normal weight, overweight and obesity were defined as BMI <24.0 kg/m2, BMI 24.0–27.9 kg/m2 and BMI ≥28.0 kg/m2, respectively, as recommended by the Working Group on Obesity in China [19]. Blood samples were obtained from all participants after they had fasted overnight for ≥10 h. Participants not diagnosed previously with diabetes underwent 2 h OGTT by being given 75 g glucose solution. Fasting plasma glucose (FPG) and 2 h postprandial glucose (PG) were measured at 0 h and 2 h, respectively, during the OGTT. Blood samples were collected using a vacuum collection tube containing anticoagulant sodium fluoride and centrifuged on-site within 2 h of collection. Details on the measurement of FPG, 2 h PG and HbA1c have been described in previous publications and insulin concentrations at fasting state were determined via immunoassay at the central laboratory [17]. Diabetes was defined as FPG ≥7.0 mmol/l, and/or 2 h PG ≥11.1 mmol/l, and/or HbA1c ≥48 mmol/mol (6.5%), and/or a self-reported previous diagnosis of diabetes by healthcare professionals regardless of the participants’ current medications. We estimated insulin resistance by the HOMA-IR and beta cell function by the HOMA-B [20].
Outdoor LAN exposure
Data on the exposure levels of artificial outdoor LAN were retrieved from the US Defense Meteorological Satellite Program (DMSP) (https://ngdc.noaa.gov/eog/download.html, accessed 15 June 2021). The Operational Linescan System (OLS), flown on the DMSP satellites, is capable of recording low-light imaging data at night worldwide. These data were archived at the US National Geophysical Data Center (NGDC). The data contained annual composites of images of outdoor LAN after excluding sun and moon luminance, clouds, atmospheric lighting and ephemeral events such as fires. Although these images capture only a fraction of the light originating from the Earth’s surface, they represent the relative intensity of night-time illumination at ground level. There were two types of LAN data available. The ordinary DMSP-OLS Nighttime Lights Time Series, with digital numbers ranging from 0 to 63, could not accommodate bright sources (i.e. city centres) within its limited dynamic range. To solve the ‘saturation’ problem, which happens in the ordinary DMSP-OLS night-time light product, the most recent Global Radiance Calibrated Nighttime Lights expanded the dynamic range and transforms data into units of illumination (nW cm−2 sr−1) [21, 22]. To estimate the LAN exposure for study participants, we used the high dynamic range data throughout the year 2010 downloaded from the NGDC (https://ngdc.noaa.gov/eog/dmsp/download_radcal.html, data version ‘F16_20100111-20101209_rad_v4’; see electronic supplementary material [ESM] Fig. 1). The mean night-time radiance of the outdoor LAN for each study site, which was either a district in a city or a county in a rural area, was calculated and participants living within each study site were assigned the same mean radiance of the outdoor LAN at that study site.
Statistical analysis
To account for the multistage probability sampling design of the survey, the appropriate weights and design factors were considered to represent the overall Chinese adult population aged 18 years or older in all the analyses. Weight coefficients were derived from 2010 China population census data and the sampling scheme of the current survey to obtain national estimates [17]. Details of weighting methods are provided in ESM Methods. Demographic and metabolic characteristics of study participants are presented as means (95% CIs) for continuous variables and percentages (95% CIs) for categorical variables. The mean values and percentages in different groups were compared using ANOVA and χ2 tests. As suggested by previous studies [23, 24], we used Cox regression with a constant for the time variable assigned to all individuals and with robust variance estimates to assess the association between the level of outdoor LAN exposure and the presence of diabetes by calculating the prevalence ratio (PR) per quintile of LAN exposure or for each of the upper four quintiles relative to the lowest quintile of LAN, with adjustment for covariates. We selected a priori potential confounders for adjustment in multivariable models based on knowledge of their associations with LAN exposure and diabetes. These factors included age, sex, education, smoking status, drinking status, physical activity, family history of diabetes, household income, urban/rural living, taking antihypertensive medications, taking lipid-lowering medications, and BMI. To explore the possible relationships between LAN exposure and glucose homoeostasis markers and prevalent diabetes, linear regression and Cox regression with equal times assigned to all individuals and with robust variance estimates were performed by incorporating a restricted cubic spline function of LAN with the reference value of 0.1 nW cm−2 sr−1. Three knots at the 5th, 50th and 95th percentiles were automatically set for the splines. In addition, because missing data in the current study were limited (1–2% for all variables in the analysis), these were ignored and models were built on the remaining data.
