Abstract
Aims/hypothesis
We investigated whether oltipraz, a nuclear respiratory factor 2 alpha subunit (NRF2) activator, improves insulin sensitivity and prevents the development of obesity in mice.
Methods
C57BL/6J mice were fed with a low-fat diet (10% of energy as fat), a high-fat diet (HFD) (45% of energy as fat) or a HFD with oltipraz for 28 weeks. The effects of oltipraz on body weight, fat content, glucose disposal, insulin signalling, metabolic profiles and endogenous NRF2 functional status in the three groups of mice were investigated.
Results
Oltipraz prevented or significantly attenuated the effect of HFD on glucose disposal, body weight and fat gain. Impairment of protein kinase B/Akt phosphorylation in this HFD-fed mouse model in response to intraperitoneal insulin injection was observed in adipose tissue, but not in the muscles, accompanied by inhibition of AMP-activated protein kinase signalling and activation of p70S6 kinase, as well as reduced GLUT4 content. These defects were attenuated by oltipraz administration. Nuclear content of NRF2 in adipose tissue was reduced by HFD feeding, associated with increased Keap1 mRNA expression and reduced production of haem oxygenase-1 and superoxide dismutase, increased protein oxidation, decreased plasma reduced:oxidised glutathione ratio and the appearance of macrophage marker F4/80. These defects were also restored by oltipraz. Finally, oltipraz attenuated HFD-induced inducible nitric oxide synthase overproduction.
Conclusions/interpretation
Impairment of the endogenous redox system is important in the development of obesity and insulin resistance in chronic HFD feeding. NRF2 activation represents a potential novel approach in the treatment and prevention of obesity and diabetes.
Similar content being viewed by others
Introduction
Insulin resistance occurs in nearly one third of the population and is implicated in obesity, diabetes, hypertension, and cardiovascular and other metabolic disorders [1]. Mechanisms underlying the development of insulin resistance remain to be fully elucidated [2]. Several lines of evidence suggest that oxidative stress plays a critical role. First, agents inducing insulin resistance may cause oxidative stress, as documented in several cell models of insulin resistance, including treatment of 3T3-L1 cells with TNF or dexamethasone [3]. Second, in animal models, including obese mice and intralipid- or hyperglycaemia-infused mice, reactive oxygen species (ROS) and inducible nitric oxide synthase (iNOS)-mediated nitric oxide overproduction were associated with the development of insulin resistance [4–7]. Third, antioxidant administration or iNOS inhibition may reverse insulin insensitivity in a variety of animal models of insulin resistance [6, 7]. It has been suggested that ROS- or nitric oxide-induced defects of insulin signalling are due to direct impairment of insulin signalling molecules by protein oxidation or nitrosylation [8, 9]. Several signalling abnormalities caused by alteration of redox homeostasis may also indirectly impair insulin signalling [10], as exemplified by inflammatory signalling and endoplasmic reticulum (ER) stress [11, 12].
Since ROS overproduction is an important contributor to oxidative stress [13], it is important to explore the role of the endogenous antioxidant system in the prevention of insulin insensitivity in vivo. Nuclear respiratory factor 2 alpha subunit (NRF2) is a key molecule of the endogenous antioxidant system [14]. This transcription factor upregulates several antioxidant enzymes to maintain redox homeostasis. In the absence of oxidative stress, NRF2 resides in the cytoplasm together with its repressor kelch-like ECH-associated protein 1 (KEAP1). It is generally accepted that following ROS overproduction or in response to electrophilic reagent treatment, NRF2 detaches from KEAP1 and is translocated into the nucleus, leading to upregulated production of antioxidant enzymes [14], although a very recent study suggested that electrophilic reagent may lead to covalent binding of NRF2 with KEAP1 [15]. Several downstream targets of NRF2, including glutathione S-transferases, haem oxygenase-1 (HO-1) and superoxide dismutase (SOD), were able to improve insulin sensitivity [2, 10, 14, 16–19]. Moreover, inflammatory signals and ER stress can be repressed by NRF2 [12]. It is therefore reasonable to suggest that endogenous NRF2 signalling status affects the development of insulin insensitivity.
Here we examined the functional status of the NRF2 system in a high-fat diet (HFD) mouse model in which the development of obesity and insulin insensitivity was relatively slow because the HFD used by us had 45%, instead of 60% of energy from fat. We found that long-term feeding of this HFD induced oxidative stress and repressed endogenous NRF2 function. Administration of oltipraz, an NRF2 activator [20], prevented the development not only of oxidative stress but also of insulin insensitivity, as well as of obesity and other related metabolic abnormalities.
Methods
Reagents
Oltipraz was purchased from LKT Laboratories (St Paul, MN, USA). Antibodies against protein kinase B (PKB), phosphorylated PKB (Ser473), AMP-activated protein kinase (AMPK), phosphorylated AMPK (T172), phosphorylated acetyl-CoA carboxylase, eukaryotic translation initiation factor 4E (4E-BP1), phosphorylated 4E-BP1 (p-4E-BP1), RPS6-p70-protein kinase (S6K), p-70S6K, eukaryotic initiation factor 2 α subunit (eIF2α, Ser51), SOD2 and histone-3 were obtained from Cell Signaling Technology (Beverly, MA, USA). iNOS and endothelial nitric oxide synthase antibodies were from Alpha Diagnostic International (San Antonio, TX, USA). Nrf2 (also known as Nfe2l2) small interfering RNA (siRNA), the control scramble siRNA, NRF2, HO-1 and F4/80 antibodies were from Santa Cruz Biotechnology (Santa Cruz, CA, USA). GLUT1 and GLUT4 antibodies, kits for glucose, cholesterol, NEFA, HDL and TNFα ELISA assays were from Abcam (Cambridge, MA, USA). Triacylglycerol assay kit was from Cayman Chemical (Ann Arbor, MI, USA). Leptin/insulin ELISA kits were from Crystal Chem (Downers Grove, IL, USA). Adiponectin ELISA kit was from R&D Systems (Minneapolis, MN, USA). HepG2 cells were purchased from ATCC (Manassas, VA, USA). Reduced glutathione:oxidised glutathione (GSH:GSSG) assay kit was from Oxford Biomedical Research (Oxford, MI, USA).
