Abstract
Aims/hypothesis
The role of increased gluconeogenesis as an important contributor to fasting hyperglycaemia at diabetes onset is not known. We evaluated the contribution of gluconeogenesis and glycogenolysis to fasting hyperglycaemia in newly diagnosed youths with type 2 diabetes following an overnight fast.
Methods
Basal rates (μmol kgFFM −1 min−1) of gluconeogenesis (2H2O), glycogenolysis and glycerol production ([2H5] glycerol) were measured in 18 adolescents (nine treatment naive diabetic and nine normal-glucose-tolerant obese adolescents).
Results
Type 2 diabetes was associated with higher gluconeogenesis (9.2 ± 0.6 vs 7.0 ± 0.3 μmol kgFFM −1 min−1, p < 0.01), plasma fasting glucose (7.0 ± 0.6 vs 5.0 ± 0.2 mmol/l, p = 0.004) and insulin (300 ± 30 vs 126 ± 31 pmol/l, p = 0.001). Glucose production and glycogenolysis were similar between the groups (15.4 ± 0.3 vs 12.4 ± 1.4 μmol kgFFM −1 min−1, p = 0.06; and 6.2 ± 0.8 vs 5.3 ± 0.7 μmol kgFFM −1 min−1, p = 0.5, respectively). After controlling for differences in adiposity, gluconeogenesis, glycogenolysis and glucose production were higher in diabetic youth (p ≤ 0.02). Glycerol concentration (84 ± 6 vs 57 ± 6 μmol/l, p = 0.01) and glycerol production (5.0 ± 0.3 vs 3.6 ± 0.5 μmol kgFFM −1 min−1, p = 0.03) were 40% higher in youth with diabetes. The increased glycerol production could account for only ~1/3 of substrate needed for the increased gluconeogenesis in diabetic youth.
Conclusion/interpretations
Increased gluconeogenesis was a major contributor to fasting hyperglycaemia and hepatic insulin resistance in newly diagnosed untreated adolescents and was an early pathological feature of type 2 diabetes. Increased glycerol availability may represent a significant source of new carbon substrates for increased gluconeogenesis but would not account for all the carbons required to sustain the increased rates.
Similar content being viewed by others
Introduction
Type 2 diabetes in youth is an emerging public health concern and based on current data in the United States, the incidence rates of type 2 diabetes in adolescents are expected to triple over the next 40 years [1]. Since youth onset type 2 diabetes is also a rapidly progressive disease, identifying the early pathophysiological abnormalities in diabetic youth is important for developing timely and effective therapeutic targets [2].
New onset type 2 diabetes is characterised by two hallmark features: decreased first phase insulin secretion and increased peripheral insulin resistance [3]. Increased hepatic glucose production, specifically gluconeogenesis, may also be a key element early in the development of glucose dysregulation [4, 5]. While some studies report increased gluconeogenesis as a late contributor to fasting hyperglycaemia in patients with long-standing type 2 diabetes [6–10], others demonstrate increased rates of gluconeogenesis in individuals with impaired fasting glucose as well as in the insulin resistant obese adolescent, prior to the onset of glucose intolerance [5, 11]. However, not all reports confirm increased hepatic glucose production as a major contributor to hyperglycaemia in type 2 diabetes [12, 13], and the contribution of gluconeogenesis and glycogenolysis to fasting hyperglycaemia in newly diagnosed individuals is unknown.
The present study was designed to determine whether increased gluconeogenesis and glycogenolysis are primary contributors to fasting hyperglycaemia in drug naive newly diagnosed adolescents with type 2 diabetes.
Methods
Participants
The protocol was approved by the Baylor College of Medicine Institutional Review Board for Human Subjects Research. Obese healthy adolescents (obese) with no family history of diabetes were recruited by local advertisement, and newly diagnosed obese adolescents with type 2 diabetes were recruited from the Texas Children’s Hospital Pediatric Diabetes Clinic. Adolescents were screened and enrolled in the study following written assent from the participant and consent from the legal guardian.
Seventy-seven adolescents, 10–17 years of age, were screened (22 obese and 55 youth with diabetes) of which 24 were eligible for participation (12 obese and 12 youth with type 2 diabetes). Eighteen adolescents, nine obese and nine with type 2 diabetes, met all the inclusion criteria and were studied within 2 weeks of initial screening and/or diagnosis and prior to diabetes treatment (Table 1). All participants were post pubertal (Tanner IV–V) and were not taking any medications, including birth control pills, at the time of the study. Prior to the tracer dilution study, each participant had their body composition measured to calculate rates of isotope administration based on their fat-free mass (FFM).
Youth with type 2 diabetes had symptoms of hyperglycaemia (polyuria, polydipsia and polyphagia) and phenotypic features of insulin resistance (obesity, acanthosis nigricans); type 2 diabetes was diagnosed using ADA criteria [14]. There was no evidence of ketosis or acidosis and all youth with type 2 diabetes had negative autoantibodies to glutamic acid decarboxylase, insulin and insulinoma-associated protein-2 (IA-2A). Once enrolled, all youth with type 2 diabetes received standard patient education and dietary instruction [14].