The number needed to harm (NNH) was calculated to indicate how many individuals needed to be exposed to a particular level of LAN for one additional case of diabetes, when compared with individuals exposed to the lowest level of LAN. Confounding was considered according to the methods suggested by Bender and Blettner [25]. We then estimated the number of diabetes diagnoses in Chinese adults aged ≥18 years that can be attributed to LAN exposure using the Chinese population aged ≥18 years divided by NNH. Details of the calculation are provided in ESM Methods.
All analyses were performed using R version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria). A two-sided p<0.05 was considered statistically significant.
Results
The radiance of LAN exposure varied substantially across China (Fig. 1a). Most areas were exposed to a low intensity of outdoor LAN, while a higher intensity of outdoor LAN converged on the eastern coastal cities. The distribution of the outdoor LAN among the 162 study sites was skewed to the left and the median (IQR) LAN exposure of all study sites was 7.9 (2.8, 26.8) nW cm−2 sr−1 (Fig. 1b). The mean (95% CI) age of the participants was 42.7 (41.9, 43.5) years; 53,515 (weighted proportion 49.2%) participants were women. In further analyses, we categorised the participants by the quintiles of the outdoor LAN exposure. The median (IQR) of outdoor LAN in quintile 1 to quintile 5, respectively, was 1.0 (0.6, 1.7), 3.9 (3.2, 4.8), 7.0 (6.3, 8.1), 17.0 (10.5, 24.5) and 69.1 (53.9, 117.0) nW cm−2 sr−1 (Fig. 1c). Baseline characteristics of the study participants by LAN exposure are shown in Table 1. Participants in the higher quintiles of outdoor LAN were more likely to be older, have a higher BMI and household income and live in an urban area. Participants in the lower quintiles of outdoor LAN reported higher levels of physical activity but fewer years of education.
Distribution of outdoor LAN exposure. (a) Map of outdoor LAN in China in 2010, with study sites indicated by circles. (b) The number of participants exposed to each radiance level of outdoor LAN. (c) The distribution of the radiance categorised by quintiles of outdoor LAN. The median (25% quartile, 75% quartile) of LAN in quintile 1 to quintile 5, respectively, was 1.0 (0.6, 1.7), 3.9 (3.2, 4.8), 7.0 (6.3, 8.1), 17.0 (10.5, 24.5) and 69.1 (53.9, 117.0) nW cm−2 sr−1. The total number of participants was 98,658. The number of participants in quintile 1 to quintile 5, respectively, was 24,151, 14,392, 15,028, 23,773 and 21,314
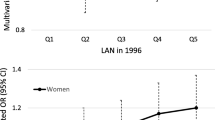
We examined the shape of the exposure–response curve for the relationship between outdoor LAN exposure and glucose homoeostasis markers and diabetes (Fig. 2). There were apparently monotonically increasing exposure–response curves for the associations between outdoor LAN exposure (reference concentration 0.1 nW cm−2 sr−1 as the lowest concentration to which participants were exposed) and HbA1c, FPG, 2h PG, and HOMA-IR (Fig. 2a–d). The association between outdoor LAN exposure and HOMA-B was monotonical and decreasing, with a steeper slope at radiance below 20 nW cm−2 sr−1 (Fig. 2e). The PRs for the association between outdoor LAN exposure and diabetes presented a similar shape of curve to those of HbA1c, FPG, 2 h PG and HOMA-IR (Fig. 2f).
