Abstract
Aims/hypothesis
An increase in the production of reactive oxygen species is commonly thought to contribute to the development of diabetic cardiomyopathy. This study aimed to assess whether administration of the antioxidant coenzyme Q10 would protect the diabetic heart against dysfunction and remodelling, using the db/db mouse model of type 2 diabetes. Furthermore, we aimed to compare the efficacy of coenzyme Q10 to that of the ACE inhibitor ramipril.
Methods
Six-week-old non-diabetic db/+ mice and diabetic db/db mice received either normal drinking water or water supplemented with coenzyme Q10 for 10 weeks. Endpoint cardiac function was assessed by echocardiography and catheterisation. Ventricular tissue was collected for histology, gene expression and protein analysis.
Results
Untreated db/db diabetic mice exhibited hyperglycaemia, accompanied by diastolic dysfunction and adverse structural remodelling, including cardiomyocyte hypertrophy, myocardial fibrosis and increased apoptosis. Systemic lipid peroxidation and myocardial superoxide generation were also elevated in db/db mice. Coenzyme Q10 and ramipril treatment reduced superoxide generation, ameliorated diastolic dysfunction and reduced cardiomyocyte hypertrophy and fibrosis in db/db mice. Phosphorylation of Akt, although depressed in untreated db/db mice, was restored with coenzyme Q10 administration. We postulate that preservation of cardioprotective Akt signalling may be a mechanism by which coenzyme Q10-treated db/db mice are protected from pathological cardiac hypertrophy.
Conclusions/interpretation
These data demonstrate that coenzyme Q10 attenuates oxidative stress and left ventricular diastolic dysfunction and remodelling in the diabetic heart. Addition of coenzyme Q10 to the current therapy used in diabetic patients with diastolic dysfunction warrants further investigation.
Similar content being viewed by others
Introduction
The global incidence of diabetes mellitus has dramatically increased throughout the past two decades, firmly establishing the condition as one of the most significant health burdens of the 21st century. By the year 2025, 300 million individuals are projected to have diabetes, with the majority of these suffering from type 2 diabetes [1].
Coronary heart disease and peripheral vascular diseases are among the most common causes of mortality in diabetic individuals; however, a specific cardiomyopathy independent of these complications is also evident [2, 3]. Diabetic cardiomyopathy is typically characterised by left ventricular (LV) dysfunction, with diastolic dysfunction manifesting early in the disease [4]. Structural abnormalities such as LV hypertrophy and increased cardiac fibrosis occur together with the onset of diastolic dysfunction in the diabetic heart [5]. The presence of these characteristics acts as a predictive indicator of mortality in diabetic patients, necessitating the development of new pharmacological targets to treat LV dysfunction and remodelling in the diabetic heart.
Despite the importance of diabetic cardiomyopathy as a clinical entity, the molecular mechanisms potentiating the adverse changes in myocardial function and structure are poorly understood. The development and progression of diabetic complications is frequently attributed to an increase in the generation of reactive oxygen species (ROS), in particular superoxide, within susceptible tissues [6, 7]. The balance between the generation and elimination of ROS via antioxidant degradation is critical in maintaining cardiovascular health. As hyperglycaemia impairs the endogenous antioxidant defence system [8], numerous studies have examined the benefits of antioxidant supplementation in the setting of diabetes [9–11].
Coenzyme Q10, an endogenous component of the mitochondrial respiratory chain, functions as an antioxidant in its reduced form, ubiquinol-10. Coenzyme Q10 has previously been shown to inhibit cardiac oxidative stress [12, 13]. A protective role for coenzyme Q10 has been suggested in settings of heart failure outside diabetes [14–16]. However, the potential of coenzyme Q10 to attenuate the structural and functional defects specifically caused by diabetic cardiomyopathy still remains to be elucidated.
The aim of the present study was to assess the efficacy of the antioxidant coenzyme Q10 in protecting the diabetic heart against adverse changes using the db/db mouse model of type 2 diabetes. We hypothesised that the administration of coenzyme Q10 would protect against the impaired LV function and adverse structural changes induced by type 2 diabetes. As ACE inhibitors (ACE-Is) are the current gold standard in minimising cardiovascular risk and hypertension in clinical settings, we also aimed to evaluate the efficacy of coenzyme Q10 compared with the ACE-I ramipril in treating diabetic cardiomyopathy.
Methods
Animal model
All animal research was conducted in accordance with the National Health and Medical Research Council of Australia guidelines, and was approved by the Alfred Medical Research and Education Precinct (AMREP) Animal Ethics committee.
Female C57BL/6 db/+ and db/db mice were obtained from Jackson Laboratories (Bar Harbor, ME, USA). The mice were housed in the AMREP Precinct Animal Centre and maintained under a 12 h light–dark cycle. Age-matched female non-diabetic db/+ mice and diabetic db/db mice received a standard diet and normal drinking water. At 6 weeks of age, the db/+ and db/db mice were allocated either to continue receiving regular water, to receive water supplemented with coenzyme Q10 (10 mg/kg; LiQsorb Liposomal CoQ10, a kind gift from R. K. Chopra, Tishcon Corp, NY, USA, using a dose previously shown to limit the renal complications of diabetes [17]) or to receive water supplemented with ramipril (3 mg kg−1 day−1; Sigma Aldrich, St Louis, MO, USA). The mice were followed for a further 10 weeks prior to killing and tissue collection. Blood was collected at the endpoint for assessment of plasma glucose (Austin Pathology Service, Heidelberg, VIC, Australia). Animals with plasma glucose levels exceeding 28 mmol/l were considered diabetic. Blood was also retained for measurement of HbA1c by HPLC (CLC330 GHb Analyser; Primus, Kansas City, MO, USA) [18].