Obese control youth were matched for age, Tanner stage and BMI. Obese youth were in good health as determined by medical history, physical examination, standard blood chemistry analysis (haemoglobin/haematocrit, liver enzymes). Additionally, obese youth had a normal 75 g OGTT and no evidence of impaired glucose tolerance or diabetes at screening evaluation [15].
Study design
The participants were admitted to the Metabolic Research Unit at the Children’s Nutrition Research Center, Houston Texas at 07:00 hours on study day 1 after a 10 h overnight fast. All participants underwent an OGTT between 08:00 and 11:00 hours to measure plasma glucose and insulin concentrations. Subsequently all participants received lunch at 11:00 hours, dinner at 17:00 hours and a snack at 20:00 hours based on a standard 8,368 kJ/day (2,000 kcal/day) diet; 50% carbohydrates, 30% fat and 20% protein. Participants had ad libitum access to water and were fasted from 21:00 hours on study day 1 until the termination of the inpatient study at around 12:00 hours the following day. A 24 h urine collection was initiated at around 12:00 hours on study day 1 to measure nitrogen excretion to be able to partition the energy expenditure from fat, carbohydrate and protein. Measurements of oxygen consumption and carbon dioxide production via indirect calorimetry were performed during steady state on study day 2 between 07:00 and 07:30 hours. On study day 2, at time 0 (09:00 hours) a 0.35 g/kgFFM bolus of dextrose was infused over 2 min and frequent blood samples taken over the following 10 min to determine the acute insulin response to glucose (AIRg).
Tracers
Deuterium oxide (99% [2H]), [6,6-2H2]glucose (99% [2H]), [U-13C3]glycerol (99% [13C]) and [2H5]glycerol (95% [2H]) were purchased from Cambridge Isotope Laboratories (Andover, MA, USA). The isotopes were tested for sterility and pyrogenicity by the investigational pharmacy at Texas Children’s Hospital (Houston, TX, USA). The infusates were filtered through a Millex GP syringe filter (0.22 μm; Millipore Corporation, Bedford, MN, USA) and stored at 4°C for up to 48 h prior to administration.
Administration of tracers
Participants received 3.0 g/kgFFM of deuterium oxide [2H2O] given in four divided doses every 2 h (21:00 hours, 23:00 hours, 01:00 hours and 03:00 hours) to enrich the body water pool to approximately 0.3% 2H2O to measure fractional gluconeogenesis. At 04:00 hours the following morning, a simultaneous, primed (60 × the minute infusion rate), 5 h constant rate infusion was initiated with [6, 6-2H2]glucose (0.493 ± 0.001 μmol kgFFM −1 min−1) and [2H5]glycerol (0.154 ± 0.002 μmol kgFFM −1 min−1) to measure glucose and glycerol turnover, respectively. Two of the nine control participants were studied in an identical fashion as described above, except [U-13C3]glycerol (mean infusion rate 0.33 μmol kgFFM −1 min−1) was substituted for [2H5]glycerol.
Blood sampling
Blood samples were obtained at baseline and at −30, −20, −10 and 0 min during the last 30 min of the continuous tracer infusion to assess plasma glucose, insulin and C-peptide concentrations and isotopic enrichments. Plasma glucose and insulin samples for AIRg were obtained at 2, 3, 4, 5, 8 and 10 min after the bolus dextrose injection.
Analyses
Glucose and lactate concentrations were measured using a YSI model 2700 analyser (Yellow Springs Instrument, Yellow Springs, OH, USA). Total urinary nitrogen was measured by the modified Kjeldahl method using a Techicon II Autoautoanalyzer in a commercial laboratory (Texas A&M AgriLife Extension Service Soil, Water and Forage Testing Laboratory, College Station, TX, USA). Insulin concentrations were determined by electrochemiluminescence (Elecsys 1010 Analyzer, Roche Diagnostics Corporation, Indianapolis, IN, USA). NEFA concentrations were determined by colorimetric assay (ELISA kits, Linco Research, St Charles, MO, USA). Glucagon was measured by radioimmunoassay (Millipore, Billerica, MA, USA). Samples for glucagon and NEFA were available in seven of nine control participants. HbA1c was measured by DCA Vantage Analyzer (Siemens Medical Solutions Diagnostics, Tarrytown, NY, USA). All plasma and urine samples were stored at −80°C and then processed and analysed simultaneously.
Plasma glycerol concentration was measured by reverse isotope dilution using [2-13C]glycerol as previously described [16]. The enrichments of [2H5]glycerol, [2H2]glucose, [2H2O]water and [2H1]glucose were determined as previously described [16, 17]. Glycerol enrichment in plasma derived from [13C3]glycerol infusion was determined using positive chemical ionisation mass spectrometry, utilising the mass fragment m/z-159 amu and m/z-162 amu of glycerol triacetate derivative. The contribution of [13C3]glycerol to plasma glucose was measured using positive chemical ionisation mass spectrometry, utilising the mass fragment m/z-169 amu and m/z-172 amu of glucose pentaacetate derivative.
