Abstract
Aims/hypothesis
Despite advances in pharmacological treatments, diabetes with hypertension continues to be a major public health problem with high morbidity and mortality rates. We recently identified a circulating peptide coupling factor 6 (CF6), which binds to the plasma membrane ATP synthase (ecto-F1Fo complex), resulting in intracellular acidosis. We investigated whether overexpression of CF6 contributes to diabetes and hypertension by intracellular acidosis.
Methods
Transgenic mice overexpressing CF6 (also known as ATP5J) were generated, and physiological, biochemical and molecular biology studies were performed.
Results
CF6 overexpression elicited a sustained decrease in intracellular pH in tissues (aorta, kidney, skeletal muscle and liver, with the exception of adipose tissue) that express its receptor, the β-subunit of ecto-F1Fo complex. Consistent with the receptor distribution, phospho-insulin receptor β, phosphoinositide 3-kinase activity and the phospho-Akt1:total Akt1 ratio were all decreased in the skeletal muscle and the liver in transgenic compared with wild-type mice, resulting in a decrease of plasma membrane-bound GLUT4 and an increase in hepatic glucose production. Under a high-sucrose diet, transgenic mice had insulin resistance and mild glucose intolerance; under a high-salt diet, they had elevated blood pressure with increased renal RAS-related C3 botulinum substrate 1 (RAC1)-GTP, which is an activator of mineralocorticoid receptor.
Conclusions/interpretation
Through its action on the β-subunit of ecto-F1Fo complex, which results in intracellular acidosis, CF6 plays a crucial role in the development of insulin resistance and hypertension. This finding might advance our understanding of the mechanisms underlying diabetes and hypertension, possibly also providing a novel therapeutic target against cardiovascular disease.
Similar content being viewed by others
Introduction
In ATP synthase (F1Fo complex), the molecular rotary motor F1-ATPase rotates in an anticlockwise direction to hydrolyse ATP [1], whereas its partner motor Fo, which is embedded in an inner membrane, rotates in a clockwise direction by a proton flux (Fig. 1a). In the mitochondria, Fo forces F1 to rotate backwards (clockwise), leading to ATP synthesis (Fig. 1b) [2]. In the plasma membrane, where the free energy of ATP hydrolysis is greater, F1 forcefully hydrolyses ATP and inversely rotates Fo to pump protons in the opposite direction, leading to intracellular acidosis (Fig. 1c) [3]. The presence of plasma membrane ATP synthase (ecto-F1Fo complex) has been reported in several types of cells and its novel functions have been disclosed [3–6]. In hepatocytes, ecto-F1Fo complex simulation by apoprotein A-I triggers the endocytosis of holo-high-density lipoprotein particles by a mechanism that depends on the generation of ADP [4]. In endothelial cells, the interaction of the β-subunit of the F1 motor with angiostatin attenuates ATP generation and angiogenesis [5, 6]. The ecto-F1Fo complex acts as receptors for lipid uptake and angiogenesis, but its ligands and functions are not fully understood. We recently identified a circulating peptide coupling factor 6 (CF6) as a novel ligand for the ecto-F1Fo complex; after binding to protrusive F1, CF6 forces Fo to rotate backwards, thereby stimulating the proton-importing transporter at the plasma membrane [3].
Protons regulate cellular function by modulating the charge and structure of macromolecules. Proton-extruding and -importing transport proteins underlie pH homeostasis. Intracellular acidosis from a steady-state value of around 7.2 occurs during pathophysiological conditions such as ischaemia and, in the heart, leads to acute contractile depression, distortion of intracellular Ca2+ signalling and the triggering of electrical arrhythmia [7, 8]. A decline of cardiac intracellular pH by no-flow ischaemia impairs tyrosine phosphorylation of the insulin receptor and activation of downstream components [9]. Extracellular acidosis causes a sustained contractile response in isolated aortas from spontaneously hypertensive and control normotensive rats [10]. Intracellular acidosis increases constrictor tone, in association with simultaneous increases in cytosolic free Ca2+, as reported in barnacle and frog muscle fibres [11, 12]. We and others, moreover, have demonstrated that plasma levels of CF6 were increased in patients with hypertension and diabetes [13, 14]. Overall, the above suggests that CF6 might contribute to diabetes and hypertension by intracellular acidosis.
Despite advances in pharmacological treatments, diabetes with hypertension continues to be a major public health problem with high morbidity and mortality rates. Here, we show that chronic stimulation of the ecto-F1Fo complex by CF6 overexpression triggers activation of RAS-related C3 botulinum substrate 1 (RAC1), a member of the Rho family GTPases, in the kidney; via sustained intracellular acidosis, it also triggers inhibition of tyrosine phosphorylation of the insulin receptor and downstream components in skeletal muscle and liver. These findings might advance our understanding of mechanisms underlying diabetes and hypertension, and also provide a novel therapeutic target against cardiovascular disease.
