Abstract
Aims/hypothesis
Maternal obesity leads to increased adiposity, hyperlipidaemia and glucose intolerance in offspring. The analogue of glucagon-like peptide-1, exendin-4 (Ex-4), has been shown to induce weight loss in both adolescence and adulthood. We hypothesised that, in rats, daily injection of Ex-4 would reduce body fat and improve metabolic disorders in offspring from obese dams, especially those consuming a high-fat diet (HFD).
Methods
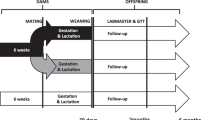
Female Sprague Dawley rats were fed chow or an HFD for 5 weeks before mating, and throughout gestation and lactation. At postnatal day 20, male pups from HFD-fed mothers were weaned onto chow or HFD and those from chow-fed mothers were fed chow. Within each dietary group, half of the pups were injected with Ex-4 (15 μg/kg/day i.p.) for 6 weeks, while the other half received saline.
Results
Maternal obesity alone or combined with postweaning HFD consumption led to increased adiposity, hyperinsulinaemia, hyperlipidaemia, inflammation and impaired regulation of hypothalamic appetite regulators by glucose in offspring, while glucose intolerance was only observed in HFD-fed rats from obese dams. Ex-4 injection significantly reduced adiposity, hyperlipidaemia and insulin resistance in HFD-fed rats from obese dams. It also restored glucose tolerance and the lipid-lowering effect of blood glucose. However, Ex-4 did not change hypothalamic appetite regulation or the response of appetite regulators to hyperglycaemia. Liver and adipose inflammatory cytokine expression was significantly reduced by Ex-4.
Conclusions/interpretation
Ex-4 reversed the detrimental impact of maternal obesity on lipid and glucose metabolism in offspring regardless of diet, supporting its potential application in reducing metabolic disorders in high-risk populations.



Similar content being viewed by others
Abbreviations
- Arc:
-
Arcuate nucleus
- BW:
-
Body weight
- C-C:
-
Pups from lean dams fed standard rodent chow diet and injected with saline
- C-C+E:
-
Pups from lean dams fed standard rodent chow diet and injected with exendin-4
- Ex-4:
-
Exendin-4
- GLP-1:
-
Glucagon-like peptide-1
- H-C:
-
Pups from HFD-fed dams fed chow and injected with saline
- H-C+E:
-
Pups from HFD-fed dams fed chow and injected with exendin-4
- HFD:
-
High-fat diet
- H-H:
-
Pups from HFD-fed dams fed HFD and injected with saline
- H-H+E:
-
Pups from HFD-fed dams fed HFD and injected with exendin-4
- IPGTT:
-
Intraperitoneal glucose tolerance test
- mTOR:
-
Mammalian target of rapamycin
- NPY:
-
Neuropeptide Y
- POMC:
-
Proopiomelanocortin
- PVN:
-
Paraventricular nucleus
- Rp:
-
Retroperitoneal
References
Muhlhausler BS (2007) Programming of the appetite-regulating neural network: a link between maternal overnutrition and the programming of obesity? J Neuroendocrinol 19:67–72
Chen H, Iglesias MA, Caruso V, Morris MJ (2011) Maternal cigarette smoke exposure contributes to glucose intolerance and decreased brain insulin action in mice offspring independent of maternal diet. PLoS One 6:e27260
Oben JA, Mouralidarane A, Samuelsson AM et al (2010) Maternal obesity during pregnancy and lactation programs the development of offspring non-alcoholic fatty liver disease in mice. J Hepatol 52:913–920
Kirk SL, Samuelsson AM, Argenton M et al (2009) Maternal obesity induced by diet in rats permanently influences central processes regulating food intake in offspring. PLoS ONE 4:e5870
Grayson BE, Levasseur PR, Williams SM, Smith MS, Marks DL, Grove KL (2010) Changes in melanocortin expression and inflammatory pathways in fetal offspring of nonhuman primates fed a high-fat diet. Endocrinology 151:1622–1632
McIntyre HD, Gibbons KS, Flenady VJ, Callaway LK (2012) Overweight and obesity in Australian mothers: epidemic or endemic? Med J Aust 196:184–188
Kim SY, Dietz PM, England L, Morrow B, Callaghan WM (2007) Trends in pre-pregnancy obesity in nine states, 1993–2003. Obesity (Silver Spring) 15:986–993
