Abstract
Aims/hypothesis
Serum albumin concentrations may be associated with future risk of type 2 diabetes, but the epidemiological evidence is limited and uncertain. We prospectively assessed the association between baseline values of serum albumin and incident type 2 diabetes risk in the Kuopio Ischaemic Heart Disease population-based cohort study.
Methods
We analysed the data of 1,785 men aged 42–61 years with no known history of diabetes at baseline. Participants’ serum albumin concentrations were measured at baseline. HRs and 95% CIs for type 2 diabetes events were subsequently assessed.
Results
During a mean follow-up of 20.4 years, 382 participants developed diabetes. Serum albumin concentrations were weakly correlated with several established risk factors for diabetes. Serum albumin was approximately linearly associated with type 2 diabetes risk. In analyses adjusted for several conventional risk factors, the HR for type 2 diabetes per 1 SD increase in serum albumin was 1.15 (95% CI 1.03, 1.28; p = 0.016), which persisted after further adjustment for triacylglycerol, C-reactive protein, γ-glutamyltransferase, estimated glomerular filtration rate and total energy intake (HR 1.15; 95% CI 1.02, 1.29; p = 0.018). The findings were generally consistent across several clinical subgroups. Addition of information on serum albumin to a diabetes risk prediction model containing conventional risk factors led to no significant change in C-index (0.0126; 95% CI −0.0055, 0.0306; p = 0.17).
Conclusions/interpretation
A near linear, positive and independent association was found between serum albumin and type 2 diabetes, but this did not improve event discrimination. Further work is warranted to evaluate the causal relevance of these findings.
Similar content being viewed by others
Introduction
Serum albumin, which is synthesised in the liver [1], is a useful marker of nutritional status and known to possess antioxidative properties [2, 3]. It is able to scavenge peroxy radicals [4] and inhibits copper-dependent lipid peroxidation systems [5]. Low serum albumin has been suggested to be an indicator of inflammation and liver disease [6, 7]. Serum albumin concentrations have also been demonstrated to be inversely correlated with several risk factors for diabetes such as age and BMI [1, 5, 8]. In addition to its physiological functions, a growing body of evidence indicates that serum concentrations of albumin may be associated with a wide range of disease outcomes including metabolic syndrome [9, 10], cardiovascular morbidity and mortality [6, 11, 12], cancer mortality [6] and all-cause mortality [11].
Emerging evidence indicates that serum albumin concentrations may be linked to type 2 diabetes risk. A limited number of prospective studies have been published reporting on the associations between baseline serum albumin concentrations and risk of type 2 diabetes [8, 13, 14], but their results have been inconsistent. Whereas some studies have shown inverse associations [13, 14], other studies have found no association between serum albumin and type 2 diabetes [8, 13], giving rise to uncertainty regarding the nature of the association. To help characterise and quantify more reliably the nature and magnitude of the association, we report a detailed assessment of the association of serum albumin concentration with incident type 2 diabetes in a population-based sample of 1,785 non-diabetic men from eastern Finland. In addition, we also report the extent to which serum albumin measurements could improve the prediction of type 2 diabetes in general population settings when added to a conventional risk prediction model.
Methods
Study population
The study population consisted of a representative sample of men living in the city of Kuopio and its surrounding rural communities in eastern Finland. Subjects were participants in the Kuopio Ischaemic Heart Disease (KIHD) risk factor study, a longitudinal population-based study designed to investigate risk factors for cardiovascular disease (CVD), atherosclerosis and related outcomes [15]. Participants were 42–61 years of age during baseline examinations performed between March 1984 and December 1989. Of 3,433 potentially randomly eligible and randomly selected men, 2,682 (78%) volunteered to participate; 186 did not respond to the invitation and 367 declined to participate. Men with a prevalent self-reported history of diabetes, CVD, liver disease or kidney disease were excluded (n = 198). Prevalent diabetes was defined as having a clinical diagnosis of diabetes and regular treatment with diet, oral hypoglycaemic agents or insulin therapy. The final cohort for the present analysis included 1,785 men with non-missing information on serum albumin and with established and emerging risk factors for type 2 diabetes. An incident case of type 2 diabetes was defined as a fasting plasma glucose (FPG) ≥7.0 mmol/l, a 2 h glucose tolerance test plasma glucose ≥11.1 mmol/l, or use of glucose-lowering medication according to self-report at re-examination 4, 11 and 20 years after baseline and by record linkage to the national hospital discharge registry and to the Social Insurance Institution of Finland register for reimbursement of medicine expenses. The Research Ethics Committee of the University of Eastern Finland approved the study, and each participant gave written informed consent.