FFM and fat mass (FM) were measured by dual-energy x-ray absorptiometry (QDR 11.2; Hologic Bedford, MA, USA). Resting energy expenditure (REE) was assessed via indirect calorimetry using DELTATRAC II (Sensormedics, Yorba Linda, CA, USA). Non-protein respiratory quotient and macronutrient oxidation were computed using 24 h excretion of urinary nitrogen [18, 19].
Calculations
Rates of plasma glucose appearance and glycerol production were calculated under near steady-state conditions (−30 to 0 min) using the average enrichment of [6, 6-2H2]glucose and [2H5] glycerol or [U-13C3]glycerol, with conventional isotope dilution calculations [16]. Under fasting and steady-state conditions, rate of glucose appearance (Ra) is equivalent to glucose production. Fractional gluconeogenesis was determined using 2H2O and the average enrichment of 2H enrichments of carbon 1,3,4,5,6 of glucose [17]. Briefly, at total body enrichment of deuterium of 0.3%, the deuterium is incorporated into the covalently bound hydrogen (deuterium) at any of the carbons 1,3,4,5,6 of glucose during the process of gluconeogenesis. At this low enrichment, each glucose carbon will have approximately the same statistical opportunity of being labelled and only one hydrogen will be labelled on any single glucose molecule. After pentaacetate derivation of 25 μl of plasma, the deuterium-labelled fragment of glucose pentaacetate (m/z 169) is identified in the positive chemical ionisation scan mode of gas chromatograph mass spectrometry (GC-MS). Since body water is the precursor pool for the deuterium, the extent of deuterium labelling of glucose during the gluconeogenic process is a measure of fractional gluconeogenesis. The rate of gluconeogenesis was calculated as the product of glucose Ra and fractional gluconeogenesis (glucose Ra × % gluconeogenesis) and the rate of glycogenolysis was calculated as the glucose production rate minus the rate of gluconeogenesis.
Hepatic insulin sensitivity index (HISIGPR) was calculated in the fasting state: 1,000/ [glucose production (mg kgFFM −1 min−1) × plasma insulin concentration (μU/ml)] [20]. In addition, since glycogenolysis is the component of glucose production that is sensitive to changes in insulin concentration [21], we calculated another parameter of hepatic insulin sensitivity (HISGLY): 1,000/ [glycogenolysis (mg kgFFM −1 min−1) × plasma insulin concentration (μU/ml)].
Whole body insulin sensitivity (WBISI) was calculated from insulin and glucose concentrations obtained during the OGTT [20]. Areas under the curve for glucose and insulin concentrations during the OGTT were calculated by the trapezoidal rule. The AIRg was calculated as the AUC of insulin concentrations above baseline, for the 10 min after the acute bolus injection of dextrose.
Statistical methods
Data are presented as means ± SEM, unless otherwise stated. Differences between the two groups were tested by two-tailed t tests for continuous variables and χ 2 tests for categorical variables. Non-parametric data (insulin) were log transformed prior to analyses. Pearson correlation coefficients (r) were used to compare continuous variables. Analysis of covariance (ANCOVA) was performed with diabetes as the fixed effect and FM as a linear covariate. Statistics were performed using SPSS v. 22 (SPSS, Chicago, IL, USA). A p value <0.05 was considered statistically significant.
Results
Participant characteristics
The average age of the study population was 14.2 ± 0.5 years and it was 90% female. Weight, age and FFM were not different between the diabetic and obese control participants. Although the average FM and BMI in the youth with type 2 diabetes were greater than in obese controls, the two groups were not significantly different (Table 1). REE ( 8,611 ± 548 vs 7,540 ± 452 kJ/day, p = 0.2; 156 ± 30 vs 157 ± 12 kJ/kgFFM, p = 0.1), protein oxidation (57.1 ± 18.7 vs 58.7 ± 25.3 g day−1, p = 0.9) and non-protein respiratory quotient (0.84 ± 0.02 vs 0.83 ± 0.02, p = 0.4) were similar between youth with type 2 diabetes and obese controls, respectively.
Metabolic variables
During the OGTT, by definition, youth with type 2 diabetes had higher fasting plasma glucose and 2 h plasma glucose compared with obese youth (8.2 ± 0.7 vs 5.1 ± 0.1 mmol/l and 13.8 ± 1.1 vs 6.1 ± 0.1 mmol/l, p < 0.001, respectively). Fasting plasma insulin, glucose, glycerol, lactate and NEFA concentrations were also higher in youth with type 2 diabetes compared with obese controls, p < 0.01 (Table 1). In contrast, fasting plasma glucagon concentrations were similar in both groups (Table 1). The HbA1c in the adolescents with type 2 diabetes was 7.4 ± 0.3% (57 ± 3.3 mmol/mol). Adolescents with type 2 diabetes had lower WBISI (0.8 ± 0.1 vs 3.0 ± 0.6, p = 0.001) and lower AIRg (282 ± 163 vs 1,529 ± 410 [mU l]−1 min, p < 0.01).