Methods
Construction of vectors and generation of CF6-overexpressing transgenic mice
A gene for the secretion signal of human calcitonin was fused to a gene for the mature ATP synthase CF6 (Asn 33-Ala 108). The fused gene was subcloned into pNE plasmid, in which the β-globin promoter of pdKCR-dhfr plasmid was replaced by human elongation factor-1α promoter. The resultant recombinant plasmid was digested with PvuII and Aor51HI to generate a 2.8 kb DNA fragment consisting of the human elongation factor 1 alpha promoter, the secretion signal–CF6 fused gene and the SV40 polyA additional sequence. The DNA fragment was then micro-injected into the pronuclei of single-cell fertilised mouse embryos to generate transgenic mice. Using COS cells, we confirmed that the protein produced was released outside the cells as mature human CF6 (Asn33-Ala108). CF6 transgenic mice and wild-type littermate mice C57BL/6J (Japan Cler, Tokyo, Japan) were maintained on standard rat chow with free access to water.
Cell culture
The mouse skeletal muscle cell line C2C12 and human hepatocyte cell line HepG2 (both from American Type of Cell Culture, Manassas, VA, USA) were cultured in DMEM supplemented with 10% (vol./vol.) fetal bovine serum.
Diet study
Mice were fed normal chow until the age of 11 weeks, followed by a high-salt diet (8% [wt/wt] salt; Oriental Yeast, Tokyo, Japan) or a high-sucrose diet (AIN-93G, 20% [wt/wt] sucrose; Oriental Yeast, Tokyo, Japan). The composition of the high-sucrose diet was 7% (wt/wt) safflower oil, 20% (wt/wt) casein, 20% (wt/wt) sucrose, 5% (wt/wt) cellulose, (3.5%) wt/wt mineral mixture and 1% (wt/wt) vitamin mixture.
Blood pressure measurement
Systolic and diastolic arterial blood pressure was measured by the tail-cuff method in conscious mice, using a Softron BP-98A (Softron, Tokyo, Japan). Blood pressure was measured ten times per day for four consecutive days and a mean value was generated for each individual mouse.
Glucose tolerance test
Glucose tolerance tests using 2 mg/g (glucose per body weight) were conducted in mice that had been fasted for 12 h. The plasma was sampled from the tail vein before, and at 0.5, 1.0 and 1.5 h after oral administration of glucose; quantification was done with a glucometer (Abbott Diabetes Care, Tokyo, Japan). Insulin was measured by sandwich ELISA kits (Crystal Chem, Downers Grove, IL, USA).
Sampling from portal vein
Under anaesthesia (ketamine 75 mg/kg, xylazine 7.5 mg/kg), the abdomen was opened through a midline incision and the portal vein and inferior vena cava identified. Blood samples were obtained simultaneously from the portal vein and inferior vena cava using a 28-gauge needle and glucose levels determined with a glucometer.
Intraperitoneal injection of drugs
Amiloride, an inhibitor of proton-extruder Na+-H+ exchangers, or an anti-CF6 antibody was injected intraperitoneally for 2 or 3 consecutive days at 50 mg/kg or 113 μg/kg, respectively.
Measurement of intracellular pH
31P-Magnetic resonance spectroscopy (MRS) of the femoral skeletal muscle and the liver was performed using the 4.7 T JASTEC (Tokyo, Japan) horizontal magnet with the mouse in a supine position and a coil (20 mm surface diameter) under the muscle and the liver. Spectra were acquired using a 0.5 s repetition time and 50 μs pulse width. Relative concentrations of inorganic phosphate and phosphocreatinine (PCr) were obtained using a time-domain fitting routine and corrected for partial saturation. Intracellular pH was calculated from the chemical shift of the Pi peak relative to PCr (δPi), measured in ppm, using the equation: \( {\text{pH}} = 6.75 + \log [(\delta {\text{Pi}} - 3.27)/(5.69 - \delta {\text{Pi}})] \). Intracellular pH in the cultured cells was measured using BCECF-AM (Molecular Probes, Eugene, OR, USA) with a luminescence spectrophotometer (Shimazu 5000; Shimazu, Tokyo, Japan).
Measurement of 3H uptake
3H-labelled water (0.01 MBq/g body weight in 200 μl PBS) (New England Nuclear, Boston, MA, USA) was injected into the peritoneal cavity under anaesthesia (ketamine 75 mg/kg, xylazine 7.5 mg/kg) and the 3H level counted in each tissue with a liquid scintillation counter after 15 min.
RAC1-GTPase activation assay
RAC1-GTP levels were determined using a pull-down assay kit (STA-405; Cell Biolabs, San Diego, CA, USA).
Measurement of insulin signalling in tissue
Phospho-insulin receptor β (Tyr1150/1151), phospho-IRS-2 (panTyr), total Akt1 and phospho-Akt1 (ser 473) were measured by sandwich ELISA kits (Cell Signaling Technology, Danvers, MA, USA). IRS-1, GLUT4 and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) were measured by western blot analysis using anti-IRS-1 and anti-GLUT4 antibodies (Santa Cruz Biotechnology, Santa Cruz, CA, USA). G6pase (also known as G6pc) and Pepck (also known as Pck1) were measured by RT-PCR. Phosphoinositide 3-kinase (PI3K) activity in the lysates was evaluated using a PI3K ELISA kit (K1000; Echelon Biosciences, Salt Lake City, UT, USA). The plasma membrane of the muscle was obtained as in Stuart et al. [15] and checked by cadherin.