Risk factor assessment
Collection of blood specimens and the measurement of serum lipids, lipoproteins and glucose have been described previously [16]. Blood samples were taken between 08:00 and 10:00 hours. In addition to fasting, participants were instructed to abstain from drinking alcohol for at least 3 days and from smoking for at least 12 h prior to assessment. Measurement of serum albumin concentrations was made from frozen serum samples using Coulter’s bromcresol purple (BCP) colorimetric assay (Kone Specific, Kone Corporation, Espoo, Finland). The serum samples were stored frozen at −80°C for 0.2–2.5 years. FPG was measured by the glucose dehydrogenase method (Merck, Darmstadt, Germany). Serum γ-glutamyltransferase (GGT) activity was measured using the kinetic method (Thermo Fisher Scientific, Vantaa, Finland) and C-reactive protein (CRP) with an immunometric assay (Immulite High Sensitivity C-Reactive Protein Assay; DPC, Los Angeles, CA, USA). Smoking, alcohol consumption and blood pressure were assessed as described previously [16]. BMI was computed as the ratio of weight in kilograms to the square of height in metres. Dietary energy intake was assessed by recording food intake over 4 days using a questionnaire, and caloric intake of nutrients was calculated using Nutrica software (version 2.5; National Public Health Institute, Turku, Finland) [17]. Physical activity was assessed using the KIHD 12 month leisure-time physical activity questionnaire [17, 18].
Statistical analyses
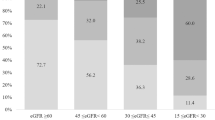
Values of positively skewed variables (e.g. triacylglycerols, CRP and GGT) were natural log-transformed to achieve normality. We performed descriptive analyses summarising the baseline characteristics of the participants. We assessed potential associations of serum albumin concentrations with risk markers for type 2 diabetes using linear regression models. Time-to-event analyses were conducted using Cox proportional hazards models to examine the association of serum albumin with incident type 2 diabetes after confirming assumption of proportionality of hazards. The shape of the association with type 2 diabetes risk was assessed by plotting HRs calculated within quartiles of baseline serum albumin concentration against the mean serum albumin concentration within each quartile. We used floating variances to calculate 95% CIs for the HR in each group, including the reference group, to allow for comparisons across the groups irrespective of the arbitrarily chosen reference category (bottom quartile) [19]. As the association showed an approximately linear shape, HRs were calculated per 1 SD higher serum albumin concentrations. The SD of the baseline serum albumin concentration was 3.6 g/l. HRs were adjusted for established type 2 diabetes risk factors (age, BMI, systolic blood pressure [SBP], smoking status, high-density lipoprotein cholesterol [HDL-C], physical activity, family history of diabetes and FPG) and further for log e triacylglycerol, log e CRP, log e GGT, estimated GFR (eGFR), as calculated using the Chronic Kidney Disease Epidemiology Collaboration formula [20], and total energy intake. We performed subgroup analyses using interaction tests to assess statistical evidence of any differences in HRs across levels of pre-specified individual level characteristics (such as age at survey, smoking status, BMI, SBP, FPG, HDL-C, eGFR and total energy intake). To avoid potential bias due to participants at high risk of diabetes or with underlying diabetes at baseline, we carried out additional analyses that excluded diabetes events ascertained in the first 5 years of follow-up.
To assess whether adding information on serum albumin values to conventional type 2 diabetes risk factors is associated with improvement in prediction of type 2 diabetes risk, we calculated measures of discrimination for censored time-to-event data (Harrell’s C-index [21]) and reclassification [22, 23]. To investigate the change in C-index on the addition of serum albumin, two diabetes risk prediction models were fitted: the 9 year Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR) risk model with several conventional risk factors (i.e. smoking, waist circumference and hypertension) [24], and the same model with the conventional risk factors plus serum albumin. We calculated the continuous net reclassification improvement (NRI) [23], a category-free version of the NRI, and the integrated discrimination improvement (IDI), which integrates the NRI over all possible cut-offs and is equivalent to the difference in discrimination slopes [22]. All statistical analyses were conducted using Stata version 12 (StataCorp LP, College Station, TX, USA).