Spline curves for outdoor LAN and glucose homoeostasis markers and diabetes: HbA1c (a); FPG (b); 2 h PG (c); HOMA-IR (d); HOMA-B (e); and diabetes (f). The data used for analysis of glucose homoeostasis markers excluded participants previously diagnosed with diabetes. In all analyses, participants experiencing the top 10% of LAN were trimmed for the spline model. The number of participants in (a–f), respectively, was 83,835, 83,858, 82,843, 83,545, 83,545 and 86,231. LAN was fitted as a smooth term using a restricted cubic spline with three knots. Shading indicates 95% CIs. The reference artificial LAN level was 0.1 nW cm−2 sr−1. The model was adjusted for age, sex, education, smoking status, drinking status, physical activity, family history of diabetes, household income, urban/rural habitation, taking antihypertensive medications, taking lipid-lowering medications, and BMI. There were 1092 missing values for HbA1c, 895 missing values for fasting glucose, 2073 missing values for 2 h PG, 1313 missing values for HOMA-IR, 1313 missing values for HOMA-B and 1432 missing values for total diabetes
Table 2 shows the PRs and 95% CIs for the associations between per quintile of outdoor LAN exposure and various definitions of diabetes prevalence. We observed positive and similar PRs in models 1–3, while in model 4 (with additional adjustment for BMI), the associations between outdoor LAN and HbA1c ≥48 mmol/mol (6.5%) and FPG ≥7.0 mmol/l were no longer statistically significant. The per-quintile LAN exposure was positively associated with diabetes prevalence in model 4 (PR 1.07 [95% CI 1.02, 1.12]).
A high intensity of outdoor LAN exposure was associated with a higher prevalence of diabetes (Fig. 3). In the adjusted model, the PR (95% CI) for quintile 5 of LAN exposure was 1.39 (1.14, 1.70) for HbA1c ≥48 mmol/mol (6.5%), 1.38 (1.03, 1.85) for FPG ≥7.0 mmol/l, and 1.40 (1.11, 1.70) for 2h PG ≥11.1 mmol/l, compared with the lowest quintile (Fig. 3a–c). A significant PR of 1.28 (1.03, 1.60) for prevalent diabetes was also observed in the highest quintile of LAN exposure compared with the lowest quintile (Fig. 3d). The NNH of diabetes for quintiles 2, 3, 4 and 5 of LAN exposure was 166, 1163, 78 and 42, respectively. The total number of diabetes diagnoses in Chinese adults aged ≥18 years that can be attributed to LAN exposure was estimated to be 9,015,056.
Associations between outdoor LAN and diabetes with different definitions. (a) HbA1c ≥48 mmol/mol (6.5%) and/or previously diagnosed diabetes. (b) FPG ≥7.0 mmol/l and/or previously diagnosed diabetes. (c) 2 h PG ≥11.1 mmol/l and/or previously diagnosed diabetes. (d) FPG ≥7.0 mmol/l, and/or 2 h PG ≥11.1 mmol/l, and/or HbA1c ≥48 mmol/mol (6.5%), and/or previously diagnosed diabetes. A log-scale was used for the PR. The model was adjusted for age, sex, education, smoking status, drinking status, physical activity, family history of diabetes, household income, urban/rural habitation, taking antihypertensive medications, taking lipid-lowering medications, and BMI. There were 1092 missing values for HbA1c ≥48 mmol/mol (6.5%) and/or previously diagnosed diabetes, 895 missing values for FPG ≥7.0 mmol/l and/or previously diagnosed diabetes, 2073 missing values for 2 h PG ≥11.1 mmol/l and/or previously diagnosed diabetes, and 1432 missing values for total diabetes
Discussion
Based on this nationwide survey of the Chinese adult general population, we found that chronic exposure to residential outdoor LAN was positively associated with blood glucose levels, insulin resistance and diabetes prevalence, and inversely associated with beta cell function; these associations were robust after adjustment for many important diabetes risk factors. On average, for every 42 individuals living in the region with the highest quintile of LAN exposure, one more individual would have diabetes than if those same individuals lived in the region with the lowest quintile of LAN exposure. Although the association of LAN exposure with diabetes might not be as strong as its relationship with more established risk factors such as obesity [17], vast amounts of people could be exposed to outdoor LAN. We reported that an estimated 9 million cases of diabetes in Chinese adults aged ≥18 years could be attributed to LAN exposure. Our findings are important for estimating the effect of light pollution on public health in China. Considering the accelerating urbanisation along with the growing number of domestic migrants to cities, the estimated amount of light-pollution-related diabetes is projected to increase.