Analysis of LV function in vivo
Endpoint LV function and chamber dimensions were assessed via two-dimensional targeted M-mode echocardiography and Doppler echocardiography. At 16 weeks of age, mice were anaesthetised with a cocktail of ketamine, xylazine and atropine (100, 10 and 1.2 mg/kg i.p.), and echocardiography was performed using a Philips (North Ryde, NSW, Australia) iE33 ultrasound machine with a 15 MHz linear array transducer.
Variables measured on M-mode echocardiography included LV end-systolic dimension (LVESD), LV end-diastolic dimension (LVEDD), LV mass (calculated as [external LV dimension3 − LVEDD] × 1.055) and fractional shortening (FS, calculated as [(LVEDD − LVESD)/LVEDD] × 100%). Doppler echocardiography allowed assessment of LV diastolic filling (LV E:A − the ratio of peak early, E, and late, A, transmitral blood flow velocities) and deceleration time of early (E) velocity [19].
LV pressure was also measured by cardiac catheterisation. A micromanometer-tipped catheter (1.4 F; Millar Instrument Co., TX, USA) was inserted through the right common carotid artery into the LV and the aorta of an anaesthetised mouse (ketamine 100 mg/kg, xylazine 10 mg/kg, atropine 1.2 mg/kg i.p.) as previously described [19]. Variables derived from catheterisation included systolic blood pressure (SBP) and LV end-diastolic pressure (LVEDP).
Tissue collection and histology
Following catheterisation, with the animal still anaesthetised, cardiac puncture was performed to collect approximately 1 ml of blood in a heparinised syringe. The heart and lungs were then excised from the animals and their wet weights recorded. The tibia was removed and used to calculate the ratio of heart weight to tibial length (HW:TL). A portion of the ventricle was cut, fixed and embedded in paraffin for histology. Paraffin-embedded sections were cut and stained with haematoxylin and eosin (H&E) or 0.1% Picrosirius Red and analysed as previously described [19]. The remaining portion of the ventricle was snap-frozen and stored at −80°C.
Levels of apoptosis were assessed in paraffin-embedded ventricular sections using the CardioTACS In Situ Apoptosis Detection Kit (Trevigen, Gaithersburg, MD, USA) [20]. This method detects nuclear DNA fragmentation by using a terminal deoxynucleotidyl transferase enzyme, which incorporates labelled nucleotides onto the free 3′ OH ends of DNA fragments. Positively stained apoptotic cells were distinguished by blue staining, while negatively stained cells were counterstained red with Nuclear Fast Red. Apoptotic cells were quantified as a percentage of non-apoptotic cells, and the results were expressed as fold levels detected in untreated db/+ mouse heart.
Gene expression and protein analysis
RNA and protein were extracted from frozen tissue samples as previously described [10]. cDNA was produced from DNase-treated RNA via reverse transcription (Taqman Reverse Transcription reagents; Applied Biosystems, Mulgrave, VIC, Australia) at template concentrations of 20 ng/μl, as previously published [10, 19, 21]. SYBR Green chemistry (Applied Biosystems) was employed to determine expression of both β-myosin heavy chain (Myh7) and sarco/endoplasmic reticulum Ca2+-ATPase (SERCA2a, also known as Atp2a2), using the Applied Biosystems ABI Prism 7700 Sequence Detection System. Ribosomal 18S (also known as Rn18s) was used as the endogenous control. All primers were generated using murine-specific sequences derived from Genebank, at predetermined concentrations. The relative fold increases in the expression of the gene of interest compared with untreated non-diabetic mice were calculated using the comparative delta-delta Ct (∆∆Ct) method [10, 22].
Analysis of protein levels
SDS-PAGE and western blotting were employed to measure the protein levels of phosphorylated Akt (Ser473) and total Akt. Both antibodies were purchased from Cell Signaling Technologies (Danvers, MA, USA), and used at a 1:1,000 dilution, according to manufacturer’s instructions. Akt protein bands were detected at 60 kDa, and results were analysed using the Image J 1.4 software (NIH, Bethesda, MD, USA) [19].
Detection of lipid peroxidation and superoxide generation
The levels of lipid peroxidation in plasma samples were determined using the Malondialdehyde-586 kit (Bioxytech MDA-586, Foster City, CA, USA), as per the manufacturer’s instructions. Superoxide generation was quantified using lucigenin (5 μmol/l)-enhanced chemiluminescence in fresh heart tissue, as previously described [10]. Results were normalised against tissue weight, and expressed as relative light units per second per milligram.