Results
Baseline characteristics
In the KIHD study, data were available for 1,785 participants with no known history of diabetes at baseline. The mean age of the participants was 53 (SD 5) years. Baseline descriptive characteristics of the participants are shown in Table 1. During an average follow-up of 20.4 years (36,640 person-years at risk), there were 382 incident type 2 diabetes events (annual rate 11.1/1,000 person-years at risk; 95% CI 10.1, 12.3). Serum albumin concentrations were weakly and positively correlated with physical measures (BMI and blood pressure) and with several lipid and metabolic markers. Weak inverse correlations were observed for age (r = −0.12), total cholesterol (r = −0.04), log e CRP (r = −0.14) and log e eGFR (r = −0.08). Baseline serum albumin concentrations were lower by 63% in current smokers compared with non-current smokers (Table 1).
Serum albumin concentrations and risk of incident type 2 diabetes
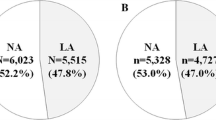
In analyses adjusted for established type 2 diabetes risk factors (age, BMI, SBP, smoking status, HDL-C, physical activity, family history of diabetes and FPG), there was an approximately linear association between serum albumin and type 2 diabetes risk (Fig. 1). Statistical tests of the compatibility of the data with a linear vs a quadratic model suggested a better fit with a linear shape (p for linearity <0.05). The age-adjusted HR per 1 SD change in serum albumin concentration was 1.14 (95% CI 1.03, 1.27; p = 0.013), which remained persistent (HR 1.15; 95% CI 1.03, 1.28; p = 0.016) after further adjusting for established risk factors. The results remained consistent after additionally adjusting for log e triacylglycerol, log e CRP, log e GGT, eGFR and total energy intake (HR 1.15; 95% CI 1.02, 1.29; p = 0.018) (Table 2). HRs did not vary importantly in analyses that excluded diabetes events ascertained in the first 5 years of follow-up (data not shown). The associations did not vary significantly by levels of several clinically relevant characteristics and other risk markers (p for interaction >0.10 for each; Fig. 2).
HRs (95% CI) for incident type 2 diabetes by quartiles of baseline concentrations of serum albumin, plotted on a logarithmic scale: (a) adjusted for age; (b) adjusted for age, BMI, SBP, smoking, HDL-C, physical activity, family history of type 2 diabetes and FPG. The figure shows the HR and 95% ‘floating absolute’ CIs per quartile of serum albumin concentrations. The size of the box is proportional to the inverse of the variance of HR. Note: the first category is the reference
Serum albumin concentration and type 2 diabetes risk prediction
A diabetes risk prediction model containing conventional risk factors yielded a C-index of 0.7614 (95% CI 0.7130, 0.8098). After addition of information on albumin in the model, the C-index was 0.7740 (95% CI 0.7261, 0.8219), representing a non-significant increase of 0.0126 (95% CI −0.0055, 0.0306; p = 0.17). The NRI and IDI were 15.8% (95% CI −5.1, 36.7; p = 0.11) and −0.00002 (95% CI −0.0027, 0.0027; p = 0.98), respectively (electronic supplementary material [ESM] Table 1).
Discussion
Our analyses of this population-based cohort of middle-aged men with over 20 years of follow-up and without a history of diabetes at baseline provide several relevant findings that have previously not been reported. There were weak associations of serum albumin concentrations with several established and emerging diabetes risk factors. Our data also suggest that baseline serum albumin concentration is positively and independently associated with incident type 2 diabetes in an approximately linear fashion. In addition, these findings remained generally consistent across several clinically relevant subgroups and at different levels of risk factors. The associations remained similar in analyses that excluded diabetes events ascertained in the first 5 years of follow-up.