In the present study, we used night-time satellite imagery provided by the US DMSP to estimate the intensity of outdoor LAN exposure. By using satellite data, several lines of evidence also support the detrimental consequences of outdoor LAN exposure on metabolic regulation and disease, such as obesity [26, 27], psychiatric disorders [28] and cancer [29]. For example, in an analysis based on a prospective cohort of older adults in Hong Kong, a 60 nW cm−2 sr−1 increase in outdoor LAN was associated with a 10% increased risk of CHD [30]. However, fewer studies have evaluated the association between outdoor LAN exposure and risk of diabetes. The current study is the largest epidemiological study to test the hypothesis that increased exposure to outdoor LAN is associated with a higher possibility of developing hyperglycaemia, insulin resistance and diabetes.
It is undeniable that the satellite imagery showing outdoor LAN is a proxy measure of the actual LAN exposure and supposes that all the residents living in one place are affected by the same intensity of LAN. Different from our study, Chamorro et al examined the effects of acute exposure to mild dim LAN on sleep architecture and glucose homoeostasis in 20 healthy normal-weight men at the individual level [31]. They did not observe significant associations between light exposure and levels of blood glucose, insulin and C-peptide [31]. However, another clinical trial with a parallel-group design including 20 young adults found that one night of moderate (100 lx) light exposure during sleep increased night-time heart rate, decreased heart rate variability (higher sympathovagal balance) and increased next-morning insulin resistance when compared with sleep in a dimly lit (<3 lx) environment [32]. A prospective study, following a group of elderly individuals, found that exposure to high-intensity LAN in the bedroom was associated with increased risk of incident diabetes independent of sleep-related variables [13]. Three population studies which assessed the intensity of LAN exposure during the participants’ in-bed period also found that exposure to LAN was associated with obesity [33], impaired lipid variables [34] and increased night-time BP [35]. Exposure to LAN may increase the risk of metabolic disease by disruption of circadian rhythms leading to a wide array of changes in physiological activities and metabolic variables, including locomotor activity, body temperature, food intake, lipid profile, insulin sensitivity, glucose metabolism and levels of plasma melatonin, glucocorticoids and fatty acids [36]. Furthermore, LAN exposure-induced disturbances in the central clock lead to perturbed circadian rhythms in brain regions and a disturbed interplay between different peripheral tissues [36].
Falchi et al reported that 83% of the world’s population and >99% of the US and European populations live under light-polluted skies [1], therefore it may not be possible to observe the associations between outdoor LAN and diabetes since the exposure is within narrow limits in Europe and the USA. China is a developing country with great regional disparities. As shown in our study, there are huge differences in the intensity of the exposure to outdoor LAN between the eastern coastal cities and the rural regions in middle and western China. Therefore, a major strength of the present study is that the data are collected from participants recruited across mainland China with a broad coverage of geographical areas with different outdoor LAN exposure intensities, and thus a certain level of representativeness of populations can be justified.