Measurement of insulin signalling in cultured cells
Phosphorylation of c-Src (tyrosine), 3-phosphoinositide-dependent kinase-1 (PDK-1) (tyrosine 9) and IRS-1 (serine 307) in C2C12 cells was analysed by western blotting using anti-phospho-cSrc, anti-phospho-PDK-1 and anti-IRS-1 antibodies (Cell Signaling). Tsc1 and Tsc2, as well as Mtor and S6k (also known as Rps6kb1) were measured by real-time RT-PCR according to the protocol supplied with the kit (TaqMan Gold RT-PCR; Applied Biosystems, Foster City, CA, USA). Cultured C2C12 cells and HepG2 cells were incubated for 45 min in pH-indicated HEPES-buffered solution at 37°C and under 5% CO2, after which insulin at 1 × 10−4 mol/l was added. After 15 min, cells were lysed by lysis buffer and phospho-insulin receptor β (Tyr1150/1151) was measured by sandwich ELISA kits (Cell Signaling).
Histological analysis of the endocrine pancreas
Isolated pancreas was processed for paraffin embedding, and 2 μm sections were cut and mounted on glass slides. Images of pancreatic tissue and islets were captured on a computer through a microscope connected to a camera (Olympus, Tokyo, Japan).
Statistical analysis and ethical considerations
Results are expressed as mean±SEM. Differences between groups were examined for statistical significance using Student’s t test or ANOVA with Bonferroni’s test. The experimental protocol was approved by the Ethics Committee for Animal Experimentation of Hirosaki University School of Medicine.
Results
Characterisation of CF6-overexpressing transgenic mice
The introduced CF6 gene was expressed in all tissues due to use of human elongation factor 1α promoter, the level being equivalent to that of endogenous mouse Cf6 expression in the aorta, pancreas, liver, skeletal muscle and adipose tissue (Fig. 2a). In parallel with a twofold increase in gene expression, the plasma level of total (human plus mouse) CF6, assessed by western blot analysis, was two times higher in transgenic than in wild-type mice (Fig. 2b). The plasma level of human CF6 related to the introduced gene was 6.98 ± 0.46 ng/ml in transgenic mice (Fig. 2c). We and others had previously reported that the plasma level of CF6 was increased by twofold in patients with coronary heart disease, hypertension, end-stage renal disease and stroke, compared with that in healthy participants [13, 16–19]. Thus, the plasma level of CF6 in transgenic mice was noted to be increased as compared with wild-type mice to a degree similar to that seen in patients with cardiovascular diseases. With regard to the receptor of CF6, the β-subunit of plasma membrane F1Fo complex was expressed in the aorta, kidney, skeletal muscle and liver, but not in adipose tissue, and was of similar abundance in transgenic and wild-type mice (Fig. 2d). Recent evidence has also confirmed that the β-subunit is expressed at the surface of cultured vascular endothelial cells and smooth muscle cells [20, 21]. Consistent with the distribution of ecto-F1Fo complex, proton uptake at 15 min after injection of 3H-labelled water into the intraperitoneal space was increased in the aorta, kidney, skeletal muscle and liver of transgenic compared with wild-type mice (Fig. 2e). As shown in Fig. 2f, the intracellular pH value measured by 31P-MRS was decreased in the skeletal muscle of transgenic mice to 6.96 ± 0.03 compared with 7.05 ± 0.02 units in wild-type mice; it was also decreased in liver of transgenic mice, to 7.0 ± 0.04 units compared with 7.16 ± 0.04 unit in wild-type mice (Fig. 2g). Administration of CF6 to cultured vascular endothelial cells, smooth muscle cells, the mouse skeletal muscle cell line C2C12 and the human hepatocyte cell line HepG2 also confirmed the decrease in intracellular pH measured by a pH-sensitive dye (BCECF-AM). The above changes were all abolished by treatment with efrapeptin, an inhibitor of the F1 motor (see electronic supplementary material [ESM] Fig. 1).