Statistical analysis
All data are presented as mean±SE (unless otherwise specified). Two-way ANOVAs were performed to identify differences between genotypes (db/+ and db/db) and treatments (untreated, coenzyme Q10-treated, ramipril-treated). Interactions between groups were statistically analysed using the Student’s Newman–Keuls post hoc test. A value of p < 0.05 was considered significant.
Results
Hyperglycaemia is evident in db/db mice
Untreated, coenzyme Q10-treated and ramipril-treated db/db mice all exhibited marked hyperglycaemia compared with relative db/+ controls in terms of both plasma glucose and HbA1c (Table 1). HbA1c levels were modestly but significantly reduced in coenzyme Q10-treated db/db mice vs untreated db/db mice. Body weight was greater in db/db diabetic animals compared with db/+ animals; neither coenzyme Q10 nor ramipril treatment noticeably affected body weight in either db/+ or db/db mice compared with untreated littermates (Table 1). Lung weight was no different between db/+ and db/db animals (Table 1) and was unaffected by treatment. HW data are discussed below.
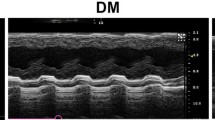
Coenzyme Q10 preserves diastolic function
Analysis of endpoint cardiac function via M-mode echocardiography revealed no differences in FS (a marker of systolic function) between db/+ and db/db mice, across all treatment groups (Table 2). On Doppler echocardiography, a prolonged deceleration time (indicative of impaired diastolic function) was observed in untreated db/db mice compared with db/+ mice (Fig. 1a). Both coenzyme Q10- and ramipril-treated db/db mice exhibited reduced deceleration times compared with untreated db/db mice (Fig. 1a). A similar trend for E:A ratio to decrease was seen in untreated db/db mice vs db/+ mice (p = 0.065; Table 2). Endpoint cardiac catheterisation further confirmed the presence of diastolic dysfunction in untreated db/db mice, where LVEDP was significantly higher that in untreated db/+ mice (Fig. 1b). Coenzyme Q10 and ramipril significantly attenuated this increase in LVEDP in db/db mice. On real-time PCR, Serca2a expression was depressed in untreated diabetic mice, but preserved with coenzyme Q10 and ramipril treatment (Fig. 1c).
Coenzyme Q10 preserves diastolic function and Serca2a expression. In diabetic mice, coenzyme Q10 and ramipril (a) decreased deceleration time, (b) reduced LVEDP and (c) prevented the diabetes-induced fall in the gene expression of Serca2a. n = 8–12/group. White bars, db/+; black bars, db/db. *p < 0.05 vs db/+ untreated, ***p < 0.001 vs db/+ untreated, † p < 0.05 vs db/+ coenzyme Q10, ‡ p < 0.05 vs db/+ ramipril, § p < 0.05 vs db/db untreated
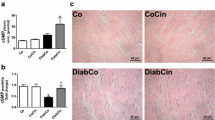
Cardiac fibrosis is reduced in coenzyme Q10-treated diabetic mice
On Sirius Red-stained sections, diabetes induced a 1.8-fold increase in collagen deposition in untreated db/db mice relative to non-diabetic db/+ mice (Fig. 2). Comparatively, no differences in collagen deposition were observed between the db/db and db/+ genotypes, in both coenzyme Q10- and ramipril-treated animals (Fig. 2). Diabetes-induced increases in collagen deposition were completely ameliorated by coenzyme Q10 and ramipril treatment.
Cardiac fibrosis is reduced in coenzyme Q10-treated mice. a Representative Sirius Red-stained LV sections. Collagen appears red; magnification × 200; scale bar 40 μm. b Pooled data on quantification of collagen area per visual field. n = 7–12/group. ***p < 0.001 vs db/+ untreated, § p < 0.05 vs db/db untreated. White bars, db/+; black bars, db/db
Coenzyme Q10 limits diabetes-induced cardiomyocyte hypertrophy
Untreated db/db mice had significantly greater HW than db/+ controls, when normalised to TL (Table 1). Despite HW:TL being greater in ramipril-treated db/db mice than db/+ controls, ramipril-treated db/db mice had comparatively smaller hearts than untreated db/db mice; a similar trend was evident in coenzyme Q10-treated db/db mice, but this was not significant (p = 0.1). On M-mode echocardiography, LV mass normalised to TL was reduced in both coenzyme Q10-treated and ramipril-treated db/db mice compared with untreated db/db controls (Table 2).
Untreated db/db mice exhibited significantly hypertrophied cardiomyocytes on H&E-stained sections (Fig. 3a and b), accompanied by elevated gene expression of the hypertrophic marker Myh7 (Fig. 3c) compared with untreated db/+ mice. Although coenzyme Q10-treated db/db mice also displayed increased cardiomyocyte size and Myh7expression compared with db/+ mice, these parameters were significantly lower than in untreated db/db mice. Ramipril-treated db/db mice were similarly protected from diabetes-induced increases in cardiomyocyte width and Myh7expression.