Study limitations
Our study has some limitations. First, the satellite-based estimate of outdoor LAN is a crude measure of LAN exposure. The mean night-time radiance of the outdoor LAN at each study site, which was either a district in a city or a county in a rural area, was assigned to each participant at the same study site. However, there might be differences in LAN exposure levels between one end of the study site and the other. Multiple factors can also influence the actual LAN exposure at an individual level, such as indoor lighting, night-time activities in both indoor and outdoor settings, and the use of light-blocking materials. Second, we cannot infer causality due to the cross-sectional nature of the study. Third, LAN exposure during the year 2010 may not reflect long-term cumulative exposure or changes in LAN. Although we recruited the participants who had been living at their current residence for at least 6 months, exposure misclassification is still possible if LAN levels changed substantially in the same areas where people resided. Additionally, we could not separate the effects of LAN with different wavelengths. Experimental evidence has demonstrated that blue light is most potent in suppressing melatonin release in humans [37]. Further study may explore the effects of light at different wavelengths on health. Finally, although we have adjusted for several socioeconomic and lifestyle-related variables, confounding from socioeconomic status and sleep behaviours for the association between LAN exposure and diabetes cannot be fully ruled out.
In conclusion, the current study demonstrates a significant association of higher intensity of outdoor LAN exposure with impaired glucose homoeostasis markers and the presence of diabetes. Our findings contribute to the growing literature suggesting that LAN is detrimental to health and demonstrate that LAN may be a potential novel risk factor for diabetes. However, we advise caution against causal interpretation of the findings and call for further studies involving direct measurement of individual exposure to LAN.
Data availability
Data are available from the corresponding authors upon request.
Abbreviations
- DMSP:
-
Defense Meteorological Satellite Program
- FPG:
-
Fasting plasma glucose
- LAN:
-
Light at night
- NGDC:
-
National Geophysical Data Center
- NNH:
-
Number needed to harm
- OLS:
-
Operational Linescan System
- PG:
-
Postprandial glucose
- PR:
-
Prevalence ratio
References
Falchi F, Cinzano P, Duriscoe D et al (2016) The new world atlas of artificial night sky brightness. Sci Adv 2(6):e1600377. https://doi.org/10.1126/sciadv.1600377
Stevens RG, Zhu Y (2015) Electric light, particularly at night, disrupts human circadian rhythmicity: is that a problem? Philos Trans R Soc Lond Ser B Biol Sci 370(1667):20140120. https://doi.org/10.1098/rstb.2014.0120
Crnko S, Du Pre BC, Sluijter JPG, Van Laake LW (2019) Circadian rhythms and the molecular clock in cardiovascular biology and disease. Nat Rev Cardiol 16(7):437–447. https://doi.org/10.1038/s41569-019-0167-4
Barre K, Vernet A, Azam C et al (2022) Landscape composition drives the impacts of artificial light at night on insectivorous bats. Environ Pollut 292(Pt B):118394. https://doi.org/10.1016/j.envpol.2021.118394
Nelson RJ, Chbeir S (2018) Dark matters: effects of light at night on metabolism. Proc Nutr Soc 77(3):223–229. https://doi.org/10.1017/S0029665118000198
Opperhuizen AL, Stenvers DJ, Jansen RD, Foppen E, Fliers E, Kalsbeek A (2017) Light at night acutely impairs glucose tolerance in a time-, intensity- and wavelength-dependent manner in rats. Diabetologia 60(7):1333–1343. https://doi.org/10.1007/s00125-017-4262-y
Stenvers DJ, van Dorp R, Foppen E et al (2016) Dim light at night disturbs the daily sleep-wake cycle in the rat. Sci Rep 6:35662. https://doi.org/10.1038/srep35662