Kinetic measurements
Isotopic enrichments of [6,6-2H2]glucose, [2H5]glycerol, [U-13C3]glycerol, average 2H per glucose carbon and 2H in body water under substrate and isotopic steady-state conditions for all participants are given in Table 2.
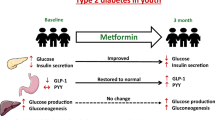
Glycogenolysis was similar (6.2 ± 0.8 vs 5.3 ± 0.7 μmol kgFFM −1 min−1, p = 0.5), but gluconeogenesis was higher in youth with type 2 diabetes compared with obese controls (9.2 ± 0.6 vs 7.0 ± 0.3 μmol kgFFM −1 min−1, p < 0.01; Fig. 1). Increased gluconeogenesis was the major contributor to higher rates of glucose production in youth with type 2 diabetes compared with obese controls (15.4 ± 0.3 vs 12.4 ± 1.4 μmol kgFFM −1 min−1, p = 0.06). ANCOVA analysis was performed to examine the effect of diabetes on glucose production and gluconeogenesis, with FM as the linear covariate. After adjusting for FM, gluconeogenesis, glucose production and glycogenolysis were higher in type 2 diabetes (p = 0.007, p = 0.002 and p = 0.02, respectively). Glycerol production was higher in youth with type 2 diabetes compared with obese (5.0 ± 0.3 vs 3.6 ± 0.5 μmol kgFFM −1 min−1, p = 0.03; Fig. 1). After statistically adjusting for FM, glycerol production remained higher in youth with type 2 diabetes, p = 0.04.
Basal rates of glycogenolysis, gluconeogenesis and glycerol turnover (Ra) in adolescents with type 2 diabetes and obese youth. The higher glycerol turnover in type 2 diabetes (0.15 mg kgFFM −1 min−1) could account for one third of their increased rates of gluconeogenesis (0.4 mg kgFFM −1 min−1). White bars, controls; black bars, type 2 diabetes. **p < 0.01 vs obese control
Gluconeogenesis correlated with fasting plasma glucose (r = 0.79, p < 0.001), glycerol (r = 0.54, p = 0.02), NEFA (r = 0.58, p = 0.02) and lactate (r = 0.55, p = 0.02), but not with fasting insulin (r = 0.4, p = 0.1), glucagon (r = −0.07, p = 0.8) or insulin:glucagon ratio (r = 0.47, p = 0.07). There was a trend for fasting glucose to correlate with glucose production (r = 0.47, p = 0.05), but not with glycogenolysis (r = 0.28, p = 0.27). Neither glucose production nor glycogenolysis correlated with fasting insulin, glycerol, NEFA, lactate, glucagon or insulin:glucagon ratio (data not shown).
Hepatic insulin sensitivity was lower in youth with type 2 diabetes (HISIGPR [using Matsuda index]: 7.8 ± 0.8 vs 32.9 ± 8.2, p < 0.001; and HISGLY [using the rate of glycogenolysis]: 20.8 ± 3.9 vs 84.2 ± 21.1, p = 0.001).
Discussion
The present study demonstrates that newly diagnosed and drug naive adolescents with type 2 diabetes had higher rates of gluconeogenesis than obese controls, a difference that was maintained after adjusting for body fat. Increased gluconeogenesis was an early pathological finding in newly diagnosed youth with type 2 diabetes despite mild fasting hyperglycaemia (~7 mmol/l). Rates of total glucose production and glycogenolysis were also higher in type 2 diabetes, but only after adjusting for FM (p ≤ 0.02). Since the absolute difference in glycogenolysis between the two groups was small, we conclude that the primary contributor to fasting hyperglycaemia in these newly diagnosed adolescents with type 2 diabetes was the 40% increase in gluconeogenesis and not the 17% increase in glycogenolysis.
Our study is the first to document increased rates of gluconeogenesis at the time of diagnosis and prior to therapeutic interventions. These findings contrast with prior studies in adults in which increased rates of gluconeogenesis were evident only in patients with long-standing disease who had marked fasting hyperglycaemia (>8 mmol/l) and were on glucose-lowering drugs [6, 22, 23]. With the use of a sensitive and highly reproducible technique, the average deuterium method, we now provide evidence that increased gluconeogenesis is unique and present very early in the pathophysiology of type 2 diabetes.
Furthermore, our data support earlier reports by our group and others, which demonstrated increased gluconeogenesis in normoglycaemic obese insulin resistant individuals [6, 7, 11, 22] and in those with impaired fasting hyperglycaemia [4, 5]. Collectively, these findings describe a progressive impairment in the regulation of gluconeogenesis along the continuum from obesity-induced insulin resistance, to impaired fasting hyperglycaemia, to type 2 diabetes.
We also investigated the effect of FM on rates of gluconeogenesis and the plasma concentrations of potential gluconeogenic substrates and precursors. Youth with type 2 diabetes had higher plasma substrate concentrations compared with otherwise healthy obese youth (Table 2). However, there were no correlations of FM with lactate, glycerol, NEFA, glycerol Ra, gluconeogenesis or glucose production. Therefore, the increased rate of gluconeogenesis in type 2 diabetes was not simply a result of increased FM, but likely mediated by other factors.