Coenzyme Q10 limits diabetes-induced cardiomyocyte hypertrophy. a Representative sections of the H&E stained LV sections; magnification × 400; scale bar 20 μm. The arrow indicates a representative cardiomyocyte width measurement. b Pooled data on cardiomyocyte width (n = 10–11/group). c Gene expression of hypertrophic marker Myh7/ analysed using real-time PCR and normalised against 18S expression. n = 5–10/group. d Quantitative analysis of Akt phosphorylation (phospho-Akt) normalised to total Akt with representative western blot analysis in untreated, Coenzyme Q10- and ramipril-treated hearts. Mean values for db/+ untreated were normalised to 1. n = 6–8/group. *p < 0.05 vs db/+ untreated, ***p < 0.001 vs db/+ untreated, † p < 0.05 vs db/+ Coenzyme Q10, ‡ p < 0.05 vs db/+ ramipril, § p < 0.05 vs db/db untreated. ¶ p = 0.05. White bars, db/+; black bars, db/db. CoQ, Coenzyme Q10
The cell survival kinase Akt, a downstream target of the IGF1 receptor–phosphoinositide-3 kinase p110α isoform (IGF1R-PI3K[p110α]) pathway, is an important mediator of physiological heart growth [23]. In the present study, Akt phosphorylation showed a strong trend to decrease in untreated diabetic mice vs. untreated control mice (p = 0.05; Fig. 3d). Both coenzyme Q10 and ramipril restored Akt phosphorylation back to levels observed in the non-diabetic mice (Fig. 3d).
Coenzyme Q10 treatment prevents diabetes-induced cardiomyocyte death
Diabetes induced a 3.9 ± 0.4-fold increase in the proportion of apoptotic cells in untreated db/db mice compared with db/+ mice (Fig. 4). Both coenzyme Q10- and ramipril-treated db/db mice also exhibited a greater number of apoptotic cells compared with their non-diabetic controls. Apoptosis was significantly reduced in both coenzyme Q10-treated db/db mice (1.8 ± 0.2-fold that detected in untreated db/+mice) and ramipril-treated db/db mice (2.3 ± 0.5-fold untreated db/+ mice).
Coenzyme Q10 prevents diabetes-induced cardiomyocyte apoptosis. a Representative LV sections stained using the CardioTACS In Situ Apoptosis Detection Kit. Positively stained apoptotic cells appear dark blue (indicated by arrows); magnification × 200; scale bar 20 μm. b Quantification of positively stained apoptotic cells/negatively stained non-apoptotic cells, expressed as fold levels detected in untreated db/+mouse heart n = 3/group. *p < 0.05 vs db/+ untreated, † p < 0.05 vs db/+ coenzyme Q10, § p < 0.05 vs db/db untreated. White bars, db/+; black bars, db/db. AU, arbitrary units
Coenzyme Q10 attenuates oxidative stress in db/db mice
Plasma concentrations of MDA, a marker of systemic lipid peroxidation, were significantly upregulated in both untreated and ramipril-treated db/db mice compared with db/+ controls (Fig. 5a). Importantly, MDA concentrations in coenzyme Q10-treated db/db mice were markedly reduced compared with their untreated counterparts, such that they were no different from the values in coenzyme Q10-treated db/+ mice. On lucigenin chemiluminescence, untreated db/db mice exhibited greater superoxide generation in the myocardium compared with db/+ controls (Fig. 5b). Coenzyme Q10 showed a strong tendency to reduce superoxide generation (p = 0.05), whereas ramipril significantly lowered superoxide production in diabetic animals.
Coenzyme Q10 reduces oxidative stress in db/db mice. a Coenzyme Q10, but not ramipril, significantly reduced plasma concentrations of MDA, a marker of lipid peroxidation (n = 6–8/group). b Ramipril markedly reduced the cardiac generation of superoxide; similar trends were observed with coenzyme Q10 treatment (n = 8–14/group). ***p < 0.001 vs db/+ untreated, ‡ p < 0.05 vs db/+ ramipril, § p < 0.05 vs db/db untreated. ¶ p = 0.05. White bars, db/+; black bars, db/db. RLU, relative light unit
Coenzyme Q10 reduces SBP
Diabetic db/db mice exhibited a significantly higher SBP than non-diabetic db/+ mice, regardless of treatment group (Fig. 6). Both coenzyme Q10 and ramipril treatment resulted in a modest reduction of SBP (<10 mmHg), which remained significantly elevated compared with untreated diabetic mice. Neither coenzyme Q10 nor ramipril treatment affected diastolic blood pressure (DBP) in the db/db mice, or either SBP or DBP in non-diabetic mice (results not shown).
SBP is decreased in coenzyme Q10-treated diabetic mice. Both coenzyme Q10 and ramipril treatment marginally reduced SBP in hypertensive diabetic animals. n = 7–11/group. ***p < 0.001 vs db/+ untreated, † p < 0.05 vs db/+ coenzyme Q10, ‡ p < 0.05 vs db/+ ramipril, § p < 0.05 vs db/db untreated. White bars, db/+; black bars, db/db
Discussion
The pathophysiology of diabetic cardiomyopathy is multifactorial; cardiomyocyte hypertrophy, interstitial fibrosis and cardiomyocyte death further exacerbate diastolic dysfunction [24]. Hyperglycaemia-induced ROS generation has been implicated as a key stimulator of these cardiac impairments [25, 26]. Consequently, reducing oxidative stress, in particular excess cardiac superoxide generation, should be favourable in the management of diabetic cardiomyopathy. The major finding of the current study is that the antioxidant coenzyme Q10 protected the heart in the db/db mouse model of type 2 diabetes from the development of adverse structural and functional changes, with efficacy comparable to the ACE-I ramipril.