Our finding of a positive association between serum albumin and type 2 diabetes is in contrast to the limited previous reports on an association (ESM Table 2). Abbasi and colleagues found no significant association in one of their cohorts of men and women aged 28–75 years [13]. In the Atherosclerosis Risk in Communities study [8], low serum albumin was associated with an increased risk of type 2 diabetes among men and women aged 45–65 years in analyses adjusted for several conventional risk factors; however, the association became non-significant on further adjustment for BMI and waist/hip ratio. In the 6 year longitudinal investigation of the Western New York Study, in which only 61 people met the case definition of incident type 2 diabetes [14], Stranges and colleagues reported a decreased risk of type 2 diabetes incidence with high (upper tertile) serum albumin concentrations. Similar to the finding of an inverse association between serum albumin concentration and type 2 diabetes in previous studies, other studies have demonstrated associations between serum albumin concentrations and outcomes such as cardiovascular disease [6, 11, 12], cancer mortality [6] and all-cause mortality [11]. Our findings of a positive association are at odds with previous findings. As to whether these previous observations reflect true associations remains unclear. Several reasons, however, could explain the conflicting results. First, previous studies were limited by the following: (1) inadequate power because of small sample sizes; (2) short follow-up durations; and (3) inability to fully examine the impact of adjustment for potential confounding. Second, there may be true differences, due to differences in study population characteristics such as age, sex, race or genetic background. Third, these differences may also be related to differences in the type of blood samples (serum or plasma) used for albumin measurements, assay methods for serum albumin, ascertainment and case definition of type 2 diabetes outcomes or a combination of all of these (ESM Table 2). Three out of all four previous studies employed the use of a bromcresol green (BCG) dye-binding assay, which is subject to non-specific interference from binding to non-albumin proteins and may overestimate the associations [25]. We, however, used the BCP assay, which agrees more closely with the gold standard of immunonephelometry [25]. Fourth, there are suggestions that low serum albumin concentrations may be an indicator of underlying subclinical disease (such as renal or liver disease, malnutrition and anaemia) [11, 14], which may produce spurious inverse associations with type 2 diabetes and other chronic conditions [26].
The current study differs in several important ways from previous studies, which enhances the reliability of the findings: (1) the analysis was based on a large dataset with adequate power to demonstrate the observed associations; (2) participants were selected from a nationally representative sample, with a high response rate; they were prospectively followed for an average period of 20 years and there was no loss to follow-up; (3) there was information on a comprehensive panel of lifestyle and biological markers to allow adequate adjustment for potential confounding; and (4) individuals with prevalent diabetes, CVD, liver disease or renal disease were excluded from the analyses; in addition, a sensitivity analysis excluded diabetes events in the first 5 years of follow-up, thus minimising the effects of any pre-existing disease on serum albumin concentrations (‘reverse causation’) and therefore more closely reflecting a causal association. In addition, given that several previous studies have demonstrated positive associations between serum albumin and the metabolic syndrome [9, 10] (a known risk factor for type 2 diabetes [27, 28]), it is possible that our findings may reflect true associations. Nonetheless, collaborative pooling of individual participant data from large-scale prospective studies with long follow-up durations may be needed to clarify the associations.
The mechanistic pathways for the link between elevated serum albumin and the development of type 2 diabetes are unclear, although a higher dietary protein intake has been suggested for the positive association between serum albumin and the metabolic syndrome [10]. Our findings did not suggest any evidence of effect modification by total dietary energy intake. If our findings of an independent and linear association between serum albumin and type 2 diabetes risk reflect a true association, it may have implications for the prevention of type 2 diabetes. Although several risk scores incorporating established risk factors for diabetes exist [29–31], their clinical utility has been questioned, as the identification of individuals at increased risk remains a difficult undertaking [32]. There is therefore stimulated interest in evaluating the relevance of additional risk factors. Serum albumin has been suggested as an emerging risk factor that may add to the identification of future diabetic patients beyond that of traditional risk factors [14]. Due to its limited and weak correlation with established risk factors, there is a potential for serum albumin to improve risk prediction over and above these established risk factors [32]. Although our results showed a graded increase in type 2 diabetes risk with increasing serum albumin concentrations, additional information on serum albumin provided no significant improvement in type 2 diabetes risk discrimination. Given that serum albumin is a simple, standardised, cost-effective and scalable biomarker, we propose additional larger studies and formal risk analyses (such as those conducted by our group [33, 34]) to assess its role in type 2 diabetes risk prediction.