Fonken LK, Workman JL, Walton JC et al (2010) Light at night increases body mass by shifting the time of food intake. Proc Natl Acad Sci U S A 107(43):18664–18669. https://doi.org/10.1073/pnas.1008734107
Vetter C, Devore EE, Wegrzyn LR et al (2016) Association Between Rotating Night Shift Work and Risk of Coronary Heart Disease Among Women. JAMA 315(16):1726–1734. https://doi.org/10.1001/jama.2016.4454
Vyas MV, Garg AX, Iansavichus AV et al (2012) Shift work and vascular events: systematic review and meta-analysis. BMJ 345:e4800. https://doi.org/10.1136/bmj.e4800
Lai KY, Sarkar C, Ni MY, Gallacher J, Webster C (2020) Exposure to light at night (LAN) and risk of obesity: A systematic review and meta-analysis of observational studies. Environ Res 187:109637. https://doi.org/10.1016/j.envres.2020.109637
Sorensen TB, Wilson R, Gregson J, Shankar B, Dangour AD, Kinra S (2020) Is night-time light intensity associated with cardiovascular disease risk factors among adults in early-stage urbanisation in South India? A cross-sectional study of the Andhra Pradesh Children and Parents Study. BMJ Open 10(11):e036213. https://doi.org/10.1136/bmjopen-2019-036213
Obayashi K, Yamagami Y, Kurumatani N, Saeki K (2020) Bedroom lighting environment and incident diabetes mellitus: a longitudinal study of the HEIJO-KYO cohort. Sleep Med 65:1–3. https://doi.org/10.1016/j.sleep.2019.07.006
Li Y, Teng D, Shi X et al (2020) Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ 369:m997. https://doi.org/10.1136/bmj.m997
Talmud PJ, Hingorani AD, Cooper JA et al (2010) Utility of genetic and non-genetic risk factors in prediction of type 2 diabetes: Whitehall II prospective cohort study. BMJ 340:b4838. https://doi.org/10.1136/bmj.b4838
Han P, Huang J, Li R et al (2014) Monitoring trends in light pollution in china based on nighttime satellite imagery. Remote Sens 6:5541–5558. https://doi.org/10.3390/rs6065541
Xu Y, Wang L, He J et al (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310(9):948–959. https://doi.org/10.1001/jama.2013.168118
Kish L (1949) A procedure for objective respondent selection within the household. J Am Stat Assoc 44(247):380–387. https://doi.org/10.2307/2280236
Zhou BF, Cooperative Meta-Analysis Group of the Working Group on Obesity in C (2002) Predictive values of BMI and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 15(1):83–96
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419. https://doi.org/10.1007/BF00280883
National Oceanic and Atmospheric Administration/ National Geophysical Data Center. Global Radiance Calibrated Nighttime Lights. https://www.ngdc.noaa.gov/eog/dmsp/download_radcal.html (15 June 2021).
Hsu F-CBK, Ghosh T, Zhishin M, Elvidge CD (2015) DMSP-OLS radiance calibrated nighttime lights time series with intercalibration. Remote Sens 7(2):1855–1876. https://doi.org/10.3390/rs70201855
Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3:21. https://doi.org/10.1186/1471-2288-3-21
Diaz-Quijano FA (2012) A simple method for estimating relative risk using logistic regression. BMC Med Res Methodol 12:14. https://doi.org/10.1186/1471-2288-12-14
Bender R, Blettner M (2002) Calculating the “number needed to be exposed” with adjustment for confounding variables in epidemiological studies. J Clin Epidemiol 55(5):525–530. https://doi.org/10.1016/S0895-4356(01)00510-8
Koo YS, Song JY, Joo EY et al (2016) Outdoor artificial light at night, obesity, and sleep health: Cross-sectional analysis in the KoGES study. Chronobiol Int 33(3):301–314. https://doi.org/10.3109/07420528.2016.1143480
Zhang D, Jones RR, Powell-Wiley TM, Jia P, James P, Xiao Q (2020) A large prospective investigation of outdoor light at night and obesity in the NIH-AARP Diet and Health Study. Environ Health 19(1):74. https://doi.org/10.1186/s12940-020-00628-4
Min JY, Min KB (2018) Outdoor light at night and the prevalence of depressive symptoms and suicidal behaviors: A cross-sectional study in a nationally representative sample of Korean adults. J Affect Disord 227:199–205. https://doi.org/10.1016/j.jad.2017.10.039