LV diastolic dysfunction is often the earliest hallmark of diabetic cardiomyopathy, preceding the onset of systolic dysfunction [4]. In the current study, diabetes-induced diastolic dysfunction was evident on Doppler echocardiography as prolonged deceleration time, with a similar trend for E:A, indicative of impaired LV relaxation. Diabetes also significantly elevated LVEDP. Importantly, treatment with either coenzyme Q10 or ramipril significantly reduced diastolic dysfunction in terms of all three variables. Previously, Chew and colleagues failed to observe significant effects of coenzyme Q10 on LV diastolic dysfunction in diabetic patients, although a trend towards improved E:A was evident [27]. Importantly, differences in patient characteristics at baseline as well as concomitant medication (ACE-1, statins, angiotensin receptor blockers) were likely to have masked coenzyme Q10 cardioprotection [27]. The absence of systolic dysfunction in db/db mice is consistent with previous reports in both experimental and clinical settings [19, 28] in which systolic dysfunction manifested later in the disease.
In the present study, cardiac collagen deposition was significantly increased in untreated diabetic mice, consistent with previous findings [29]. Diastolic dysfunction may thus be a secondary consequence of this increased myocardial stiffness. Coenzyme Q10 and ramipril treatment significantly prevented this upregulation of collagen deposition. We also present evidence that type 2 diabetes-induced downregulation of SERCA2a, a key modulator of cardiomyocyte contractile function, is significantly ameliorated by coenzyme Q10, suggesting a further role for coenzyme Q10 in protecting the heart against contractile dysfunction, possibly through improved cardiac bioenergetics [30, 31].
Pathological LV hypertrophy is a common structural hallmark of the diabetic heart, and is a strong predictor of myocardial infarction, heart failure and stroke [32]. Our findings show that HW:TL, cardiomyocyte width and Myh7 expression, all markers of hypertrophy, were upregulated in the hearts of untreated db/db mice. Although coenzyme Q10 did not significantly reduce HW:TL in db/db diabetic mice, it significantly reduced LV mass (on echocardiography), cardiomyocyte width and Myh7 expression compared with untreated diabetic mice. Ramipril elicited comparable reductions in LV mass, cardiomyocyte width and Myh7 expression, as well as decreasing HW:TL.
Coenzyme Q10 treatment has also been shown to elicit beneficial antihypertrophic effects in the setting of hypertrophic cardiomyopathy [33]. The net increase in HW:TL in diabetic mice occurred in the face of increased LV apoptosis, consistent with previous studies [9, 34]. Both hyperglycaemia and oxidative stress can induce apoptosis, further impairing myocardial structure and function, which is implicated in the transition from compensated to decompensated hypertrophy in the diabetic heart [34, 35]. The ability of coenzyme Q10 to reduce diabetes-induced cell death may underlie its effectiveness in reducing myocardial dysfunction and structural remodelling.
Elevated oxidative stress plays a prominent role in the progression of diabetic cardiac complications [8]. Coenzyme Q10 levels are reduced in patients with heart disease and/or diabetes [36], perhaps due to fewer functional mitochondria. In the present study, replenishment of coenzyme Q10 reduced both systemic lipid peroxidation and ventricular superoxide production, in accordance with its ability to reduce oxidative stress and scavenge free radicals in its reduced state [37]. However, it still remains to be determined whether exogenously administered coenzyme Q10 is taken up by mitochondria and reincorporated into the electron transport chain, in addition to increasing circulating coenzyme Q10 [27, 38].
Coenzyme Q10 is detected in membranes other than mitochondria, suggesting that its antioxidant actions are widespread and of physiological importance [30]. Interestingly in the current study, ramipril failed to reduce systemic lipid peroxidation, but it effectively lowered cardiac superoxide production, as previously described [39, 40]. The reduced generation of ROS (and hence restored redox balance) achieved by coenzyme Q10 and ramipril treatment in the present study is likely to be a key mechanism by which they limited myocardial fibrosis and cardiomyocyte hypertrophy in this model of type 2 diabetes, as has been implicated in other settings of cardiac fibrosis [25, 41] and LV hypertrophy [22, 42, 43].
The downstream molecular signalling pathways implicated in ROS-induced cardiac remodelling have not been fully resolved. We demonstrated that cardiac Akt phosphorylation, a downstream target of IGF1R-PI3K(p110α), was reduced in type 2 diabetes, but was restored with coenzyme Q10 and ramipril treatment. The IGF1R-PI3K(p110α)-Akt pathway induces a physiological hypertrophic response associated with cardioprotection [19, 23, 44], in which cardiac structure and function are preserved. Based on our observations, we postulate that increased ROS depresses protective IGF1R-PI3K(p110α)-Akt signalling. The preservation of Akt activity in the coenzyme Q10-treated diabetic myocardium may thereby confer protection against pathological cardiac hypertrophy. This relationship between LV ROS generation and IGF1R-PI3K(p110α)-Akt signalling warrants further investigation.