Baseline characteristics in transgenic mice overexpressing CF6. a The expression of human CF6 mRNA in transgenic (TG) mice. White bars, mouse Cf6 mRNA; black bars, human CF6 mRNA; WT, wild-type. b The plasma level of total (t) and (c) human (h) CF6; n = 5; **p < 0.01 vs wild-type. d The β-subunit of plasma membrane F1Fo complex in tissue and animal groups as indicated; n = 4; **p < 0.01 vs aorta, kidney, skeletal muscle and liver. e Uptake of 3H in tissue and animal groups as indicated; n = 4; *p < 0.05 vs wild-type (each organ). f MRS in skeletal muscle and (g) liver; n = 4; *p < 0.05 vs wild-type. h Systolic blood pressure in transgenic and wild-type mice on a normal- or high-salt diet; n = 10; *p < 0.05 vs wild-type; † p < 0.05. Ab, anti-CF6 antibody (113 μg/kg). i RAC1-GTP and total RAC1 in the kidney of transgenic and wild-type mice, with effects of extracellular acidification (pH 5.5) and amiloride at 10−3 mol/l on RAC1 activation. n = 5; *p < 0.05 vs wild-type or pH 7.4
Salt-sensitive hypertension under a high-salt diet
Under a normal diet, systolic blood pressure measured by the tail-cuff method in conscious animals was slightly elevated in transgenic mice compared with wild-type littermates (116 ± 2 vs 110 ± 3 mmHg at 15–20 weeks, p < 0.05; Fig. 2h). This is consistent with our previous report that CF6 enhances Ca2+ signalling in cultured vascular smooth muscle cells and causes vasoconstriction in the mesenteric arteriolar network via c-Src activation [21]. A high-salt diet significantly increased systolic and diastolic blood pressure by 21 ± 3 and 17 ± 3 mmHg, respectively, in transgenic, but not in wild-type mice (p < 0.05). Administration of an anti-CF6 antibody at 113 μg/kg for three consecutive days to transgenic mice improved the salt-induced hypertension. Since RAC1, a member of the Rho family GTPases, was recently identified as a determinant molecule for salt-sensitive hypertension via activation of mineralocorticoid receptor [22], we measured RAC1 activity in the kidney of transgenic mice. Pull-down assays revealed that transgenic mice had more active GTPases than control wild-type mice (Fig. 2i). We further examined the role of intracellular pH in RAC1 activation by modulating the status with extracellular acidification and administration of an inhibitor of Na+-H+ exchanger (amiloride). RAC1-GTP was increased by extracellular acidification and amiloride at 1 × 10−3 mol/l in the kidney (Fig. 2i). Furthermore, pretreatment with EGTA-AM for 30 min at 1 × 10−6 mol/l did not prevent acidosis-induced RAC1 activation (Fig. 2i). Thus, intracellular acidosis induced by interaction between CF6 and the ecto-F1Fo complex seems to cause salt-sensitive hypertension in mice.
Insulin resistance under a high-sucrose diet
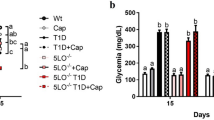
Next, to investigate the role of activation of the ecto-F1Fo complex in glucose catabolism, transgenic mice at the age of 11 weeks were fed a high-sucrose diet for 8 weeks. The trend of body weight change was similar between transgenic and wild-type mice under the high-sucrose diet (Fig. 3a). However, the plasma glucose concentration was higher in transgenic than in wild-type mice from 4–8 weeks after initiation of the high-sucrose diet (Fig. 3b). At 8 weeks of high-sucrose diet, plasma glucose and insulin levels in animals fasted for 12 h were increased in transgenic compared with wild-type mice (glucose 7.38 ± 0.55 vs 5.99±0.06 mmol/l, insulin 120 ± 15 vs 51 ± 9 pmol/l, p < 0.05 for both), suggesting that transgenic mice developed insulin resistance. In the glucose tolerance test, plasma glucose was higher up to 1.50 h (p < 0.05, two-way ANOVA; Fig. 3c), while insulin levels at baseline and at 1 h were twofold higher in transgenic than in wild-type mice (112 ± 13 vs 51 ± 9 pmol/l and 192 ± 20 vs 69 ± 9 pmol/l, p < 0.05 for both; Fig. 3d). Hepatic glucose release, which was evaluated by the increase of plasma glucose between portal vein and inferior vena cava, was enhanced in transgenic mice (Fig. 3e). We further investigated the role of tissue acidosis in the genesis of insulin resistance and glucose intolerance by modulating the extent of intracellular acidosis using amiloride and an anti-CF6 antibody. Intraperitoneal administration of amiloride, an inhibitor of proton-extruder Na+-H+ exchangers, at 50 mg/kg for 2 days worsened the plasma glucose level (Fig. 3f). In contrast, administration of an anti-CF6 antibody at 113 μg/kg for 3 consecutive days improved the plasma glucose level (Fig. 3g). These results are compatible with the hypothesis that tissue acidosis may be related to the genesis of insulin resistance and glucose intolerance. Overall, intracellular acidosis by interaction between CF6 and the ecto-F1Fo complex seems to underlie the molecular mechanisms of salt-sensitive hypertension and insulin resistance.