Increased gluconeogenesis was accompanied with reduced total body insulin sensitivity as reflected by the two- to threefold higher fasting plasma insulin concentrations, lower WBISI and more specifically, lower hepatic insulin sensitivity as measured by two indices. Rates of glycogenolysis were also mildly increased and explained by incompletely compensated hepatic insulin resistance in type 2 diabetes. This is supported by our measure of hepatic insulin sensitivity (HISGLY), which detects early derangements in the direct actions of insulin on glycogenolysis and provides a specific measure of hepatic insulin action.
However, the physiological or pathophysiological mechanism(s) governing increased gluconeogenesis in type 2 diabetes is unclear. Many have speculated that insulin has an inhibitory effect on gluconeogenesis based on changes in the expression of mRNA of the rate limiting gluconeogenic enzymes in animal models [24, 25]. Yet, gluconeogenesis is a complex process that involves multiple enzymatic steps, none of which are directly regulated by insulin [26, 27]. Carefully conducted studies in humans have failed to demonstrate inhibition of gluconeogenesis under conditions of mild to moderate hyperinsulinaemia, whether as the result of oral ingestion of a carbohydrate containing meal or infused insulin as part of a hyperinsulinaemic euglycaemic clamp study [21, 28–30]. During hyperinsulinaemic euglycaemic clamps at physiological to high physiological insulin concentrations, there was complete suppression of glycogenolysis, but only a 20% decrease in gluconeogenesis in obese individuals and those with type 2 diabetes [6, 7, 28]. These changes occurred despite complete suppression of fatty acid oxidation and insulin’s well-known effect on suppression of lipolysis [6, 7, 31]. Therefore, factors other than insulin must be involved in the regulation of hepatic gluconeogenesis during times of hyperinsulinaemia.
Another potential factor in the regulation of hepatic gluconeogenesis is the increased availability of circulating gluconeogenic substrates (e.g. lactate and glycerol) [32]. In normal individuals, increased substrate availability as a result of infusions of glycerol and lactate infusions increased the fractional contribution of carbon sources for glucose production, but had no effect on the total rate of glucose production [33]. However, in type 2 diabetes, increased lipolysis and proteolysis resulted in greater availability of potential gluconeogenic substrates—glycerol (lipolysis) and amino acids (proteolysis)—which may have resulted in higher rates of glucose production [34, 35]. It should be pointed out that gluconeogenesis was not specifically measured in these latter studies. Our current results support a role for increased substrate availability in regulating gluconeogenesis as we demonstrated that glycerol turnover and the plasma concentrations of glycerol and lactate increased by 30 to 40% in type 2 diabetes. However, if the total mass of the increase in glycerol carbon was shunted exclusively into the gluconeogenic pathway, glycerol would account for only one third of the increased gluconeogenesis observed (0.15 of 0.4 mg kgFFM −1 min−1, Fig. 1).
Since increased glycerol availability would account for up to 1/3 of increased gluconeogenesis, other gluconeogenic substrates contribute to (but may not drive) this process. Although not measured in the present study, the other carbon sources for glucose production from gluconeogenesis would be lactate (via increased Cori cycle activity) and/or amino acids (via shunting of amino acid carbons to gluconeogenesis via the tri-carboxylic [TCA] cycle). Studies using 14C-lactate and 14C-alanine demonstrated that these substrates could contribute up to 50% and 6% of carbons, respectively [36], although it is unclear if this was associated with an overall increase in gluconeogenesis. Lactate and alanine enter the gluconeogenic pathway via the TCA cycle and would contribute to gluconeogenesis primarily by recycling of glucose carbons [37]. Glycerol, on the other hand, is a unique gluconeogenic substrate because it enters the pathway at the level of the triose phosphates and could be an important contributor of new carbons to the gluconeogenic pool [34, 35]. Despite correlations of gluconeogenesis with increased substrate, simple availability of these gluconeogenesis precursors would only play a passive role in driving the gluconeogenic process and needs further investigation.
Increased hepatic fat is a more likely causative factor for the increased gluconeogenesis observed in individuals with obesity [6, 22] and type 2 diabetes [38]. At the level of the liver, increased hepatic fat and NEFA availability may have profound effects on both lipid and glucose metabolism. Increased NEFA oxidation increases intracellular acetyl coenzyme A concentrations, which in turn would inhibit pyruvate dehydrogenase, activate pyruvate carboxylase and drive substrates towards the gluconeogenic pathway to glucose [32].