Hypertension is a frequent cardiovascular complication in the diabetic population, which further limits patient prognosis [45]. In the current study, SBP was significantly elevated in diabetic mice (in line with previous studies [46]), which was evident in all treatment groups. Although this was modestly reduced by both coenzyme Q10 and ramipril, this reduction was not strongly correlated with cardiomyocyte width reduction; i.e. the effect of coenzyme Q10 and ramipril on reducing cardiomyocyte size was much greater than would be expected based on the modest lowering of SBP. The benefits of coenzyme Q10 on diabetic cardiomyopathy are thus likely to be largely independent of reduced afterload. The mechanism underlying the antihypertensive effect of coenzyme Q10 is inadequately understood, but a reduction in peripheral vascular resistance has been suggested [38, 47, 48]. The antihypertensive actions of ramipril are well known [39, 49].
Limitations of the study
Despite the extensive use of db/db mice in the study of various diabetes-related pathologies, the db/db mouse model is not a perfect model of the human disease. A defect in the leptin receptor subjects db/db mice to severe lipotoxicity, more excessive than is observed in diabetes in humans. However, db/db mice display a cardiac pathological phenotype that closely mirrors human diabetic cardiomyopathy, including increased cardiac size, depressed cardiac function and efficiency, and impaired Ca2+ handling [50]. Despite its limitations, the db/db mouse model is considered one of the better animal models for studying the mechanisms underlying human diabetic heart disease and the identification of potential cardiomyopathy-reducing therapeutic agents [50].
Another limitation of our study was the route of coenzyme Q10 administration. The dosage of coenzyme Q10 in drinking water was designed in accordance with average daily water intake of db/+ and db/db mice, and small differences in total dose between animals probably occurred. We acknowledge that oral gavage is a more accurate rate of drug delivery, but this is not well-tolerated by db/+ or db/db mice.
Conclusions
In summary, this study demonstrates the benefit of treating diabetic cardiomyopathy with exogenous antioxidants. Coenzyme Q10 attenuated diabetes-induced diastolic dysfunction, cardiomyocyte hypertrophy, cardiac fibrosis and cell death. The cardioprotective effect of coenzyme Q10 may be mediated through its ability to inhibit systemic oxidative stress, improve cardiac bioenergetics and preserve Akt and SERCA2a regulation in the diabetic context. To our knowledge, our study is the first to establish the ability of coenzyme Q10 to prevent diabetic cardiomyopathy, and to compare the efficacy of coenzyme Q10 with that of an ACE-I. Considering that ROS-mediated cardiac complications are a major contributor to morbidity and death in the diabetic population, coenzyme Q10 may be a clinically valuable adjunct therapy to standard care for preserving cardiac function in diabetic patients.
Abbreviations
- ACE-I:
-
ACE inhibitor
- AMREP:
-
Alfred medical research and education precinct
- DBP:
-
Diastolic blood pressure
- E:A:
-
Ratio of peak early to late transmitral blood flow velocities
- FS:
-
Fractional shortening
- H&E:
-
Haematoxylin and eosin
- HW:
-
Heart weight
- IGF1R:
-
IGF1 receptor
- LV:
-
Left ventricular
- LVEDD:
-
LV end-diastolic dimension
- LVEDP:
-
LV end-diastolic pressure
- LVESD:
-
LV end-systolic dimension
- MDA:
-
Malondialdehyde
- PI3K[p110α]:
-
Phosphoinositide-3 kinase p110α isoform
- ROS:
-
Reactive oxygen species
- SBP:
-
Systolic blood pressure
- SERCA2a:
-
Sarco/endoplasmic reticulum Ca2+-ATPase
- TL:
-
Tibial length
References
Shaw JE, Sicree RA, Zimmet PZ (2010) Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 87(1):4–14
Fang ZY, Prins JB, Marwick TH (2004) Diabetic cardiomyopathy: evidence, mechanisms, and therapeutic implications. Endocr Rev 25:543–567
Rubler S, Yuceoglu YZ, Kumral T, Grishman A, Branwood AW, Dlugash J (1972) New type of cardiomyopathy associated with diabetic glomerulosclerosis. Am J Cardiol 30:595–602
Schannwell CM, Schneppenheim M, Perings S, Plehn G, Strauer BE (2002) Left ventricular diastolic dysfunction as an early manifestation of diabetic cardiomyopathy. Cardiology 98:33–39
Asbun J, Villarreal FJ (2006) The pathogenesis of myocardial fibrosis in the setting of diabetic cardiomyopathy. J Am Coll Cardiol 47:693–700
Evans JL, Goldfine ID, Maddux BA, Grodsky GM (2002) Oxidative stress and stress-activated signaling pathways: a unifying hypothesis of type 2 diabetes. Endocr Rev 23:599–622
Haidara MA, Yaseen HZ, Rateb M, Ammar H, Zorkani MA (2006) Role of oxidative stress in development of cardiovascular complications in diabetes mellitus. Curr Vasc Pharmacol 4:215–227