Diet-induced insulin resistance in transgenic mice. a Trend of body weight in transgenic (TG) (squares) and wild-type (WT) (diamonds) mice on the high-sucrose (HS) diet; n = 13. b Plasma glucose concentration in transgenic and wild-type mice before and after the high-sucrose diet; n = 13. c Trend of plasma glucose level in glucose tolerance test; n = 9. d Trend of plasma insulin level in glucose tolerance test; n = 9. b–d *p < 0.05 vs wild-type at the same age or time; † p < 0.05 by two-way ANOVA. e Hepatic glucose release; n = 4; *p < 0.05 vs portal. IVC, inferior vena cava. f Effect of intraperitoneal administration of amiloride (50 mg/kg for 2 days, vertical arrows) on plasma glucose; n = 4; *p < 0.05 vs day 0. g Effect of intraperitoneal administration of anti-CF6 antibody (113 μg/kg for three consecutive days, vertical arrows) on plasma glucose; n = 4; *p < 0.05 vs day 0
Molecular mechanism for the genesis of insulin resistance
Next we investigated the molecular mechanism for the genesis of insulin resistance by evaluating proteins related to insulin signalling. Phospho-insulin receptor β (Tyr1150/1151) was decreased in skeletal muscle and liver of transgenic compared with wild-type mice, but was of similar abundance in adipose tissue (Fig. 4a). IRS-1 was decreased by 64 ± 9% in transgenic compared with wild-type mice in skeletal muscle (n = 5, p < 0.05), while phospho-IRS-2 (panTyr) was decreased in liver of transgenic compared with wild-type mice (Fig. 4b,c). Consistent with impairment of upstream signalling, PI3K activity and the ratio of phospho-Akt1 (ser 473) to total Akt1 were both decreased in skeletal muscle and liver of transgenic compared with wild-type mice (Fig. 4d,e). Transgenic mice exhibited decreases in plasma membrane-bound GLUT4 in skeletal muscle (by 69 ± 11%; n = 5, p < 0.05) compared with wild-type mice, despite having no difference in the total fraction of GLUT4 (Fig. 4f). The expression of G6pase and Pepck was increased by 54 ± 17% and 41 ± 9%, respectively, in the liver of transgenic mice (n = 5, p < 0.05 for both). The area of islets in the pancreas was greater in transgenic than in wild-type mice (Fig. 4g,h,i). To further investigate the role of intracellular pH in the phosphorylation of insulin receptor β, the mouse skeletal muscle cell line C2C12 and human hepatocyte cell line HepG2 were exposed to extracellular acidification and amiloride. Administration of amiloride and the decrease in extracellular pH impaired insulin-dependent (1 × 10−4 mol/l insulin for 15 min) phosphorylation of insulin receptor β in a concentration-dependent manner in both kinds of cells (Fig. 4j,k). We also examined the effect of pretreatment with EGTA-AM at 1 × 10−6 mol/l for 30 min on phosphorylation of insulin receptor β and found that phosphorylation was not prevented.
Mechanism for diet-induced insulin resistance in transgenic (TG) mice fed an 8-week high-sucrose diet. a Phospho-insulin receptor β (P-IRβ) (Tyr1150/1151) in tissue (as indicated) of transgenic and wild-type (WT) mice; n = 6. b IRS-1 and (c) phospho-IRS-2 abundance in tissue and mouse groups as indicated; n = 5. d PI3K activity in tissue as indicated; n = 6. e The ratio of phospho-Akt1 (ser 473) to total Akt1 in tissue as indicated (n = 6). f Plasma membrane-bound GLUT4 in skeletal muscle from mice as labelled; n = 5. g Representative histology of the pancreas of mice as labelled. h Beta cell area and (i) the size of each islet in mouse groups; n = 6. a–i *p < 0.05 vs wild-type. j Effects of extracellular acidification and amiloride at 1 × 10−3 and 1 × 10−4 mol/l on phospho-insulin receptor β (Tyr1150/1151) in C2C12 and (k) HepG2 cells; n = 5; *p < 0.05 vs pH 7.4. epH, extracellular pH
Molecular mechanisms for the decrease in IRS-1 protein
To investigate the molecular mechanisms for the decrease in IRS-1 protein in skeletal muscle, we examined the effect of CF6 on IRS-1 in the mouse skeletal muscle cell line C2C12. It is known that increased PDK-1 activity induces phosphorylation of Ser307 on IRS-1 and results in its dissociation from the insulin receptor, triggering proteasome-dependent degradation [23, 24].
On the other hand, increased ribosomal protein S6 kinase activity previously resulted in enhanced IRS-1 phosphorylation on amino acid residues Ser636/639 and Ser1101 [23, 25, 26], leading to a reduction of IRS-1 levels [27]. The protein kinase, mammalian target of rapamycin (mTOR), leads to phosphorylation and activation of S6 kinase [23, 24], and activation of the function of tuberous sclerosis complex (TSC)1 and TSC2, which are upstream inhibitors of the mTOR pathway [28]. We therefore postulated that the increased PDK-1 or S6 kinase activity is responsible for reduced IRS-1 expression in skeletal muscle. CF6 activated tyrosine kinase c-Src by generation of reactive oxygen species (ROS) (Fig. 5a) and led to tyrosine phosphorylation of PDK-1 (Fig. 5b), resulting in phosphorylation of IRS-1 at Ser307 at 30 min (Fig. 5c) and degradation of IRS-1 at 24 h (Fig. 5d). Another pathway for phosphorylation of Ser307 on IRS-1, namely TSC1/2–mTOR–S6 kinase, was not affected by CF6 (data not shown). Overall, the reduction of IRS-1 seems to be dependent on activation of PDK-1 via ROS generation.
Effect of CF6 on insulin signalling in cultured mouse skeletal myocytes (C2C12 cell line). a c-Src activation by CF6; n = 5;*p < 0.05 vs control (Cont); † p < 0.05 for CF6 vs NAC + CF6. NAC, N-acetyl-l-cysteine (10 mmol/l). b Effect of CF6 on PDK-1 and Tyr9 of PDK-1 levels; n = 5; *p < 0.05 vs control; † p < 0.05 for CF6 vs PPI+CF6. PP1, inhibitor of tyrosine kinase c-Src (50 μmol/l). c Phosphorylation of Ser307 on IRS-1 by CF6; n = 5; *p < 0.05 vs time 0. d Degradation of IRS-1 at 24 h by CF6; n = 5; *p < 0.05 vs time 0. e Summary of the mechanism for the linkage of hypertension with diabetes after interaction between CF6 and the ecto-F1Fo complex
Discussion
The major findings of this study were as follows. Chronic stimulation of the ecto-F1Fo complex by CF6 overproduction elicited a sustained decrease in intracellular pH in tissues expressing the receptor of CF6, the β-subunit of ecto-F1Fo complex, i.e. in aorta, kidney, skeletal muscle and liver, but not adipose tissue. Transgenic mice manifested salt-sensitive hypertension with RAC1 activation in the kidney and insulin resistance with impaired tyrosine phosphorylation of insulin receptor. Extracellular acidification and administration of amiloride increased RAC1-GTP in the mouse kidney and impaired insulin-dependent phosphorylation of insulin receptor β in skeletal myocytes and hepatocytes.