Animal care and treatment
Male C57BL/6J mice from Jackson Laboratory (Bar Harbor, ME, USA) were housed five per cage under conditions of constant temperature (22°C), and a light/dark cycle of 12 h with free access to food and water. From 5 weeks of age mice had free access to a low-fat diet (LFD) (control diet, 10% energy from fat), HFD (45% energy from fat) or HFD diet plus oltipraz (0.75 g/kg diet). Diets were made up by Harlan Teklad (Madison, WI, USA) according to customer specifications. The animal experiments were performed in accordance with the Guide for Care and Use of Experimental Animals (University Health Network, Toronto, ON, Canada).
Magnetic resonance imaging assessment of total fat mass and lipid content
Magnetic resonance imaging (MRI) scans were performed (7 tesla Biospec 70/30 USR; Bruker BioSpin MRI, Ettlingen, Germany). Mice in a prone position were advanced into a cylindrical volume resonator, with a receive-only surface coil placed posterior to the liver. A respiratory pad provided physiological monitoring (SA Instruments, Stony Brook, NY, USA). Whole-body quantification of fat relied on fat hyperintensity in T2-weighted RARE images, using the volume resonator for RF transmission and reception. Respiratory-gated PRESS magnetic resonance spectroscopy was applied to evaluate intra-hepatic water and lipid contents, using the surface coil for RF reception. The PRESS technique was also used to evaluate intra-muscular water and lipid contents, using muscle within proximity of the spinal cord. The RARE variable set included: echo time (TE) 24 ms; repetition time (TR) 5,000 ms; 250 × 250 μm in-plane resolution over 40 × 40 mm field-of-view (160 × 160 matrix) with 89.286 kHz readout bandwidth. A total of 44 contiguous 2-mm vertical slices provided whole-body coverage. Respiratory motion artefacts were suppressed using nine averages, for a total acquisition time of 15 min. Total fat mass quantification used custom image segmentation software (Matlab; The Mathworks, Natick, MA, USA), which robustly separated fat from non-fat voxels within each image. The number of voxels within each mask image was counted and scaled to volume (0.125 mm3 per voxel). The PRESS variable sets included: TE/TR 20/5,000 ms; 2 × 2 × 2 mm PRESS voxel, 2,048 points; 0.98 Hz/point; 64 averages; 5 min and 40 s total data acquisition time. jMRUI (The MRUI Project; www.mrui.uab.es/mrui/) supported basic spectral processing, and Matlab supported quantification of areas under water (centred at 4.7 ppm) and fat resonances (defined as the summation centred at 1.3 and 0.9 ppm).
Glucose, insulin and pyruvate tolerance tests
Mice were fasted overnight for the glucose tolerance test or fasted for 6 h for insulin and pyruvate tolerance tests. Following the fasting, glucose (2 g/kg), insulin (0.65 U/kg) or pyruvate (2 g/kg) was injected i.p. Blood samples collected from the tail vein were used for glucose measurement.
Determination of blood biochemistry and liver triacylglycerol content
Ambient levels of plasma glucose, triacylglycerol, total cholesterol, NEFA and HDL after overnight fasting were measured using kits following manufacturer’s instruction. Liver triacylglycerol content was determined as described [21].
Tissue protein preparation, nuclear protein extraction and western blot analysis
Nuclear extracts were prepared according to Carey et al. [22]. Methods for tissue protein preparation and western blotting have been previously described [23].
Determination of macrophage infiltration in adipose tissue
Paraffin-embedded adipose tissues were subjected to F4/80 immunostaining for determination of macrophage infiltration.
Quantitative real-time RT-PCR
Real-time PCR was performed using iQ Sybr Green (Bio-Rad, Mississauga, ON, Canada) and the Rotorgene according to the protocol provided by the manufacturer. The relative mRNA transcript levels were calculated according to the \( {2^{{ - \Delta \Delta {C_t}}}} \) method [24].
Assessment of redox status
GSH and GSSG were determined using a GSH:GSSG kit (Oxford Biomedical Research) according to the manufacturer’s instructions. Protein oxidation was detected using a protein oxidation detection kit (OxyBlot; Millipore, Kingston, ON, Canada), which contains the antibody against dinitrophenol.
siRNA knockdown
Methods for Nrf2 knockdown with siRNA in the HepG2 cell line are detailed in the Electronic supplementary material (ESM) Methods.
Statistics
All results are presented as mean ± SEM. Statistical significance was assessed by ANOVA. A p value of p < 0.05 was considered to be statistically significant.
Results
Long-term oltipraz administration prevents HFD feeding-induced whole-body insulin resistance
Insulin resistance in C57BL/6J mice has often been induced in the short term by feeding a diet containing poly-saturated fatty acid (45%) or with a mixed fatty acid diet with 60% energy from fat. Here we employed soybean oil as the fat source in the HFD. In addition, the fat content of the HFD was relatively low (45%). In this HFD mouse model, the development of obesity and insulin resistance was slow (see below). The mice were fed with LFD, HFD or HFD plus oltipraz for 28 weeks. We measured levels of plasma glucose, insulin, leptin, adiponectin, triacylglycerol and HDL. As shown in Table 1, the fasting blood glucose level, total cholesterol and NEFA showed no significant differences among the three groups of animals, while neither HFD nor oltipraz administration had any significant effect on plasma HDL or adiponectin levels. However, oltipraz significantly attenuated HFD-induced elevation of plasma insulin and leptin levels. The triacylglycerol level was significantly higher in HFD mice than in LFD mice, while oltipraz administration showed a trend towards reducing plasma triacylglycerol content. Together, although the deleterious effects of HFD were modest and not all variables examined showed significant alterations, the protective effect of oltipraz was appreciable.
