Abstract
Aims/hypothesis
In 2003, guidelines for management of diabetic foot infection (DFI) were written by the authors’ team according to the guidelines of the International Working Group on the Diabetic Foot. The effects of implementing these guidelines on the microbiology and costs of infected diabetic foot ulcers were assessed.
Methods
From 2003 to 2007, potential beneficial effects of implementing these guidelines were assessed by comparison over time of bacteriological data (number of bacterial samples, number of microorganisms isolated in cultures, prevalence of multidrug-resistant organisms [MDRO] and colonising flora), and costs related to use of antimicrobial agents and microbiology laboratory workload.
Results
The study included 405 consecutive diabetic patients referred to the Diabetic Foot Unit for a suspected DFI. From 2003 to 2007, a significant decrease was observed in the median number of bacteria species per sample (from 4.1 to 1.6), prevalence of MDRO (35.2% vs 16.3%) and methicillin-resistant Staphylococcus aureus (52.2% vs 18.9%) (p < 0.001). Moreover, prevalence of pathogens considered as colonisers dramatically fell from 23.1% to 5.8% of all isolates (p < 0.001). In parallel, implementation of guidelines was associated with a saving of €14,914 (US$20,046) related to a reduced microbiology laboratory workload and €109,305 (US$147,536) due to reduced prescription of extended-spectrum antibiotic agents.
Conclusions/interpretation
Implementation of guidelines for obtaining specimens for culture from patients with DFI is cost-saving and provides interesting quality indicators in the global management of DFI.
Similar content being viewed by others
Introduction
Diagnosis and treatment of infected diabetic foot ulcers (DFU) remain problematic. As emphasised in recently published guidelines, diabetic foot infection (DFI) should be diagnosed on clinical arguments, but the cardinal manifestations of inflammation may be mitigated by diabetic complications, particularly neuropathy and ischaemia [1–3]. On the other hand, wound cultures may suggest, but do not prove, the presence of infection, as all open chronic wounds are covered by colonising flora. Appropriate antibiotic treatment requires antibiotic susceptibility testing to be performed on cultures from the wound, but the accuracy of bacteriological results depends, critically, not only on obtaining appropriate specimens but also on collecting them from the appropriate (clinically infected) patients. Unless strict criteria are implemented for diagnosis of DFI, overestimation of DFI may be of major concern, leading to misuse of antimicrobial agents with potential adverse effects and possible development of antibiotic resistance, as well as wasting money.
In 2003, a multidisciplinary group working on the diabetic foot (GP30) was set up in our University hospital, including specialists in diabetology, bacteriology, infectious diseases, vascular and orthopaedic surgery, imaging medicine and rehabilitation. One of the objectives of this group was to develop guidelines on how to diagnose and treat DFI.
The aim of the present study was to assess the effects of these guidelines on the microbiology and healthcare costs of DFU.
Methods
Guidelines for DFI
Following an internal audit in 2003, all specialists at our University hospital involved in the management of the diabetic foot attended regular multidisciplinary meetings in order to write guidelines for diagnosing and treating DFI. Our aim was to provide procedures to improve the selection of patients from whom cultures should be obtained and the techniques of collecting cultures, and to avoid contamination by the commensal flora that colonise the skin. These guidelines were based on the International Consensus on the Diabetic Foot and Practical Guidelines on the Management and the Prevention of the Diabetic Foot published in 1999 by the International Working Group on the Diabetic Foot [4], local practices and expert opinions. Briefly, the main points of our guidelines were as follows. (1) DFI must be diagnosed according to clinical signs and symptoms, and must always be confirmed and classified by an expert in the field (J.-L. Richard, N. Jourdan, S. Schuldiner). (2) Bacteriological sampling is only indicated if DFI is clinically confirmed, corresponding to a grade 2–4 infection using the International Consensus grading system [2]. (3) Before sampling, the wound must be mechanically debrided and cleansed using gauze soaked in sterile physiological saline. (4) Samples must be obtained by scraping or curetting the wound base, by aspirating purulent secretion using a needle, or by tissue biopsy. Superficial swabbing of the wound was discouraged, but swabbing the base of the ulcer (‘deep swab technique’) was allowed if it was the only possible option. For osteomyelitis, performing a bone biopsy by surgery, or percutaneously through healthy skin, was recommended [3]. (5) Sampling may be repeated only if the outcome is unfavourable. (6) Samples must be sent to the microbiology laboratory as rapidly as possible. (7) Only clinically infected DFU warrants antibiotic therapy [1–3, 5, 6]. All these guidelines have been widely circulated to all the staff of the departments involved in managing DFI. Effective communication between clinicians and bacteriology department staff was emphasised, as was a rapid processing of samples. Moreover, a specialist in infectious diseases was readily available to discuss antibiotic regimens for difficult-to-treat DFI.