Our current findings support a strong positive correlation of plasma NEFA with gluconeogenesis. Although we did not measure hepatic fat in this study, we previously demonstrated fourfold higher hepatic fat content in obese compared with lean adolescents. Furthermore, after a supervised and precisely executed 12 week aerobic exercise programme, obese adolescents had improved hepatic insulin sensitivity associated with a 40% reduction in hepatic fat and decreased rates of glycogenolysis [39, 40]. Yet, despite the reduction in hepatic fat, the absolute intrahepatic triacylglycerol content remained high (>5.6%) [39] perhaps explaining why rates of gluconeogenesis remained unchanged [40]. Hepatic fat content also correlates with metabolites of gluconeogenesis [41] and rates of TCA cycle flux into gluconeogenesis (U-13C propionate) were 50% higher in individuals with high (>6%) intrahepatic fat [42]. Together, these studies suggest an association between gluconeogenesis and intrahepatic fat content but the underlying pathophysiological mechanisms and the potential role of NEFA in this process remains elusive.
An important strength of our study is the use of the average deuterium method to demonstrate the early dysregulation of gluconeogenesis in type 2 diabetes. Older published methods (14C labelled alanine, lactate or glycerol) were only able to quantify the fraction of gluconeogenesis from the substrate labelled with the infused tracer. Only with the use of [2-13C] glycerol, C-5 [2H]glucose [43], the U-13C glucose method [13, 44] and average deuterium method [17], were quantitative rates of total gluconeogenesis possible. It is also important to note that there is no gold standard for measurements of gluconeogenesis and all of these measurements are semi-quantitative and most useful for intra-study comparisons.
The average deuterium method used in this study is comparable with the C5-HMT Landau method that measures the enrichment of deuterium on carbon 5 of the glucose molecule [17]. However, deuterium labelling may occur on different glucose carbons for the same substrate and in the same carbon for several substrates [45, 46]. Our method assumes equal distribution of deuterium labelling at all glucose carbons, except for C2, which undergoes glucose cycling [43]. By measuring the overall deuterium incorporation in covalently bonded C-H (except C-2), our method ignores small differences in labelling at different carbons of glucose [17]. With the use of our sensitive, highly reproducible (CV < 3%) and analytically easy technique, we provide evidence that increased gluconeogenesis is an early feature in type 2 diabetes that can be detected at disease onset.
Furthermore, our findings of increased gluconeogenesis in youth are representative of the adolescent population with type 2 diabetes since type 2 diabetes in youth is three to four times more prevalent in adolescent girls compared with boys [47]. Although several studies have reported no sex differences in fasting glucose production [48, 49] in healthy adults, a more recent study reports lower fasting glucose production in women [50]. Therefore, additional studies may be required to confirm this latter finding and its relationship to our findings of increased rates of gluconeogenesis in adolescents with new onset diabetes.
In conclusion, increased gluconeogenesis is a primary pathophysiological finding in drug naive adolescents with newly diagnosed type 2 diabetes, and contributes to their hepatic insulin resistance and fasting hyperglycaemia. Glycerol may be an important contributor of new carbons to gluconeogenesis but would account for only one third of the increased rate observed between adolescents with obesity and those with type 2 diabetes. Future research studies should focus on the role of intrahepatic fat in the regulation of gluconeogenesis.
Abbreviations
- AIRg:
-
Acute insulin response to glucose
- FFM:
-
Fat-free mass
- FM:
-
Fat mass
- HIS:
-
Hepatic insulin sensitivity
- HISI:
-
Hepatic insulin sensitivity index
- Ra:
-
Rate of appearance
- REE:
-
Resting energy expenditure
- TCA:
-
Tri-carboxylic
- WBISI:
-
Whole body insulin sensitivity
References
Imperatore G, Boyle J, Thompson T et al (2012) Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care 35:2515–2520
Dart A, Martens P, Rigatto C, Brownell M, Dean H, Sellers E (2014) Earlier onset of complications in youth with type 2 diabetes. Diabetes Care 37:436–443
Defronzo R (2009) Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 58:773–795
Bock G, Chittilapilly E, Basu R et al (2007) Contribution of hepatic and extrahepatic insulin resistance to the pathogenesis of impaired fasting glucose: role of increased rates of gluconeogenesis. Diabetes 56:1703–1711
Basu R, Barosa C, Jones J et al (2013) Pathogenesis of prediabetes: role of the liver in isolated fasting hyperglycemia and combined fasting and postprandial hyperglycemia. J Clin Endocrinol Metab 98:E409–E417
Basu R, Chandramouli V, Dicke B, Landau B, Rizza R (2005) Obesity and type 2 diabetes impair insulin-induced suppression of glycogenolysis as well as gluconeogenesis. Diabetes 54:1942–1948