To evaluate the functional impact of long-term oltipraz administration on whole-body glucose metabolism, we conducted an intraperitoneal glucose tolerance test (IPGTT). A representative IPGTT performed at 20 weeks is presented in Fig. 1a. Blood glucose levels were higher in HFD mice than in LFD mice after glucose challenge, while oltipraz treatment significantly improved glucose tolerance in the former. To determine insulin sensitivity more directly, an intraperitoneal insulin tolerance test (IPITT) was performed. Insulin was less effective in lowering glucose level in the HFD mice, while oltipraz administration significantly enhanced insulin-mediated glucose-lowering (Fig. 1b). We then assessed whether the liver was responsible for the improved glucose disposal using an intraperitoneal pyruvate tolerance test (IPPTT). As shown in Fig. 1c, glucose production following pyruvate administration was significantly enhanced in the HFD animals, while oltipraz administration partially inhibited this effect, indicating that increased liver gluconeogenesis induced by HFD can be inhibited by oltipraz.
Long-term oltipraz administration prevents HFD-induced insulin resistance. After the stated period of LFD, HFD or HFD plus oltipraz (OPZ) feeding, IPGTT (n = 5) (20 weeks) (a, b), IPITT (n = 6) (22 weeks) (c, d) and IPPTT (n = 6) (24 weeks) (e, f) were performed on the three groups of mice. Black squares, LFD; black triangles, HFD; black diamonds, HFD + OPZ. † p < 0.05 for LFD vs HFD; ‡ p < 0.05 for HFD vs HFD + OPZ; *p < 0.05, **p < 0.01, ***p < 0.001
Oltipraz administration prevents HFD-induced obesity and lipid accumulation in muscle
In this animal model, the effect of HFD feeding on body weight gain was gradual. A significant difference in body weight appeared at 16 weeks after HFD vs LFD feeding (Fig. 2a). Importantly, oltipraz administration completely inhibited the effect of HFD on body weight gain during the entire experimental period. To specifically examine fat mass, we used MRI. In the LFD-fed animals, the average total fat volume was approximately 3.7 ml. HFD caused an increase to 9.8 ml, while oltipraz treatment of HFD mice reduced this to 4.1 ml (Fig. 2b). Consistent with total fat mass, the weight of epididymal fat pads, representative of visceral fat, was significantly increased by HFD feeding, while oltipraz blocked this stimulation (Fig. 2c). Indeed, the size of adipocytes in HFD-fed mice was greater than in the LFD-fed mice, while oltipraz administration reduced adipocyte size, as shown by haematoxylin and eosin staining (Fig. 2d). Figure 2e shows representative RARE images of cross-sections in the mice with fat displayed as hyperintense tissue.
Long-term oltipraz administration prevents HFD-induced obesity and lipid accumulation in liver and muscle. a Comparison of body weight change of mice fed with LFD (black squares), HFD (black triangles, dashed line) or HFD plus oltipraz (OPZ) (black diamonds) during 28 weeks (n = 10 for LFD and HFD, n = 8 for HFD + OPZ). † p < 0.05 for LFD vs HFD; ‡ p < 0.05 for HFD vs HFD + OPZ. b Total body fat volume assessed by MRI at 26 weeks (n = 4 for all three groups) and (c) weight of epididymal fat pads (n = 8); **p < 0.01. d Haematoxylin and eosin staining shows the sizes of adipocytes from the epididymal fat pad. e Representative RARE images at multiple cross-sections of mice in each cohort. Fat is displayed as a considerable hyperintensity compared with other tissues. Arrows, area of fat (white)
There was no significant difference in liver weight between LFD and HFD mice, while the oltipraz group showed reduced liver weight compared with the HFD group (ESM Fig. 1a). Liver triacylglycerol content was slightly increased by HFD, while the mice treated with HFD and oltipraz showed a triacylglycerol level similar to that of LFD mice, although there were no significantly statistical differences between them (ESM Fig. 1b). MRI assessment revealed that total liver lipid content was significantly increased by HFD, while oltipraz tended to block the effect of HFD (ESM Fig. 1c, d). Together, the above observations suggest that this long-term HFD feeding generated a model of moderate insulin resistance, characterised by a significant increase in fat mass and a modest increase of hepatic lipid content. We also observed a significant increase in liver TNFα induced by HFD feeding and a repressive effect of oltipraz administration on this increase (data not shown). However, this increase did not result in increased plasma TNFα in the HFD group (Table 1).
HFD feeding was also shown to increase muscle triacylglycerol content, which was blocked by oltipraz administration (ESM Fig. 2a). We then assessed intra-muscle lipid content by MRI. As presented in ESM Fig. 2b, c, HFD-fed mice had elevated total lipid content in the gastrocnemius muscle, although the increase did not reach statistical significance. Oltipraz showed a trend to reduce lipid content in mouse muscle. There was no apparent pathological change in liver sections of the three groups by haematoxylin and eosin staining, in contrast to sections of corresponding C57BL/6J mouse groups subjected to HFD with 60% energy from fat (ESM Fig. 3). In our experimental animals, oltipraz administration prevented not only HFD-induced obesity, but also lipid accumulation in insulin-sensitive tissues other than the adipose tissue.