First, to investigate whether long-term stimulation of the ecto-F1Fo complex elicits a sustained decrease in intracellular pH, we generated transgenic mice that overexpressed its endogenous activator CF6. We had previously shown that CF6 is first generated as an immature form (1–108 amino acids) in the cytoplasm and released outside the cells as a mature form (33–108 amino acids) after enzymatic deletion of the signal peptide (1–32 amino acids) [20, 29]. We further showed that CF6 attenuates prostacyclin generation by inhibiting cytosolic phospholipase A2 [30] and nitric oxide generation via upregulation of asymmetric dimethylarginine or inhibition of endothelial nitric oxide synthase phosphorylation [31, 32]. CF6 also elevates arterial blood pressure and enhances angiotensin II-induced vasoconstriction in resistance arterioles [21, 33]. In transgenic mice, intracellular pH measured by 31P-MRS was reduced in skeletal muscle and liver, a finding consistent with the distribution of the receptor of CF6, the β-subunit of the ecto-F1Fo complex. Interestingly, chronic stimulation of the ecto-F1Fo complex by CF6 overproduction elicited a sustained decrease in intracellular pH, despite the fact that the proton-extruding transporter might act to prevent excess acidification. The pH value decrease in transgenic mice ranged from 0.1 to 0.15 pH units in skeletal muscle and liver, and proton uptake was increased in the aorta, kidney, skeletal muscle and liver. Overall we confirmed that this mouse maintains the sustained decrease in intracellular pH in tissues expressing the receptor of CF6.
We next analysed the phenotype of transgenic compared wild-type mice with regard to arterial blood pressure. A high-salt diet increased systolic and diastolic blood pressure in transgenic mice, and this salt-induced hypertension was improved by administration of an anti-CF6 antibody. Since RAC1 was recently identified as a determinant molecule for salt-sensitive hypertension via activation of mineralocorticoid receptor [22], we investigated a possible involvement of RAC1 activation in the genesis of salt-sensitive hypertension in transgenic mice. Pull-down assays clearly showed that transgenic mice had more active GTPases in the kidney than wild-type mice, while RAC1-GTP was increased by extracellular acidosis and amiloride administration. Thus, overabundance of CF6 might activate RAC1 by intracellular acidosis and lead to salt-sensitive hypertension. In clinical settings, the intracellular pH of erythrocytes measured by 31P-MRS is decreased by 0.1 units in hypertensive compared with normotensive patients [34]. Moreover, a proton-extruder Na+/H+ exchanger is increased in hypertension and serum ionised calcium is elevated in intracellular acidosis in clinical hypertension [35, 36].
To further investigate the role of activation of the ecto-F1Fo complex in glucose catabolism, transgenic mice were fed a high-sucrose diet for 8 weeks. During the high-sucrose diet, the plasma glucose concentration was higher in transgenic than in wild-type mice, and levels of plasma glucose and insulin after a 12 h fast were increased in the former versus the latter, suggesting that transgenic mice developed insulin resistance. This was also confirmed by a glucose tolerance test and hepatic glucose release. We further showed that intraperitoneal administration of amiloride exacerbated the plasma glucose level, whereas administration of an anti-CF6 antibody ameliorated it. Thus, in addition to salt-sensitive hypertension, the small decrease of 0.1–0.15 pH units seems to cause insulin resistance in mice.
We also investigated the molecular mechanism for the genesis of insulin resistance by evaluating proteins related to insulin signalling. Consistent with the distribution of CF6 receptor ecto-F1Fo complex, phospho-insulin receptor β (Tyr1150/1151) was decreased in skeletal muscle and liver of transgenic mice, while its downstream of IRS-1, IRS-2 and PI3K activity, as well as the ratio of phospho-Akt1 to total Akt1 were attenuated. These changes may result in a decrease of plasma membrane-bound GLUT4, and increased expression of G6pase and Pepck. Although CF6 production is ubiquitous, the tissue-specific effects observed by us depend on levels its receptor. In our in vitro assay, extracellular acidosis and amiloride impaired insulin-dependent phosphorylation of insulin receptor β in the mouse skeletal muscle cell line C2C12 and human hepatocyte cell line HepG2. Therefore, like RAC1 activation in the kidney, intracellular acidosis seems to play an important role in the genesis of insulin resistance via overexpression of CF6. Additionally, the decrease in IRS-1 protein in skeletal muscle seems to be dependent on activation of PDK-1 via ROS generation in cultured C2C12 cells.