Xiao Q, Jones RR, James P, Stolzenberg-Solomon RZ (2021) Light at night and risk of pancreatic cancer in the NIH-AARP diet and health study. Cancer Res 81(6):1616–1622. https://doi.org/10.1158/0008-5472.CAN-20-2256
Sun S, Cao W, Ge Y et al (2021) Outdoor light at night and risk of coronary heart disease among older adults: a prospective cohort study. Eur Heart J 42(8):822–830. https://doi.org/10.1093/eurheartj/ehaa846
Chamorro R, Wilms B, Holst A et al (2021) Acute mild dim light at night slightly modifies sleep but does not affect glucose homeostasis in healthy men. Sleep Med 84:158–164. https://doi.org/10.1016/j.sleep.2021.05.038
Mason IC, Grimaldi D, Reid KJ et al (2022) Light exposure during sleep impairs cardiometabolic function. Proc Natl Acad Sci U S A 119(12):e2113290119. https://doi.org/10.1073/pnas.2113290119
Park YM, White AJ, Jackson CL, Weinberg CR, Sandler DP (2019) Association of exposure to artificial light at night while sleeping with risk of obesity in women. JAMA Intern Med 179(8):1061–1071. https://doi.org/10.1001/jamainternmed.2019.0571
Obayashi K, Saeki K, Iwamoto J et al (2013) Exposure to light at night, nocturnal urinary melatonin excretion, and obesity/dyslipidemia in the elderly: a cross-sectional analysis of the HEIJO-KYO study. J Clin Endocrinol Metab 98(1):337–344. https://doi.org/10.1210/jc.2012-2874
Obayashi K, Saeki K, Iwamoto J, Ikada Y, Kurumatani N (2014) Association between light exposure at night and nighttime blood pressure in the elderly independent of nocturnal urinary melatonin excretion. Chronobiol Int 31(6):779–786. https://doi.org/10.3109/07420528.2014.900501
Fleury G, Masis-Vargas A, Kalsbeek A (2020) Metabolic implications of exposure to light at night: lessons from animal and human studies. Obesity 28(Suppl 1):S18–S28. https://doi.org/10.1002/oby.22807
Brainard GC, Sliney D, Hanifin JP et al (2008) Sensitivity of the human circadian system to short-wavelength (420-nm) light. J Biol Rhythm 23(5):379–386. https://doi.org/10.1177/0748730408323089
Acknowledgements
The authors are grateful to all the staff members and participants for collecting and providing study data.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
RZ and ZX contributed equally to the work and should be regarded as joint first authors. RZ and YX conceived and designed the study. ML, TW, MX, JL, SW, HL, MD, DZ, YC, WW, GN, YB and YX contributed to data acquisition . RZ, ZX, ZZ and YX analysed and interpreted the data. RZ, ZX and YX drafted the manuscript. ML, TW, ZZ, MX, JL, MD, DZ, YC, SW, HL, WW, GN, YB revised the manuscript for important intellectual content. All authors agreed to be held accountable for all aspects of this work and approved the final version of the manuscript. RZ, YB, and YX had full access to all the data in the study and had final responsibility for the decision to submit for publication. YX is responsible for the integrity of the work as a whole.
Funding
This work was supported by the grants from the National Natural Science Foundation of China (81870560, 8208810, 81970691, 81941017, 81770842, 81970706, 82022011, 82070880), the Shanghai Shenkang Hospital Development Center (SHDC12019101, SHDC2020CR1001A, SHDC2020CR3064B), the Shanghai Municipal Government (20Y11905100), Shanghai Jiaotong University School of Medicine (DLY201801) and the Ruijin Hospital (2018CR002).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM
(PDF 236 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, R., Xin, Z., Li, M. et al. Outdoor light at night in relation to glucose homoeostasis and diabetes in Chinese adults: a national and cross-sectional study of 98,658 participants from 162 study sites. Diabetologia 66, 336–345 (2023). https://doi.org/10.1007/s00125-022-05819-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05819-x