Oltipraz prevents HFD-induced impairments in insulin signalling and GLUT4 depletion in adipose tissue
To explore mechanisms underlying the protective effects of oltipraz during HFD feeding, we first investigated insulin signalling by determining PKB Ser473 phosphorylation in response to insulin in adipose tissue, and soleus and gastrocnemius muscles. In adipose tissue, insulin-stimulated PKB phosphorylation was clearly impaired by HFD, while oltipraz administration restored the response (Fig. 3a). However, this impairment was not observed in soleus (ESM Fig. 4a) or gastrocnemius muscles (ESM Fig. 4b). These results support the notion that adipose tissue is the initial site affected by HFD feeding. Thus, the following investigations were focused on the adipose tissue.
Oltipraz attenuates HFD-induced impairments in insulin signalling and GLUT4 depletion in adipose tissue. Mice on LFD, HFD and HFD + oltipraz (OPZ) diets for 28 weeks were fasted overnight and injected with PBS or insulin for 30 min. Samples from epididymal fat pad (adipose) were prepared for western blotting. Representative blots and densitometry scanning of the blots are shown for (a) PKB, (b) AMPK and acetyl-CoA carboxylase (ACC), (c) 4EBP-1, (d) S6K and (e) GLUT4; n = 3 or 4; *p < 0.05, ***p < 0.001, † p = 0.06. a–d White bars, basal; black bars, insulin-stimulated
Mammalian target of rapamycin (mTOR), along with its downstream targets, p70S6K and 4E-BP1, may function as a negative feedback loop of insulin signalling, while AMPK improves insulin sensitivity by inhibiting the mTOR/p70S6 kinase pathway [25, 26]. In hepatocytes, oltipraz was shown to enhance insulin signalling via AMPK activation-mediated p70S6K inhibition [25]. Here we tested whether the stimulatory effect of oltipraz on AMPK can be detected in our experimental setting in adipose tissue. As shown in Fig. 3b, HFD inhibited AMPK T172 phosphorylation, while oltipraz administration at least partially attenuated the effect of HFD. Correspondingly, the level of phosphorylated acetyl-CoA carboxylase, a known target of AMPK [27], was barely detectable in HFD-fed mice, while oltipraz administration restored its appearance (Fig. 3b). In addition, insulin-stimulated p-4E-BP1 and p-70S6K levels were higher in HFD-fed mice than in LFD-fed mice, while oltipraz partially attenuated the effect of HFD (Fig. 3c, d).
To further investigate the mechanisms by which oltipraz increases the capacity of mice to lower blood glucose, we examined GLUT4 content in adipose tissue in the three groups of mice. The level of GLUT4, which is responsible for insulin-stimulated glucose uptake [28], was reduced in HFD mice, while oltipraz administration restored it (Fig. 3e).
Oltipraz reverses HFD-induced NRF2 repression and oxidative stress
To investigate the involvement of oxidative stress and the endogenous NRF2 system in the development of insulin resistance induced by HFD, we first measured plasma GSH:GSSG ratio, an index of redox status. As shown in Fig. 4a, HFD feeding reduced the GSH:GSSG ratio by approximately 27%, while oltipraz administration completely prevented the reduction. In adipose tissue, HFD feeding also significantly reduced the GSH:GSSG ratio, while oltipraz administration showed a partial, although not statistically significant reversal (Fig. 4b). To detect protein carboxylation (an indicator of protein oxidation) in adipose tissue, we used dinitrophenol antibody. As shown in Fig. 4c, the total protein oxidation level was elevated in HFD mice, while oltipraz administration clearly reduced protein oxidation.
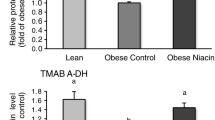
Oltipraz increases the plasma GSH:GSSG ratio and reverses HFD-induced NRF2 repression in adipose tissue. a Plasma and (b) fat cell GSH:GSSG ratio in the mice fed LFD, HFD and HFD + oltipraz (OPZ) diet at 28 weeks after diet initiation (n = 4 for all three groups, *p < 0.05). c Protein oxidation in epididymal fat tissue was detected using a protein oxidation detection kit, in which treated samples were subjected to SDS-PAGE and western blotting analysis with dinitrophenol (DNP) as the primary antibody, with β-actin as loading control. d Western blot assessment of NRF2 in nuclear preparations, quantified by optical density. Histone-3, a nuclear protein loading control. e SOD and HO-1 in whole-cell lysates. Samples were prepared from epididymal fat tissue of indicated group of mice. f Increased Keap1 mRNA expression by HFD feeding in adipose tissue and the reversal by oltipraz, detected by real-time RT-PCR (n = 4 for LFD and HFD, n = 3 for HFD + OPZ) as shown by regular RT-PCR image with 28 cycles (n = 2) and quantified in graph. Primers for Keap1 RT-PCR were Keap1 forward: 5-TGGTGTTCGCTTAGTGTTTC-3; Keap1 reverse: 5-CGCTTTCCAACCTCTTCACT-3. e, f *p < 0.05, **p < 0.01
We then tested whether endogenous NRF2 machinery in adipose tissue was impaired after HFD feeding. Both nuclear NRF2 levels and the levels of two known targets of NRF2, HO-1 and SOD, were chosen as indicators of the status of the NRF2 system. As shown in Fig. 4d, nuclear NRF2 levels in HFD mice were lower than in LFD mice, while oltipraz partially restored nuclear NRF2 content. Consistently, the levels of HO-1 and SOD were significantly reduced by HFD feeding, while oltipraz restored them (Fig. 4e). These changes were accompanied by increased KEAP1 production following HFD feeding and its reduction by oltipraz administration (Fig. 4f).