Gastaldelli A, Baldi S, Pettiti M et al (2000) Influence of obesity and type 2 diabetes on gluconeogenesis and glucose output in humans: a quantitative study. Diabetes 49:1367–1373
Basu R, Basu A, Johnson CM, Schwenk WF, Rizza RA (2004) Insulin dose-response curves for stimulation of splanchnic glucose uptake and suppression of endogenous glucose production differ in nondiabetic humans and are abnormal in people with type 2 diabetes. Diabetes 53:2042–2050
Rizza RA (2010) Pathogenesis of fasting and postprandial hyperglycemia in type 2 diabetes: implications for therapy. Diabetes 59:2697–2707
Bacha F, Lee S, Gungor N, Arslanian S (2010) From pre-diabetes to type 2 diabetes in obese youth: pathophysiological characteristics along the spectrum of glucose dysregulation. Diabetes Care 33:2225–2231
Sunehag AL, Toffolo G, Campioni M, Bier DM, Haymond MW (2005) Effects of dietary macronutrient intake on insulin sensitivity and secretion and glucose and lipid metabolism in healthy, obese adolescents. J Clin Endocrinol Metab 90:4496–4502
Pigon J, Giacca A, Ostenson CG, Lam L, Vranic M, Efendic S (1996) Normal hepatic insulin sensitivity in lean, mild noninsulin-dependent diabetic patients. J Clin Endocrinol Metab 81:3702–3708
Tayek JA, Katz J (1996) Glucose production, recycling, and gluconeogenesis in normals and diabetics: a mass isotopomer [U-13C]glucose study. Am J Physiol 270:E709–E717
ADA (2011) Standards of medical care in diabetes—2011. Diabetes Care 34(Suppl 1):S11–S61
ADA (2011) Update of ADA’s major position statement, “Standards of Medical Care in Diabetes” Introduction. Diabetes Care 34(Suppl 1):S1–S2
Sunehag AL, Treuth MS, Toffolo G et al (2001) Glucose production, gluconeogenesis, and insulin sensitivity in children and adolescents: an evaluation of their reproducibility. Pediatr Res 50:115–123
Chacko S, Sunehag A, Sharma S, Sauer PJJ, Haymond M (2008) Measurement of gluconeogenesis using glucose fragments and mass spectrometry after ingestion of deuterium oxide. J Appl Physiol 104:944–951
Ferrannini E (1988) The theoretical bases of indirect calorimetry: a review. Metab Clin Exp 37:287–301
Livesey G, Elia M (1988) Estimation of energy expenditure, net carbohydrate utilization, and net fat oxidation and synthesis by indirect calorimetry: evaluation of errors with special reference to the detailed composition of fuels. Am J Clin Nutr 47:608–628
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–1470
Kaplan W, Sunehag AL, Dao H, Haymond MW (2008) Short-term effects of recombinant human growth hormone and feeding on gluconeogenesis in humans. Metab Clin Exp 57:725–732
Gastaldelli A, Miyazaki Y, Pettiti M et al (2004) Separate contribution of diabetes, total fat mass, and fat topography to glucose production, gluconeogenesis, and glycogenolysis. J Clin Endocrinol Metab 89:3914–3921
Wajngot A, Chandramouli V, Schumann WC et al (2001) Quantitative contributions of gluconeogenesis to glucose production during fasting in type 2 diabetes mellitus. Metab Clin Exp 50:47–52
Wan M, Leavens K, Hunter R et al (2013) A noncanonical, GSK3-independent pathway controls postprandial hepatic glycogen deposition. Cell Metab 18:99–105
Stark R, Guebre Egziabher F, Zhao X et al (2014) A role for mitochondrial phosphoenolpyruvate carboxykinase (PEPCK-M) in the regulation of hepatic gluconeogenesis. J Biol Chem 289:7257–7263
Saltiel AR, Kahn CR (2001) Insulin signalling and the regulation of glucose and lipid metabolism. Nature 414:799–806
Lin H, Accili D (2011) Hormonal regulation of hepatic glucose production in health and disease. Cell Metab 14:9–19
Gastaldelli A, Toschi E, Pettiti M et al (2001) Effect of physiological hyperinsulinemia on gluconeogenesis in nondiabetic subjects and in type 2 diabetic patients. Diabetes 50:1807–1812
Adkins A, Basu R, Persson M et al (2003) Higher insulin concentrations are required to suppress gluconeogenesis than glycogenolysis in nondiabetic humans. Diabetes 52:2213–2220
Tigas S, Sunehag A, Haymond M (2002) Metabolic adaptation to feeding and fasting during lactation in humans. J Clin Endocrinol Metab 87:302–307
Boden G, Chen X, Capulong E, Mozzoli M (2001) Effects of free fatty acids on gluconeogenesis and autoregulation of glucose production in type 2 diabetes. Diabetes 50:810–816
Hue L, Taegtmeyer H (2009) The Randle cycle revisited: a new head for an old hat. Am J Physiol Endocrinol Metab 297:E578–E591
Jahoor F, Klein S, Wolfe R (1992) Mechanism of regulation of glucose production by lipolysis in humans. Am J Physiol 262:E353–E358
Nurjhan N, Consoli A, Gerich J (1992) Increased lipolysis and its consequences on gluconeogenesis in non-insulin-dependent diabetes mellitus. J Clin Invest 89:169–175
Puhakainen I, Koivisto VA, Yki Järvinen H (1992) Lipolysis and gluconeogenesis from glycerol are increased in patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 75:789–794
Jenssen T, Nurjhan N, Consoli A, Gerich JE (1990) Failure of substrate-induced gluconeogenesis to increase overall glucose appearance in normal humans. Demonstration of hepatic autoregulation without a change in plasma glucose concentration. J Clin Invest 86:489–497