Stefater MA, Seeley RJ (2010) Central nervous system nutrient signaling: the regulation of energy balance and the future of dietary therapies. Annu Rev Nutr 30:219–235
Sarbassov DD, Ali SM, Sabatini DM (2005) Growing roles for the mTOR pathway. Curr Opin Cell Biol 17:596–603
Cota D, Proulx K, Smith KA et al (2006) Hypothalamic mTOR signaling regulates food intake. Science 312:927–930
Chen H, Simar D, Morris MJ (2013) Maternal obesity impairs hypothalamic glucose metabolism and appetite regulators in rat offspring. J Neurochem. doi:10.1111/jnc.12623
Chen H, Morris MJ (2009) Differential responses of orexigenic neuropeptides to fasting in offspring of obese mothers. Obesity 17:1356–1362
Chen H, Simar D, Ting JH, Erkelens JR, Morris MJ (2012) Leucine improves glucose and lipid status in offspring from obese dams, dependent on diet type, but not caloric intake. J Neuroendocrinol 24:1356–1364
Kelly AS, Rudser KD, Nathan BM et al (2013) The effect of glucagon-like peptide-1 receptor agonist therapy on body mass index in adolescents with severe obesity: a randomized, placebo-controlled, clinical trial. JAMA Pediatr 167:355–360
Rosenstock J, Klaff LJ, Schwartz S et al (2010) Effects of exenatide and lifestyle modification on body weight and glucose tolerance in obese subjects with and without pre-diabetes. Diabetes Care 33:1173–1175
Schlögl H, Kabisch S, Horstmann A et al (2013) Exenatide-induced reduction in energy intake is associated with increase in hypothalamic connectivity. Diabetes Care 36:1933–1940
Kulkarni RN, Mizrachi E-B, Ocana AG, Stewart AF (2012) Human β-cell proliferation and intracellular signaling: driving in the dark without a road map. Diabetes 61:2205–2213
Chen H, Simar D, Morris MJ (2009) Hypothalamic neuroendocrine circuitry is programmed by maternal obesity: interaction with postnatal nutritional environment. PLoS ONE 4:e6259
Chen H, Simar D, Lambert K, Mercier J, Morris MJ (2008) Intrauterine and postnatal overnutrition differentially impact appetite regulators and fuel metabolism. Endocrinology 149:5348–5356
Wren AM, Small CJ, Abbott CR et al (2001) Ghrelin causes hyperphagia and obesity in rats. Diabetes 50:2540–2547
Barnett AH (2012) The role of GLP-1 mimetics and basal insulin analogues in type 2 diabetes mellitus: guidance from studies of liraglutide. Diabetes Obes Metab 14:304–314
Knauf C, Cani PD, Ait-Belgnaoui A et al (2008) Brain glucagon-like peptide 1 signaling controls the onset of high-fat diet-induced insulin resistance and reduces energy expenditure. Endocrinology 149:4768–4777
Konturek PC, Konturek JW, Czesnikiewicz-Guzik M, Brzozowski T, Sito E, Konturek SJ (2005) Neuro-hormonal control of food intake: basic mechanisms and clinical implications. J Physiol Pharmacol 56(Suppl 6):5–25
Leibowitz SF, Alexander JT (1991) Analysis of neuropeptide Y-induced feeding: dissociation of Y1 and Y2 receptor effects on natural meal patterns. Peptides 12:1251–1260
Marty N, Dallaporta M, Thorens B (2007) Brain glucose sensing, counterregulation, and energy homeostasis. Physiology 22:241–251
Sandoval D, Cota D, Seeley RJ (2008) The integrative role of CNS fuel-sensing mechanisms in energy balance and glucose regulation. Annu Rev Physiol 70:513–535
Sandoval DA, Bagnol D, Woods SC, D’Alessio DA, Seeley RJ (2008) Arcuate glucagon-like peptide 1 receptors regulate glucose homeostasis but not food intake. Diabetes 57:2046–2054
Lam T, Gutierrez-Juarez R, Pocai A et al (2007) Brain glucose metabolism controls the hepatic secretion of triglyceride-rich lipoproteins. Nat Med 13:171–180
Kim J, Gall SL, Dewey HM, Macdonell RA, Sturm JW, Thrift AG (2012) Baseline smoking status and the long-term risk of death or nonfatal vascular event in people with stroke: a 10-year survival analysis. Stroke 43:3173–3178
Holst JJ, Vilsbøll T, Deacon CF (2009) The incretin system and its role in type 2 diabetes mellitus. Mol Cell Endocrinol 297:127–136