Oltipraz prevents HFD-induced inflammation and ER stress in adipose tissue
Oxidative stress affects other redox-sensitive signalling, such as inflammation and ER function. Increased inflammatory signalling and ER stress have been associated with the development of insulin resistance [11, 12, 29]. We did not see significant alterations in plasma TNFα content with HFD feeding or oltipraz administration (Table 1). In fat tissue, however, the content of IκB, a negative modulator of the inflammatory mediator nuclear factor kappa-B, was significantly reduced by HFD feeding and significantly increased by oltipraz administration (Fig. 5a). Furthermore, iNOS, the nitric oxide synthase isoform that is elevated in response to inflammation, was increased by HFD feeding, and this increase was prevented by oltipraz administration (Fig. 5b). This was associated with inhibition of macrophage infiltration by oltipraz administration, as detected by immunostaining using the F4/80 antibody (Fig. 5c). Finally, in adipose tissue, eIF2α Ser51, an indicator of ER stress, was activated by HFD feeding, while oltipraz partially attenuated this effect (Fig. 5d). Neither apparent changes in IκB content, nor alterations of the ER stress indicator eIF2α Ser51 were observed in the liver (data not shown).
Oltipraz prevents HFD-induced inflammation and ER stress in adipose tissue. Mice on LFD, HFD and HFD + oltipraz (OPZ) diets for 28 weeks were killed. Epididymal fat pads were taken for western blotting to assess levels of IκB (a), iNOS and endothelial nitric oxide synthase (eNOS) (b) and phosphorylated eIF2α (d). Quantification was by optical density. n = 4, *p < 0.05, **p < 0.01. c Immunostaining shows detection of macrophage infiltration marker F4/80 (arrows) in the fat tissue of HFD-fed mice, but not in tissue of mice on LFD or HFD + OPZ
Our observations collectively suggest that oltipraz regulates insulin signalling via stimulation of the endogenous NRF2 machinery. For the exploration of underlying mechanisms, extensive in vitro investigations will be needed. Up to this stage, we have conducted Nrf2 siRNA knockdown in a hepatocyte cell line, showing that reduced Nrf2 production led to impaired insulin signalling and attenuated response to oltipraz protection (ESM Fig. 5).
Discussion
Oltipraz, a prototype dithiolethione, has been found to have cancer chemopreventive activity in a promising clinical trial [20]. Oltipraz may enhance the binding activity of NRF2 to the antioxidant response element, hence increasing production of phase II enzyme genes [30, 31]. Although the beneficial effect of oltipraz on insulin action has been documented in recent studies in some mouse models of insulin resistance [32, 33], these investigators did not directly relate the insulin-sensitising effect of oltipraz to NRF2 activation. We found that in our HFD mouse model the alteration in oxidative homeostasis, along with impaired glucose disposal and insulin signalling, as well as the development of obesity, can be reversed by oltipraz administration. These observations support the notion that the function of NRF2 is important in preventing HFD-induced oxidative stress and associated impairment of insulin signalling. We show in this study that long-term HFD feeding led to a reduced nuclear content of NRF2 in adipose tissue, along with decreased levels of NRF2 target proteins. Oltipraz administration abrogated these changes. We therefore suggest that HFD can lead to a defect in the endogenous NRF2 antioxidant system, which plays a role in the impairment of insulin signalling and energy homeostasis.
A dedicated and robust homeostasis in redox status is important for maintaining sensitivity to insulin [34]. It has been suggested that physiological levels of ‘oxidants’ are required to maintain effective insulin signalling [35, 36]. Conversely, oxidative stress or toxic levels of ROS will impair insulin signalling [37–39]. Oxidative stress may serve as a signal of the nutritional excess that negatively regulates insulin action via activation of the inhibitory process, such as inflammatory signalling [11, 40] and adaptive mechanisms including ER stress [12, 41]. These alterations causally induce the development of insulin resistance. We show in this model that pharmacological administration of oltipraz not only reversed oxidative stress, but also improved insulin sensitivity in HFD-fed mice. These observations highlight the importance of the NRF2 antioxidant system in regulating redox balance and maintaining insulin sensitivity during long-term consumption of high-fat food.
Oltipraz administration may improve in vivo insulin signalling through multiple mechanisms. Combining the previous observations by others [25, 26, 30] and those in this study, we would summarise the beneficial effects of oltipraz as follows. First, the elevation of NRF2 target enzymes, such as SOD and HO-1, by oltipraz administration suggests that oltipraz exerts its beneficial effect via NRF2 activation. This is consistent with the notion that NRF2-stimulated SOD or HO-1 production improves insulin signalling and glucose uptake in a setting of insulin resistance [2, 10]. Second, in line with NRF2 activation, the redox-related processes inflammation and ER stress can also be inhibited by the oltipraz-mediated activation of NRF2. Third, extensive investigations by Kim and colleagues and others have shown that oltipraz exerts its effect in hepatocytes via AMPK activation following oltipraz administration [25, 26]. These investigators demonstrated that AMPK can be activated by oltipraz, leading to p70S6K inhibition. This attenuates a negative feedback of IRS-1, resulting in improved insulin signalling [25, 26]. We were unable to verify the observations by Kim and colleagues in our model in hepatocytes, because the impairment of insulin action in liver was relatively modest. However, we did observe the opposite effects of HFD and oltipraz on AMPK and p70S6K phosphorylation in adipose tissue (Fig. 3). Finally, we show here for the first time that oltipraz reduces KEAP1 production. While the mechanisms underlying KEAP1 production remain largely unknown, it can be functionally inactive due to its mutation in certain cancer patients [42].