In addition to the several strengths enumerated above, our study did have some limitations. The study included only men and the findings cannot necessarily be generalised to women. Although we accounted for many potential confounders including key clinical characteristics, liver and kidney function, and caloric intake, there was a potential for residual confounding, as with all observational studies. Furthermore, we could not correct for within-individual variation in serum albumin concentrations over time, which may have underestimated the associations demonstrated, as we had only a one-time measurement of serum albumin. Though there are suggestions that serum albumin exhibits low within-individual variation (the correlation coefficient between measured levels of serum albumin several years apart has been reported to be approximately 0.70 [1]), studies with repeat measurements of serum albumin are still needed to assess its variability in greater detail.
In summary, there is an approximately linear positive association between serum albumin concentration and incident type 2 diabetes risk, which is independent of established risk factors. However, no improvement in diabetes risk prediction was demonstrated. Further studies are needed to determine whether this relationship represents a causal association.
Abbreviations
- BCP:
-
Coulter’s bromcresol purple
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- eGFR:
-
Estimated GFR
- FPG:
-
Fasting plasma glucose
- GGT:
-
γ-glutamyltransferase
- HDL-C:
-
High-density lipoprotein cholesterol
- IDI:
-
Integrated discrimination improvement
- KIHD:
-
Kuopio Ischaemic Heart Disease
- NRI:
-
Net reclassification improvement
- SBP:
-
Systolic blood pressure
References
Danesh J, Collins R, Appleby P, Peto R (1998) Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA 279:1477–1482
Harris D, Haboubi N (2005) Malnutrition screening in the elderly population. J R Soc Med 98:411–414
Roche M, Rondeau P, Singh NR, Tarnus E, Bourdon E (2008) The antioxidant properties of serum albumin. FEBS Lett 582:1783–1787
Wayner DD, Burton GW, Ingold KU, Locke S (1985) Quantitative measurement of the total, peroxyl radical-trapping antioxidant capability of human blood plasma by controlled peroxidation. The important contribution made by plasma proteins. FEBS Lett 187:33–37
Gillum RF (2000) Assessment of serum albumin concentration as a risk factor for stroke and coronary disease in African Americans and whites. J Natl Med Assoc 92:3–9
Phillips A, Shaper AG, Whincup PH (1989) Association between serum albumin and mortality from cardiovascular disease, cancer, and other causes. Lancet 2:1434–1436
Wroblewski F, Ladue JS (1956) Serum glutamic pyruvic transaminase in cardiac with hepatic disease. Proc Soc Exp Biol Med 91:569–571
Schmidt MI, Duncan BB, Sharrett AR et al (1999) Markers of inflammation and prediction of diabetes mellitus in adults (Atherosclerosis Risk in Communities study): a cohort study. Lancet 353:1649–1652
Ishizaka N, Ishizaka Y, Nagai R, Toda E, Hashimoto H, Yamakado M (2007) Association between serum albumin, carotid atherosclerosis, and metabolic syndrome in Japanese individuals. Atherosclerosis 193:373–379
Cho HM, Kim HC, Lee JM, Oh SM, Choi DP, Suh I (2012) The association between serum albumin levels and metabolic syndrome in a rural population of Korea. J Prev Med Public Health 45:98–104
Djousse L, Rothman KJ, Cupples LA, Levy D, Ellison RC (2002) Serum albumin and risk of myocardial infarction and all-cause mortality in the Framingham Offspring Study. Circulation 106:2919–2924
Nelson JJ, Liao D, Sharrett AR et al (2000) Serum albumin level as a predictor of incident coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol 151:468–477
Abbasi A, Bakker SJ, Corpeleijn E et al (2012) Liver function tests and risk prediction of incident type 2 diabetes: evaluation in two independent cohorts. PLoS One 7:e51496
Stranges S, Rafalson LB, Dmochowski J et al (2008) Additional contribution of emerging risk factors to the prediction of the risk of type 2 diabetes: evidence from the Western New York Study. Obesity (Silver Spring) 16:1370–1376
Salonen JT (1988) Is there a continuing need for longitudinal epidemiologic research? The Kuopio Ischaemic Heart Disease Risk Factor Study. Ann Clin Res 20:46–50