Eric AS, Juraj K, Michael PM, Iyad S, Dawn CS, Peter DR (2010) Exenatide suppresses postprandial elevations in lipids and lipoproteins in individuals with impaired glucose tolerance and recent onset type 2 diabetes mellitus. Atherosclerosis 212:217–222
Bojanowska E, Nowak A (2007) Interactions between leptin and exendin-4, a glucagon-like peptide-1 agonist, in the regulation of food intake in the rat. J Physiol Pharmacol 58:349–360
Astrup A, Rossner S, van Gaal L et al (2009) Effects of liraglutide in the treatment of obesity: a randomised, double-blind, placebo-controlled study. Lancet 374:1606–1616
Ranganath LR, Beety JM, Morgan LM, Wright JW, Howland R, Marks V (1996) Attenuated GLP-1 secretion in obesity: cause or consequence? Gut 38:916–919
Feinle C, Chapman IM, Wishart J, Horowitz M (2002) Plasma glucagon-like peptide-1 (GLP-1) responses to duodenal fat and glucose infusions in lean and obese men. Peptides 23:1491–1495
Hotamisligil GS, Shargill NS, Spiegelman BM (1993) Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 259:87–91
Nguyen MT, Favelyukis S, Nguyen AK et al (2007) A subpopulation of macrophages infiltrates hypertrophic adipose tissue and is activated by free fatty acids via Toll-like receptors 2 and 4 and JNK-dependent pathways. J Biol Chem 282:35279–35292
Weisberg SP, Hunter D, Huber R et al (2006) CCR2 modulates inflammatory and metabolic effects of high-fat feeding. J Clin Invest 116:115–124
Clement S, Juge-Aubry C, Sgroi A et al (2008) Monocyte chemoattractant protein-1 secreted by adipose tissue induces direct lipid accumulation in hepatocytes. Hepatology 48:799–807
Moran-Salvador E, Lopez-Parra M, Garcia-Alonso V et al (2011) Role for PPARgamma in obesity-induced hepatic steatosis as determined by hepatocyte- and macrophage-specific conditional knockouts. FASEB J 25:2538–2550
Pettinelli P, Videla LA (2011) Up-regulation of PPAR-γ mRNA expression in the liver of obese patients: an additional reinforcing lipogenic mechanism to SREBP-1c induction. J Clin Endocrinol Metab 96:1424–1430
Miquilena-Colina ME, Lima-Cabello E, Sánchez-Campos S et al (2011) Hepatic fatty acid translocase CD36 upregulation is associated with insulin resistance, hyperinsulinaemia and increased steatosis in non-alcoholic steatohepatitis and chronic hepatitis C. Gut 60:1394–1402
Chabowski A, Chatham JC, Tandon NN et al (2006) Fatty acid transport and FAT/CD36 are increased in red but not in white skeletal muscle of ZDF rats. Am J Physiol Endocrinol Metab 291:E675–E682
Langin D, Dicker A, Tavernier G et al (2005) Adipocyte lipases and defect of lipolysis in human obesity. Diabetes 54:3190–3197
Acknowledgements
We thank S. Rajia and V. Caruso (Pharmacology, School of Medical Sciences, University of New South Wales, Australia) for assistance with tissue harvesting at the endpoint.
Funding
This work presents independent research that was supported by Research Student Support from the Faculty of Science, University of Technology, Sydney to HC, and a research grant from Diabetes Australia Research Trust to HC, DS and MJM.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
HC, DS and MJM were involved in the project design, applying for funding and data interpretation. HC, KP and DS contributed to the animal experiments, data generation and interpretation, SS and CP contributed to data generation and interpretation. HC and KP wrote the first draft of the manuscript, and all authors read and modified the manuscript and approved the final draft.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 51 kb)
Rights and permissions
About this article
Cite this article
Chen, H., Simar, D., Pegg, K. et al. Exendin-4 is effective against metabolic disorders induced by intrauterine and postnatal overnutrition in rodents. Diabetologia 57, 614–622 (2014). https://doi.org/10.1007/s00125-013-3132-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-013-3132-5