In the chronic HFD-fed mouse model in the current study, the development of insulin resistance and obesity took a relatively long time. We believe this model mimics the natural development of insulin resistance and therefore represents a relevant animal model. In addition, these conditions facilitated the detection of early pathological alterations that lead to the development of impaired insulin action. In this model, the most apparent abnormalities, including reduced PKB phosphorylation in response to i.p. insulin, the signs of inflammatory activation and ER stress, were all observed in adipose tissue. This is consistent with the current notion that adipose tissue is the main organ to be affected by oxidative stress after HFD feeding [43–45]. However, the concomitant alterations in lipid profile were observed both in blood and other insulin-sensitive tissues, including liver and muscle. Again, oltipraz administration was shown to reduce lipid content in liver and muscle. This supports the notion that lipid accumulation is important for the development of insulin resistance [43]. The underlying mechanism by which oltipraz caused this improvement could be related to its protective effect on mitochondria, which promotes lipid utilisation [30]; this deserves further investigation.
The phosphatidylinositol 3 kinase/PKB signalling pathway has been a focus for assessing insulin sensitivity. We found that although our experimental animals showed whole-body insulin insensitivity, and increased intrahepatic and muscle triacylglycerol content by HFD feeding, PKB Ser473 phosphorylation in response to i.p. insulin injection in the muscles was not impaired. These observations support the theory that IRS1-independent defects may define major nodes of insulin insensitivity [2]. To identify such a defect in muscle, which is the main organ for glucose uptake, will be a challenge future work.
Another major finding of the current study is that long-term oltipraz administration rendered mice resistant to HFD-induced obesity. Given that a few studies have shown the inhibitory effect of NRF2 activation on adipocyte differentiation [46, 47], the beneficial effect of oltipraz on HFD-induced obesity may be due to the direct inhibition of adipocyte differentiation. However, this notion has been challenged by a recent in vivo Nrf2 knockout mouse study, showing that NRF2 is required for adipocyte differentiation [48]. NRF2 deficiency leads to decreased peroxisome proliferator-activated receptor γ production, along with a decrease in adipose tissue mass [48]. Further studies are required to explore this apparent discrepancy of the role of NRF2 in adipose tissue differentiation, revealed by genetic knockout vs pharmacological manipulation.
Together, our observations indicate the importance of the endogenous NRF2 antioxidant system in preventing development of insulin resistance and obesity. They also indicate the beneficial effects of oltipraz administration in HFD-fed animals. We suggest that the induction of NRF2-responsive antioxidant enzymes to reduce oxidative stress is a potential strategy to combat obesity and the associated insulin resistance.
Abbreviations
- AMPK:
-
AMP-activated protein kinase
- 4E-BP1:
-
Eukaryotic translation initiation factor 4E
- eIF2α:
-
Eukaryotic initiation factor 2 α
- ER:
-
Endoplasmic reticulum
- GSH:
-
Reduced glutathione
- GSSG:
-
Oxidised glutathione
- HFD:
-
High-fat diet
- HO-1:
-
Haem oxygenase-1
- iNOS:
-
Inducible nitric oxide synthase
- IPGTT:
-
Intraperitoneal glucose tolerance test
- IPITT:
-
Intraperitoneal insulin tolerance test
- IPPTT:
-
Intraperitoneal pyruvate tolerance test
- KEAP1:
-
Kelch-like ECH-associated protein 1
- LFD:
-
Low-fat diet
- MRI:
-
Magnetic resonance imaging
- mTOR:
-
Mammalian target of rapamycin
- NRF2:
-
Nuclear respiratory factor 2 alpha subunit
- PKB:
-
Protein kinase B
- ROS:
-
Reactive oxygen species
- siRNA:
-
Small interfering RNA
- S6K:
-
RPS6-p70-protein kinase
- SOD:
-
Superoxide dismutase
References
Reaven GM (1995) Pathophysiology of insulin resistance in human disease. Physiol Rev 75:473–486
Hoehn KL, Salmon AB, Hohnen-Behrens C et al (2009) Insulin resistance is a cellular antioxidant defense mechanism. Proc Natl Acad Sci U S A 106:17787–17792
Houstis N, Rosen ED, Lander ES (2006) Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature 440:944–948
Matsuzawa-Nagata N, Takamura T, Ando H et al (2008) Increased oxidative stress precedes the onset of high-fat diet-induced insulin resistance and obesity. Metabolism 57:1071–1077
Furukawa S, Fujita T, Shimabukuro M et al (2004) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114:1752–1761
Perreault M, Marette A (2001) Targeted disruption of inducible nitric oxide synthase protects against obesity-linked insulin resistance in muscle. Nat Med 7:1138–1143
Haber CA, Lam TK, Yu Z et al (2003) N-acetylcysteine and taurine prevent hyperglycemia-induced insulin resistance in vivo: possible role of oxidative stress. Am J Physiol Endocrinol Metab 285:E744–E753
Yasukawa T, Tokunaga E, Ota H et al (2005) S-nitrosylation-dependent inactivation of Akt/protein kinase B in insulin resistance. J Biol Chem 280:7511–7518
Kaneki M, Shimizu N, Yamada D, Chang K (2007) Nitrosative stress and pathogenesis of insulin resistance. Antioxid Redox Signal 9:319–329