Salonen JT, Nyyssonen K, Korpela H, Tuomilehto J, Seppanen R, Salonen R (1992) High stored iron levels are associated with excess risk of myocardial infarction in eastern Finnish men. Circulation 86:803–811
Laukkanen JA, Laaksonen D, Lakka TA et al (2009) Determinants of cardiorespiratory fitness in men aged 42 to 60 years with and without cardiovascular disease. Am J Cardiol 103:1598–1604
Lakka TA, Venalainen JM, Rauramaa R, Salonen R, Tuomilehto J, Salonen JT (1994) Relation of leisure-time physical activity and cardiorespiratory fitness to the risk of acute myocardial infarction. N Engl J Med 330:1549–1554
Easton DF, Peto J, Babiker AG (1991) Floating absolute risk: an alternative to relative risk in survival and case-control analysis avoiding an arbitrary reference group. Stat Med 10:1025–1035
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Pencina MJ, D'Agostino RB Sr, D'Agostino RB Jr, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–172, discussion 207–112
Pencina MJ, D'Agostino RB Sr, Steyerberg EW (2011) Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 30:11–21
Balkau B, Lange C, Fezeu L et al (2008) Predicting diabetes: clinical, biological, and genetic approaches: data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care 31:2056–2061
Gustafsson JE (1976) Improved specificity of serum albumin determination and estimation of "acute phase reactants" by use of the bromcresol green reaction. Clin Chem 22:616–622
Goldwasser P, Feldman J (1997) Association of serum albumin and mortality risk. J Clin Epidemiol 50:693–703
Sattar N, Gaw A, Scherbakova O et al (2003) Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation 108:414–419
Lorenzo C, Okoloise M, Williams K, Stern MP, Haffner SM, San Antonio Heart S (2003) The metabolic syndrome as predictor of type 2 diabetes: the San Antonio heart study. Diabetes Care 26:3153–3159
Kahn HS, Cheng YJ, Thompson TJ, Imperatore G, Gregg EW (2009) Two risk-scoring systems for predicting incident diabetes mellitus in U.S. adults age 45 to 64 years. Ann Intern Med 150:741–751
Wilson PW, Meigs JB, Sullivan L, Fox CS, Nathan DM, D'Agostino RB Sr (2007) Prediction of incident diabetes mellitus in middle-aged adults: the Framingham Offspring Study. Arch Intern Med 167:1068–1074
Griffin SJ, Little PS, Hales CN, Kinmonth AL, Wareham NJ (2000) Diabetes risk score: towards earlier detection of type 2 diabetes in general practice. Diabetes Metab Res Rev 16:164–171
Herder C, Karakas M, Koenig W (2011) Biomarkers for the prediction of type 2 diabetes and cardiovascular disease. Clin Pharmacol Ther 90:52–66
Emerging Risk Factors C, Kaptoge S, Di Angelantonio E et al (2012) C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med 367:1310–1320
Emerging Risk Factors C, Di Angelantonio E, Gao P et al (2014) Glycated hemoglobin measurement and prediction of cardiovascular disease. JAMA 311:1225–1233
Acknowledgements
We thank the staff of the Kuopio Research Institute of Exercise Medicine and the Research Institute of Public Health and University of Eastern Finland, Kuopio, Finland, who assisted in data collection in the study.
Funding
This work was supported by the Academy of Finland, Helsinki, Finland; City of Kuopio, Kuopio, Finland; Finnish Medical Foundation, Helsinki, Finland; and Finnish Cultural Foundation, Helsinki, Finland.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
SKK, HK and JAL participated in the conception and design of the study. SKK analysed the data. SKK, HK and JAL were involved in interpretation of data, and contributed to drafting the manuscript and revising it critically for important intellectual content. All authors approved the manuscript for submission. JAL supervised the study and is the guarantor of this work.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 75 kb)
ESM Table 2
(PDF 94 kb)
Rights and permissions
About this article
Cite this article
Kunutsor, S.K., Khan, H. & Laukkanen, J.A. Serum albumin concentration and incident type 2 diabetes risk: new findings from a population-based cohort study. Diabetologia 58, 961–967 (2015). https://doi.org/10.1007/s00125-015-3520-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-015-3520-0