Consoli A, Nurjhan N, Reilly JJ, Bier DM, Gerich JE (1990) Mechanism of increased gluconeogenesis in noninsulin-dependent diabetes mellitus. Role of alterations in systemic, hepatic, and muscle lactate and alanine metabolism. J Clin Invest 86:2038–2045
Gastaldelli A, Cusi K, Pettiti M et al (2007) Relationship between hepatic/visceral fat and hepatic insulin resistance in nondiabetic and type 2 diabetic subjects. Gastroenterology 133:496–506
van der Heijden G-J, Wang Z, Chu Z et al (2010) A 12-week aerobic exercise program reduces hepatic fat accumulation and insulin resistance in obese, Hispanic adolescents. Obesity 18:384–390
van der Heijden G-J, Toffolo G, Manesso E, Sauer PJJ, Sunehag A (2009) Aerobic exercise increases peripheral and hepatic insulin sensitivity in sedentary adolescents. J Clin Endocrinol Metab 94:4292–4299
Sharma R, Sinha S, Danishad KA et al (2009) Investigation of hepatic gluconeogenesis pathway in non-diabetic Asian Indians with non-alcoholic fatty liver disease using in vivo ((31)P) phosphorus magnetic resonance spectroscopy. Atherosclerosis 203:291–297
Sunny N, Parks E, Browning J, Burgess S (2011) Excessive hepatic mitochondrial TCA cycle and gluconeogenesis in humans with nonalcoholic fatty liver disease. Cell Metab 14:804–810
Landau BR, Wahren J, Chandramouli V, Schumann WC, Ekberg K, Kalhan SC (1996) Contributions of gluconeogenesis to glucose production in the fasted state. J Clin Invest 98:378–385
Haymond MW, Sunehag AL (2000) The reciprocal pool model for the measurement of gluconeogenesis by use of [U-(13)C]glucose. Am J Physiol Endocrinol Metab 278:E140–E145
Landau BR, Wahren J, Chandramouli V, Schumann WC, Ekberg K, Kalhan SC (1995) Use of 2H2O for estimating rates of gluconeogenesis. Application to the fasted state. J Clin Invest 95:172–178
Rose IA (1975) Mechanism of the aldose-ketose isomerase reactions. Adv Enzymol Relat Areas Mol Biol 43:491–517
(2004) SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials 25: 458-471
Clore JN, Glickman PS, Helm ST, Nestler JE, Blackard WG (1989) Accelerated decline in hepatic glucose production during fasting in normal women compared with men. Metab Clin Exp 38:1103–1107
Robertson MD, Livesey G, Mathers JC (2002) Quantitative kinetics of glucose appearance and disposal following a 13C-labelled starch-rich meal: comparison of male and female subjects. Br J Nutr 87:569–577
Anderwald C, Gastaldelli A, Tura A et al (2011) Mechanism and effects of glucose absorption during an oral glucose tolerance test among females and males. J Clin Endocrinol Metab 96:515–524
Acknowledgements
We thank the volunteers (and their families) whose participation made this study possible. We gratefully acknowledge S. Sharma (Department of Pediatrics, Baylor College of Medicine, Houston, TX, USA) who facilitated data acquisition and study execution and X. Zhao (National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, USA) who assisted with statistical analyses. We thank Texas A&M AgriLife Extension Service Soil, Water and Forage Testing Laboratory, USA and Quest Diagnostic Laboratories, USA for their laboratory assistance in measuring urinary nitrogen and HbA1c, respectively.
Funding
This project was supported by National Institutes of Health grants RO1DK 55478 (MWH), USDA/ARS 6250-5100 (MWH) and the Marilyn Fishman Endocrine Fellows Foundation grant (STC). STC is currently supported by the intramural programme of the National Institute of Diabetes, Digestive Disorders and Kidney Diseases at the National Institutes of Health, Bethesda, MD, USA. This work is a publication of the USDA/ARS Children’s Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine (Houston, TX, USA). The contents of this publication do not necessarily reflect the views of policies of the U.S. Department of Agriculture, nor does mention of trade names, commercial products, or organisations imply endorsement from the US Government.
Duality of interest
STC and DSH are currently employed by National Institutes of Health, Bethesda, MD, USA and the Pennington Biomedical Research Center, Baton Rouge, LA, USA, respectively. All other authors declare that there is no duality of interest associated with their contribution to this manuscript.
Contribution statement
STC and MWH contributed to the conceptualisation, design, acquisition, analysis and interpretation of data, and writing of the manuscript. SKC contributed to the design and analysis of data and to the critical revision of the manuscript for important intellectual content. DSH and LMR contributed to the design, acquisition of data and to the critical revision of the manuscript for important intellectual content. All authors gave final approval of the version to be published. MWH is the guarantor of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, S.T., Hsia, D.S., Chacko, S.K. et al. Increased gluconeogenesis in youth with newly diagnosed type 2 diabetes. Diabetologia 58, 596–603 (2015). https://doi.org/10.1007/s00125-014-3455-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3455-x