D’Apolito M, Du X, Zong H et al (2010) Urea-induced ROS generation causes insulin resistance in mice with chronic renal failure. J Clin Invest 120:203–213
Yuan M, Konstantopoulos N, Lee J et al (2001) Reversal of obesity- and diet-induced insulin resistance with salicylates or targeted disruption of Ikkbeta. Science 293:1673–1677
Malhotra JD, Kaufman RJ (2007) Endoplasmic reticulum stress and oxidative stress: a vicious cycle or a double-edged sword? Antioxid Redox Signal 9:2277–2293
Bonnard C, Durand A, Peyrol S et al (2008) Mitochondrial dysfunction results from oxidative stress in the skeletal muscle of diet-induced insulin-resistant mice. J Clin Invest 118:789–800
Kaspar JW, Niture SK, Jaiswal AK (2009) Nrf2:INrf2 (Keap1) signaling in oxidative stress. Free Radic Biol Med 47:1304–1309
Sumi D, Numasawa Y, Endo A, Iwamoto N, Kumagai Y (2009) Catechol estrogens mediated activation of Nrf2 through covalent modification of its quinone metabolite to Keap1. J Toxicol Sci 34:627–635
Nicolai A, Li M, Kim DH et al (2009) Heme oxygenase-1 induction remodels adipose tissue and improves insulin sensitivity in obesity-induced diabetic rats. Hypertension 53:508–515
Ndisang JF, Lane N, Jadhav A (2009) Upregulation of the heme oxygenase system ameliorates postprandial and fasting hyperglycemia in type 2 diabetes. Am J Physiol Endocrinol Metab 296:E1029–E1041
Thirunavukkarasu V, Anuradha CV (2004) Influence of alpha-lipoic acid on lipid peroxidation and antioxidant defence system in blood of insulin-resistant rats. Diabetes Obes Metab 6:200–207
Curtis JM, Grimsrud PA, Wright WS et al (2010) Down regulation of adipose glutathione S-transferase leads to increased protein carbonylation, oxidative stress and mitochondrial dysfunction. Diabetes 59:1132–1142
Lee JS, Surh YJ (2005) Nrf2 as a novel molecular target for chemoprevention. Cancer Lett 224:171–184
Oakes ND, Thalen PG, Jacinto SM, Ljung B (2001) Thiazolidinediones increase plasma-adipose tissue FFA exchange capacity and enhance insulin-mediated control of systemic FFA availability. Diabetes 50:1158–1165
Carey MF, Peterson CL, Smale ST (2009) Dignam and Roeder nuclear extract preparation. Cold Spring Harb Protoc. doi:10.1101/pdb.prot5330
Shao W, Yu Z, Fantus IG, Jin T (2010) Cyclic AMP signaling stimulates proteasome degradation of thioredoxin interacting protein (TxNIP) in pancreatic beta-cells. Cell Signal 22:1240–1246
Sirek AS, Liu L, Naples M et al (2009) Insulin stimulates the expression of carbohydrate response element binding protein (ChREBP) by attenuating the repressive effect of Pit-1, Oct-1/Oct-2, and Unc-86 homeodomain protein octamer transcription factor-1. Endocrinology 150:3483–3492
Hwahng SH, Ki SH, Bae EJ, Kim HE, Kim SG (2009) Role of adenosine monophosphate-activated protein kinase-p70 ribosomal S6 kinase-1 pathway in repression of liver X receptor-alpha-dependent lipogenic gene induction and hepatic steatosis by a novel class of dithiolethiones. Hepatology 49:1913–1925
Tremblay F, Marette A (2001) Amino acid and insulin signaling via the mTOR/p70 S6 kinase pathway. A negative feedback mechanism leading to insulin resistance in skeletal muscle cells. J Biol Chem 276:38052–38060
Thomson DM, Fick CA, Gordon SE (2008) AMPK activation attenuates S6K1, 4E-BP1, and eEF2 signaling responses to high-frequency electrically stimulated skeletal muscle contractions. J Appl Physiol 104:625–632
Larance M, Ramm G, James DE (2008) The GLUT4 code. Mol Endocrinol 22:226–233
Hotamisligil GS (2010) Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Cell 140:900–917
Choi SH, Kim YM, Lee JM, Kim SG (2010) Antioxidant and mitochondrial protective effects of oxidized metabolites of oltipraz. Expert Opin Drug Metab Toxicol 6:213–224
Zhu H, Itoh K, Yamamoto M, Zweier JL, Li Y (2005) Role of Nrf2 signaling in regulation of antioxidants and phase 2 enzymes in cardiac fibroblasts: protection against reactive oxygen and nitrogen species-induced cell injury. FEBS Lett 579:3029–3036
Bae EJ, Yang YM, Kim JW, Kim SG (2007) Identification of a novel class of dithiolethiones that prevent hepatic insulin resistance via the adenosine monophosphate-activated protein kinase-p70 ribosomal S6 kinase-1 pathway. Hepatology 46:730–739
Brooks SC 3rd, Brooks JS, Lee WH, Lee MG, Kim SG (2009) Therapeutic potential of dithiolethiones for hepatic diseases. Pharmacol Ther 124:31–43
Bashan N, Kovsan J, Kachko I, Ovadia H, Rudich A (2009) Positive and negative regulation of insulin signaling by reactive oxygen and nitrogen species. Physiol Rev 89:27–71
Goldstein BJ, Mahadev K, Wu X (2005) Redox paradox: insulin action is facilitated by insulin-stimulated reactive oxygen species with multiple potential signaling targets. Diabetes 54:311–321
Loh K, Deng H, Fukushima A et al (2009) Reactive oxygen species enhance insulin sensitivity. Cell Metab 10:260–272
Ando K, Fujita T (2009) Metabolic syndrome and oxidative stress. Free Radic Biol Med 47:213–218
Nunn AV, Bell JD, Guy GW (2009) Lifestyle-induced metabolic inflexibility and accelerated ageing syndrome: insulin resistance, friend or foe? Nutr Metab Lond 6:16, Abstract
Gao L, Mann GE (2009) Vascular NAD(P)H oxidase activation in diabetes: a double-edged sword in redox signalling. Cardiovasc Res 82:9–20