Maritim AC, Sanders RA, Watkins JB (2003) Diabetes, oxidative stress, and antioxidants: a review. J Biochem Mol Toxicol 17:24–38
Fiordaliso F, Bianchi R, Staszewsky L et al (2004) Antioxidant treatment attenuates hyperglycemia-induced cardiomyocyte death in rats. J Mol Cell Cardiol 37:959–968
Ritchie RH, Quinn JM, Cao AH et al (2007) The antioxidant tempol inhibits cardiac hypertrophy in the insulin-resistant GLUT4-deficient mouse in vivo. J Mol Cell Cardiol 42:1119–1128
Cai L (2006) Suppression of nitrative damage by metallothionein in diabetic heart contributes to the prevention of cardiomyopathy. Free Radic Biol Med 41:851–861
Rauscher FM, Sanders RA, Watkins JB (2001) Effects of coenzyme Q10 treatment on antioxidant pathways in normal and streptozotocin-induced diabetic rats. J Biochem Mol Toxicol 15:41–46
Coldiron AD, Sanders RA, Watkins JB (2002) Effects of combined quercetin and coenzyme Q(10) treatment on oxidative stress in normal and diabetic rats. J Biochem Mol Toxicol 16:197–202
Langsjoen PH, Langsjoen A, Willis R, Folkers K (1997) Treatment of hypertrophic cardiomyopathy with coenzyme Q(10). Mol Asp Med 18:S145–S151
Silver MA, Langsjoen PH, Szabo S, Patil H, Zelinger A (2004) Effect of atorvastatin on left ventricular, diastolic function and ability of coenzyme Q(10) to reverse that dysfunction. Am J Cardiol 94:1306–1310
Sander S, Coleman CI, Patel AA, Kluger J, White CM (2006) The impact of coenzyme Q10 on systolic function in patients with chronic heart failure. J Card Fail 12:464–472
Sourris KC, Harcourt BE, Tang PH et al (2012) Ubiquinone (coenzyme Q10) prevents renal mitochondrial dysfunction in an experimental model of type 2 diabetes. Free Radic Biol Med 52:716–723
Dunn SR, Qi ZH, Bottinger EP, Breyer MD, Sharma K (2004) Utility of endogenous creatinine clearance as a measure of renal function in mice. Kidney Int 65:1959–1967
Huynh K, McMullen JR, Julius T et al (2010) Cardiac-specific insulin-like growth factor 1 receptor transgenic expression protects against cardiac fibrosis and diastolic dysfunction in a mouse model of diabetic cardiomyopathy. Diabetes 59:1512–1520
Chen ZY, Chua CC, Ho YS, Hamdy RC, Chua BHL (2001) Overexpression of Bcl-2 attenuates apoptosis and protects against myocardial I/R injury in transgenic mice. Am J Physiol-Heart Circul Physiol 280:H2313–H2320
Rosenkranz AC, Hood SG, Woods RL, Dusting GJ, Ritchie RH (2003) B-type natriuretic peptide prevents acute hypertrophic responses in the diabetic rat heart—importance of cyclic GMP. Diabetes 52:2389–2395
Laskowski A, Woodman OL, Cao AH et al (2006) Antioxidant actions contribute to the antihypertrophic effects of atrial natriuretic peptide in neonatal rat cardiomyocytes. Cardiovasc Res 72:112–123
McMullen JR, Shioi T, Zhang L et al (2003) Phosphoinositide 3-kinase(p110 alpha) plays a critical role for the induction of physiological, but not pathological, cardiac hypertrophy. Proc Natl Acad Sci USA 100:12355–12360
Devereux RB, Roman MJ, Paranicas M et al (2000) Impact of diabetes on cardiac structure and function. The strong heart study. Circulation 101:2271–2276
Gonzalez-Vilchez F, Ayuela J, Ares M, Pi J, Castillo L, Martin-Duran R (2005) Oxidative stress and fibrosis in incipient myocardial dysfunction in type 2 diabetic patients. Int J Cardiol 101:53–58
Bonnefont-Rousselot D, Bastard JP, Jaudon MC, Delattre J (2000) Consequences of the diabetic status on the oxidant/antioxidant balance. Diabetes Metab 26:163–176
Chew GT, Watts GF, Davis TME et al (2008) Hemodynamic effects of fenofibrate and coenzyme Q(10) in type 2 diabetic subjects with left ventricular diastolic dysfunction. Diabetes Care 31:1502–1509
Diamant M, Lamb HJ, Groeneveld Y et al (2003) Diastolic dysfunction is associated with altered myocardial metabolism in asymptomatic normotensive patients with well-controlled type 2 diabetes mellitus. J Am Coll Cardiol 42:328–335
Shimizu M, Umeda K, Sugihara N et al (1993) Collagen remodelling in myocardia of patients with diabetes. J Clin Path 46:32–36
Kumar A, Kaur H, Devi P, Mohan V (2009) Role of coenzyme Q10 (CoQ10) in cardiac disease, hypertension and Meniere-like syndrome. Pharmacol Ther 124:259–268
Belke DD, Swanson EA, Dillmann WH (2004) Decreased sarcoplasmic reticulum activity and contractility in diabetic db/db mouse heart. Diabetes 53:3201–3208
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP (1990) Prognostic implications of echocardiographically determined left-ventricular mass in the Framingham Heart Study. New Engl J Med 322:1561–1566
Langsjoen PH, Langsjoen A, Willis R, Folkers K (1996) Treatment of hypertrophic cardiomyopathy with coenzyme Q(10). Pergamon, Ancona, Italy, pp S145–S151