It has been demonstrated that metabolic acidosis produces insulin resistance in healthy humans, whereas treatment of metabolic acidosis increases insulin sensitivity and insulin secretion in patients with uraemia [37, 38]. Many recent epidemiological studies have also linked metabolic acidosis indicators to insulin resistance and systemic hypertension [38]. To our knowledge, this is the first report that chronic stimulation of the ecto-F1Fo complex by CF6 overexpression elicits a sustained decrease in intracellular pH in tissues expressing the receptor of CF6 in mice. In addition, tissue acidosis appeared to induce insulin resistance and hypertension. As shown in Fig. 5e, protons regulate cellular function by modulating the charge and structure of macromolecules, such as phosphorylation of RAC1 and dephosphorylation of insulin receptor, and also explain the activation of cSrc and p38 mitogen-activated protein kinase, the other signalling pathways of CF6 [21, 32]. In clinical settings, we and others previously showed that circulating CF6 is elevated in patients with hypertension, acute myocardial infarction, end-stage renal disease, stroke and diabetes [13, 14, 16–18], all of which predispose to the development of atherosclerosis. Given the present finding and the widespread biological actions of CF6, such as inhibition of prostacyclin and nitric oxide [21, 30–33], the reduction of CF6 levels may be an important and useful way to prevent cardiovascular events. To date, we have reported that salt restriction, vitamin C and vitamin B12 plus folic acid lowered plasma levels of CF6 in patients with hypertension and stroke [13, 17], and that peroxisome proliferator-activated receptor γ ligand attenuated CF6 release from cultured vascular endothelial cells [39]. The present findings provide new insights into our understanding of the pivotal role of CF6 in the mechanisms underlying hypertension and diabetes in connection with tissue acidosis; they also shed light on a novel potential therapeutic target in vascular medicine.
Abbreviations
- CF6:
-
Coupling factor 6
- Ecto-F1Fo complex:
-
Plasma membrane ATP synthase
- MRS:
-
31P-Magnetic resonance spectroscopy
- mTOR:
-
Mammalian target of rapamycin
- PCr:
-
Phosphocreatinine
- PDK-1:
-
3-Phosphoinositide-dependent kinase-1
- PI3K:
-
Phosphoinositide 3-kinase
- RAC1:
-
RAS-related C3 botulinum substrate 1
- ROS:
-
Reactive oxygen species
- TSC:
-
Tuberous sclerosis complex
References
Yoshida M, Muneyuki E, Hisabori T (2001) ATP synthase—a marvellous rotary engine of the cell. Nature Rev Mol Cell Biol 2:669–677
Itoh H, Takahashi A, Adachi K et al (2004) Mechanically driven ATP synthesis by F1-ATPase. Nature 427:465–468
Osanai T, Magota K, Tanaka M et al (2005) Intracellular signaling for vasoconstrictor coupling factor 6: novel function of β-subunit of ATP synthase as receptor. Hypertension 46:1140–1146
Martinez LO, Jacquet S, Esteve JP et al (2003) Ectopic β-chain of ATP synthase is an apolipoprotein A-I receptor in hepatic HDL endocytosis. Nature 421:75–79
Moser TL, Stack MS, Asplin I et al (1999) Angiostatin binds ATP synthase on the surface of human endothelial cells. Proc Natl Acad Sci USA 96:2811–2816
Moser TL, Kenan DJ, Ashley TA et al (2001) Endothelial cell surface F1-Fo ATP synthase is active in ATP synthesis and is inhibited by angiostatin. Proc Natl Acad Sci USA 98:6656–6661
Casey JR, Grinstein S, Orlowski J (2010) Sensors and regulators of intracellular pH. Nat Rev Mol Cell Biol 11:50–61
Vaughan-Jones RD, Spitzer KW, Swietach P (2009) Intracellular pH regulation in heart. J Mol Cell Cardiol 46:318–331
Beauloye C, Bertrand L, Krause U et al (2001) No-flow ischemia inhibits insulin signaling in heart by decreasing intracellular pH. Circ Res 88:513–519
Rohra DK, Saito S, Ohizumi Y (2003) Extracellular acidosis results in higher intracellular acidosis and greater contraction in spontaneously hypertensive rat aorta. Eur J Pharmacol 465:141–144
Lea TJ, Ashley CC (1978) Increase in free Ca2+ in muscle after exposure to CO2. Nature 275:236–238
Rink TJ, Tsien RY, Warner AE (1980) Free calcium in Xenopus embryos measured with ion-selective microelectrodes. Nature 283:658–660
Osanai T, Sasaki S, Kamada T et al (2003) Circulating coupling factor 6 in human hypertension: role of reactive oxygen species. J Hypertens 21:2323–2328
Li XL, Xing QC, Gao YY et al (2007) Plasma level of mitochondrial coupling factor 6 increases in patients with type 2 diabetes mellitus. Int J Cardiol 117:411–412
Stuart CA, Howell MEA, Zhang Y, Yin D (2009) Insulin-stimulated translocation of glucose transporter (GLUT) 12 parallels that of GLUT4 in normal muscle. J Clin Endocrinol Metab 94:3535–3542
Osanai T, Nakamura M, Sasaki S et al (2003) Plasma concentration of coupling factor 6 and cardiovascular events in patients with end-stage renal disease. Kidney Int 64:2291–2297