Park J, Chung JJ, Kim JB (2007) New evaluations of redox regulating system in adipose tissue of obesity. Diabetes Res Clin Pract 77(Suppl 1):S11–S16
Santos CX, Tanaka LY, Wosniak J, Laurindo FR (2009) Mechanisms and implications of reactive oxygen species generation during the unfolded protein response: roles of endoplasmic reticulum oxidoreductases, mitochondrial electron transport, and NADPH oxidase. Antioxid Redox Signal 11:2409–2427
Singh A, Misra V, Thimmulappa RK et al (2006) Dysfunctional KEAP1-NRF2 interaction in non-small-cell lung cancer. PLoS Med 3:e420
Yu YH, Ginsberg HN (2005) Adipocyte signaling and lipid homeostasis: sequelae of insulin-resistant adipose tissue. Circ Res 96:1042–1052
Lumeng CN, Deyoung SM, Bodzin JL, Saltiel AR (2007) Increased inflammatory properties of adipose tissue macrophages recruited during diet-induced obesity. Diabetes 56:16–23
Andersson CX, Gustafson B, Hammarstedt A, Hedjazifar S, Smith U (2008) Inflamed adipose tissue, insulin resistance and vascular injury. Diabetes Metab Res Rev 24:595–603
Shin SM, Kim SG (2009) Inhibition of arachidonic acid and iron-induced mitochondrial dysfunction and apoptosis by oltipraz and novel 1, 2-dithiole-3-thione congeners. Mol Pharmacol 75:242–253
Shin S, Wakabayashi N, Misra V et al (2007) NRF2 modulates aryl hydrocarbon receptor signaling: influence on adipogenesis. Mol Cell Biol 27:7188–7197
Pi J, Leung L, Xue P et al (2010) Deficiency in the nuclear factor E2-related factor-2 transcription factor results in impaired adipogenesis and protects against diet-induced obesity. J Biol Chem 285:9292–9300
Acknowledgements
This study was supported by operating grants from Canadian Institutes of Health Research to T. Jin (89887) and I. G. Fantus (97979). W. Shao is a recipient of a Banting and Best Diabetes Centre/University Health Network Post-doctoral Fellowship (Diabetes Care).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Z. Yu and W. Shao contributed equally to this study.
An erratum to this article can be found at http://dx.doi.org/10.1007/s00125-011-2043-6
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Fig. 1
Liver weight and lipid content. a The weight of the liver and (b) the amount of triacylglycerol (TG) in liver from mice on LFD, HFD and HFD + oltipraz (OPZ) diets for 28 weeks was measured after mice were killed (n = 8 for each group). c MRI assessment of intra-hepatic lipid content (n = 4). d Representative MRI spectra, including in-phase water resonance and inlay of in-phase fat resonance for each experimental group. au, arbitrary units; ppm, parts per million (PDF 41 kb)
ESM Fig. 2
Lipid content in the gastrocnemius muscle. a The amount of triacylglycerol (TG) in the gastrocnemius muscle from mice on LFD, HFD and HFD + oltipraz (OPZ) diets for 28 weeks was measured after mice were killed (n = 8 for each group). b MRI assessment of lipid content in the gastrocnemius muscle of the three groups of mice after 26 weeks of diet (n = 4). c Representative MRI spectra, including in-phase water resonance and inlay of in-phase fat resonance for each experimental group. au, arbitrary units; ppm, parts per million (PDF 21.7 kb)
ESM Fig. 3
Representative images of haematoxylin and eosin staining on mouse liver sections. Liver samples were prepared from mice on (a) LFD, (b) HFD and (c) HFD + oltipraz (OPZ) for 28 weeks, or on HFD with 60% of energy from fat (d) for 8 weeks (PDF 104 kb)
ESM Fig. 4
PKB phosphorylation is not impaired in skeletal muscle of HFD mice. Mice on LFD, HFD and HFD + oltipraz (OPZ) diets for 28 weeks were fasted overnight and injected with PBS or insulin for 30 min. Samples from soleus muscle (a) and gastrocnemius muscle (b) were prepared for western blotting, with indicated antibodies. Representative blots are shown; n = 3 (PDF 47 kb)
ESM Fig. 5
Nrf2 knockdown impairs insulin signalling in HepG2 cells. a Oltipraz (OPZ) pretreatment prevents ROS-induced insulin resistance. HepG2 cells were incubated overnight in serum-free DMEM with indicated reagents, followed by addition of glucose oxidase (GO, 100 μU/ml) for 3 h. After washing with DMEM for 1 h, cells were treated with 100 nmol/l insulin (INS) for 15 min. Whole-cell lysates were then prepared for detection of PKB Ser473 or total PKB by western blotting, with densitometric analysis (n = 3). b Knockdown Nrf2 impairs insulin-stimulated PKB Ser473 phosphorylation. Top panel: 20 or 40 μmol/l Nrf2 siRNA effectively reduced Nrf2 expression in the HepG2 cell line. Bottom panel: after control scrambled siRNA transfection, insulin was still able to strongly stimulate PKB Ser473 phosphorylation. GO pretreatment impaired the effect of insulin, while oltipraz partially restored it. After Nrf2 knockdown, the effect of insulin on PKB Ser473 phosphorylation was severely impaired in the presence and absence of GO or oltipraz (PDF 194 kb)
ESM 1
(PDF 5 kb)
Rights and permissions
About this article
Cite this article
Yu, Z., Shao, W., Chiang, Y. et al. Oltipraz upregulates the nuclear respiratory factor 2 alpha subunit (NRF2) antioxidant system and prevents insulin resistance and obesity induced by a high-fat diet in C57BL/6J mice. Diabetologia 54, 922–934 (2011). https://doi.org/10.1007/s00125-010-2001-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-2001-8