Frustaci A, Kajstura J, Chimenti C et al (2000) Myocardial cell death in human diabetes. Circ Res 87:1123–1132
Fiordaliso F, Li BS, Latini R et al (2000) Myocyte death in streptozotocin-induced diabetes in rats is angiotensin II-dependent. Lab Invest 80:513–527
Lim SC, Tan HH, Goh SK et al (2006) Oxidative burden in prediabetic and diabetic individuals: evidence from plasma coenzyme Q(10). Diabet Med 23:1344–1349
Bentinger M, Brismar K, Dallner G (2007) The antioxidant role of coenzyme Q. Mitochondrion 7:S41–S50
Hodgson JM, Watts GF, Playford DA, Burke V, Croft KD (2002) Coenzyme Q(10) improves blood pressure and glycaemic control: a controlled trial in subjects with type 2 diabetes. Eur J Clin Nutr 56:1137–1142
Liang W, Tan CYR, Ang L et al (2008) Ramipril improves oxidative stress-related vascular endothelial dysfunction in db/db mice. J Physiol Sci 58:405–411
Otto A, Fontaine J, Berkenboom G (2006) Ramipril treatment protects against nitrate-induced oxidative stress in eNOS(−/−) mice: an implication of the NADPH oxidase pathway. J Cardiovasc Pharmacol 48:842–849
Aragno M, Mastrocola R, Alloatti G et al (2008) Oxidative stress triggers cardiac fibrosis in the heart of diabetic rats. Endocrinology 149:380–388
Bendall JK, Cave AC, Heymes C, Gall N, Shah AM (2002) Pivotal role of a gp91(phox)-containing NADPH oxidase in angiotensin II-induced cardiac hypertrophy in mice. Circulation 105:293–296
Nakagami H, Takemoto M, Liao JK (2003) NADPH oxidase-derived superoxide anion mediates angiotensin II-induced cardiac hypertrophy. J Mol Cell Cardiol 35:851–859
McMullen JR, Shioi T, Huang WY et al (2004) The insulin-like growth factor 1 receptor induces physiological heart growth via the phosphoinositide 3-kinase(p110 alpha) pathway. J Biol Chem 279:4782–4793
Stas SN, El-Atat FA, Sowers JR (2004) Pathogenesis of hypertension in diabetes. Rev Endocr Metab Disord 5:221–225
Su W, Guo ZH, Randall DC, Cassis L, Brown DR, Gong MC (2008) Hypertension and disrupted blood pressure circadian rhythm in type 2 diabetic db/db mice. Am J Physiol-Heart Circ Physiol 295:H1634–H1641
Singh RB, Niaz MA, Rastogi SS, Shukla PK, Thakur AS (1999) Effect of hydrosoluble coenzyme Q10 on blood pressures and insulin resistance in hypertensive patients with coronary artery disease. J Hum Hypertens 13:203–208
Rosenfeldt FL, Haas SJ, Krum H et al (2007) Coenzyme Q(10) in the treatment of hypertension: a meta-analysis of the clinical trials. J Hum Hypertens 21:297–306
Luders S, Schrader J, Berger J et al (2008) The PHARAO study: prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure—a prospective, randomised, controlled prevention trial of the German Hypertension League. J Hypertens 26:1487–1496
Bugger H, Abel ED (2009) Rodent models of diabetic cardiomyopathy. Dis Model Mech 2:454–466
Acknowledgements
The authors thank N. Jennings for her help with echocardiography, K. Gilbert for her help with animal monitoring and M. A. Arnstein for helpful advice on histological analysis (all from the Baker IDI Heart and Diabetes Institute). Parts of this study were presented in abstract form at the 2010 Scientific Sessions of the American Heart Association, Chicago, IL, USA, November 2010.
Funding
This work was supported by the Diabetes Australia Research Trust and the National Health and Medical Research Council of Australia (NHMRC project ID526638 to RHR, JRM and KAJ-D), and supported in part by the Victorian Government’s Operational Infrastructure Support Program. KH is supported by an Australian Postgraduate Award. JRM is supported by an Australian Research Council Future Fellowship (FT0001657) and holds an Honorary NHMRC Research Fellowship (586604). X-JD holds an NHMRC Senior Research Fellowship (ID317808). RHR is the recipient of an NHMRC Senior Research Fellowship (ID472673).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
KH, JRM and RHR contributed to the design of the study, data acquisition, analysis and interpretation of data and drafting of the manuscript. HK, JMF and JEL contributed to data acquisition and interpretation, and manuscript revision. XJD and KJD contributed to data interpretation and manuscript revision. All authors have approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. R. McMullen and R. H. Ritchie are joint senior authors of this study.
Rights and permissions
About this article
Cite this article
Huynh, K., Kiriazis, H., Du, XJ. et al. Coenzyme Q10 attenuates diastolic dysfunction, cardiomyocyte hypertrophy and cardiac fibrosis in the db/db mouse model of type 2 diabetes. Diabetologia 55, 1544–1553 (2012). https://doi.org/10.1007/s00125-012-2495-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2495-3