Osanai T, Fujiwara N, Sasaki S et al (2010) Novel pro-atherogenic molecule coupling factor 6 is elevated in patients with stroke: a possible linkage to homocysteine. Ann Med 42:79–86
Ding WH, Chu SY, Jiang HF et al (2004) Plasma mitochondrial coupling factor 6 in patients with acute myocardial infarction. Hypertens Res 27:717–722
Chai SB, Hui YM, Li XM, Tang CS (2007) Plasma level of mitochondrial coupling factor 6 increases in patients with coronary heart disease. Circ J 71:693–697
Osanai T, Okada S, Sirato K et al (2001) Mitochondrial coupling factor 6 is present on the surface of human vascular endothelial cells and released by shear stress. Circulation 104:3132–3136
Osanai T, Tomita H, Kushibiki M et al (2009) Coupling factor 6 enhances Src-mediated responsiveness to angiotensin II in resistance arterioles and cells. Cardiovasc Res 81:780–787
Shibata S, Nagase M, Yoshida S et al (2008) Modification of mineralocorticoid receptor function by Rac1 GTPase: implication in proteinuric kidney disease. Nat Med 14:1370–1376
Um SH, Frigerio F, Watanabe M et al (2004) Absence of S6K1 protects against age- and diet-induced obesity while enhancing insulin sensitivity. Nature 431:200–205
Tremblay F, Marette A (2001) Amino acid and insulin signaling via the mTOR/p70 S6 kinase pathway. A negative feedback mechanism leading to insulin resistance in skeletal muscle cells. J Biol Chem 276:38052–38060
Bouzakri K, Roques M, Gual P et al (2003) Reduced activation of phosphatidylinositol-3 kinase and increased serine 636 phosphorylation of insulin receptor substrate-1 in primary culture of skeletal muscle cells from patients with type 2 diabetes. Diabetes 52:1319–1325
Li Y, Soos TJ, Li X et al (2004) Protein kinase C theta inhibits insulin signaling by phosphorylating IRS1 at Ser(1101). J Biol Chem 279:45304–45307
Harrington LS, Findlay GM, Gray A et al (2004) The TSC1-2 tumor suppressor controls insulin-PI3K signaling via regulation of IRS proteins. J Cell Biol 166:213–223
Li Y, Corradetti MN, Inoki K, Guan KL (2004) TSC2: filling the GAP in the mTOR signaling pathway. Trends Biochem Sci 29:32–38
Osanai T, Magota K, Okumura K (2009) Coupling factor 6 as a novel vasoactive and proatherogenic peptide in vascular endothelial cells. Naunyn Schmiedebergs Arch Pharmacol 380:205–214
Osanai T, Kamada T, Fujiwara N et al (1998) A novel inhibitory effect on prostacyclin synthesis of coupling factor 6 extracted from the heart of spontaneously hypertensive rats. J Biol Chem 273:31778–31783
Tanaka M, Osanai T, Murakami R et al (2006) Effect of vasoconstrictor coupling factor 6 on gene expression profile in human vascular endothelial cells: enhanced release of asymmetric dimethylarginine. J Hypertens 24:489–497
Kumagai A, Osanai T, Katoh C et al (2008) Coupling factor 6 downregulates platelet endothelial cell adhesion molecule-1 via c-Src activation and acts as a proatherogenic molecule. Atherosclerosis 200:45–50
Osanai T, Tanaka M, Kamada T et al (2001) Mitochondrial coupling factor 6 as a novel endogenous vasoconstrictor. J Clin Invest 108:1023–1030
Resnick LM, Gupta RK, Sosa RE, Corbett ML, Laragh JH (1987) Intracellular pH in human and experimental hypertension. Proc Natl Acad Sci USA 84:7663–7667
Furspan PB, Bohr DF (1985) Lymphocyte abnormalities in three types of hypertension in the rat. Hypertension 7:860–866
Erne P, Bolli P, Bürgisser E, Bühler FR (1984) Correlation of platelet calcium with blood pressure. Effect of antihypertensive therapy. N Engl J Med 310:1084–1088
Mak RH (1998) Effect of metabolic acidosis on insulin action and secretion in uremia. Kidney Int 54:603–607
Souto G, Donapetry C, Calviño J, Adeva MM (2011) Metabolic acidosis-induced insulin resistance and cardiovascular risk. Metab Syndr Relat Disord 9:247–253
Tomita H, Osanai T, Toki T et al (2005) Troglitazone and 15-deoxy-deta 12, 14-prostaglandin J2 inhibit shear-induced coupling factor 6 release in endothelial cells. Cardiovasc Res 67:134–141
Acknowledgements
This work was supported by Grant-in-Aid for Scientific Research (19590800 to T. Osanai) from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Contribution statement
All authors contributed to conception and design, or analysis and interpretation of data, and to drafting the article or revising it critically for important intellectual content. All the authors gave final approval of the version to be published.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Fig. 1
PDF 39.2 kb
Rights and permissions
About this article
Cite this article
Osanai, T., Tanaka, M., Magota, K. et al. Coupling factor 6-induced activation of ecto-F1Fo complex induces insulin resistance, mild glucose intolerance and elevated blood pressure in mice. Diabetologia 55, 520–529 (2012). https://doi.org/10.1007/s00125-011-2341-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-011-2341-z