Patients
This study was approved by the responsible ethics committee (South Mediterranean III) and was carried out in accordance with the Declaration of Helsinki as revised in 2000. All patients gave informed consent for participation in the study. From 1 January 2003 to 31 December 2007, all diabetic patients managed in the two diabetology departments of our University hospital with a suspected newly presenting episode of DFI were included in the study, provided at least one sample was taken for culture. Every wound was assessed for severity of infection by a trained diabetologist (J.-L. Richard, N. Jourdan, S. Schuldiner). Osteomyelitis was diagnosed by a positive probe-to-bone test and/or suggestive results of imaging studies (radionuclide scans or magnetic resonance imaging) [7]. The International Working Group on Diabetic Foot (IWGDF) criteria for diagnosing osteomyelitis [8] were not used as they were not available at the time of the study.
Microbiological methods
The Vitek 2 automated system (BioMérieux, Marcy l’Etoile, France) was used for biochemical identification of pathogens and for antibiotic susceptibility testing [9]. Strains were classified as antibiotic sensitive, intermediately resistant, or resistant, according to the recommendations of the Antibiotic Committee of the French Society for Microbiology [10]. Multidrug-resistant organisms (MDRO) included methicillin-resistant Staphylococcus aureus (MRSA), extended-spectrum cephalosporin (ESC)-resistant Enterobacteriaceae, Pseudomonas aeruginosa resistant to two antibiotics among piperacillin, ciprofloxacin, ceftazidime and imipenem, Enterococcus sp. resistant to glycopeptides, Acinetobacter baumannii resistant to ceftazidime, and Stenotrophomonas maltophilia [10]. Low-virulence bacteria included such well-described commensal flora as coagulase-negative Staphylococcus, Corynebacterium sp. and Propionibacterium sp., together with Enterococcus sp., Stenotrophomonas maltophilia, and Pseudomonas sp., whose virulence in DFIs remains a matter of debate.
Statistical and economic analysis
All statistical analyses were carried out using the SAS/ETS statistical package, version 9.1 (SAS Institute Inc., Cary, NC, USA). Yearly number of specimens, number of bacteria species per sample, distribution by bacterial species and MDRO prevalence were compared throughout the study period using Fisher’s exact test and χ 2 test. Results were considered significant at p < 0.05. For the healthcare economics analysis, the cost of microbiological cultures and the cost of the drugs (vancomycin and imipenem) prescribed by the medical doctors of the department were analysed. The cost for one bacteriological analysis of a diabetic foot sample was set at €31.81, according to the French General Nomenclature of Professional Acts (including inoculation of culture media, identification of pathogens, and antibiotic susceptibility testing) [11]. The prescription costs for the extended-spectrum antimicrobial agents were obtained from the hospital pharmacy. We used the fee negotiated by the hospital pharmacy. The daily cost of vancomycin (for treatment of MRSA) and imipenem (for treatment of ESC-resistant Enterobacteriaceae) was €5.68 and €52.24, respectively. Consumption of antibiotics during the study period was obtained from the hospital pharmacy database, and was expressed as defined daily doses (DDD) in grams per 1,000 patient-days [12]. The total cost to the hospital was assessed for each year. The mean cost per patient is also presented. The reduction in costs for each year was determined as the difference between the costs for that year and the costs for 2003. As the data obtained were aggregated, no statistical test was performed.
Results
Microbiological results
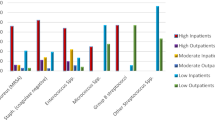
From 2003 to 2007, 405 consecutive patients (median age 70.3 years, range 32–97 years) were included in the study, as both outpatients (n = 332) and inpatients (n = 73). Their clinical characteristics are given in Table 1. Using the IWGDF–Infectious Diseases Society of America (IDSA) classification system, most wounds (56.5%) were classified as grade 2 (mild infection), but it was not possible to confirm that all ulcers diagnosed in 2003 as grade 2 were really clinically infected. One hundred and twenty-three cases of osteomyelitis were diagnosed, corresponding to a prevalence rate of 30.4%. From 2004 to 2007, the distribution between infection grades remained roughly the same.
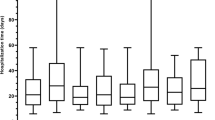
During the study period, 1,146 bacteriological samples were obtained, 76.4% by swab technique. However, from 2004 onwards, only the deep swab technique, including sharp wound debridement and curettage, was used (Table 1). Moreover, during this period, the other techniques were more frequently performed (17.6% in 2003 vs 36.2% in 2007) (p = 0.005). The yearly number of samples almost halved, from 323 in 2003 to 163 in 2007, and the number of samples per patient decreased significantly, from 3.5 to 2.1 (p < 0.001) (Table 2). The average number of isolates was 2.7 per sample, but there was a statistically significant decrease over time from 4.1 in 2003 to 2.1, 1.6 and 1.9 in 2005, 2006 and 2007, respectively (p < 0.001) (Table 2).
Gram-positive aerobic bacteria were the most frequently recovered pathogens, accounting for 59% of all isolates, with an increasing prevalence during the time period, from 55.6% in 2003 to 71.2% in 2007. The predominant aerobic species was S. aureus, comprising 24% of all aerobic strains. Gram-negative aerobes were isolated from 34.8% of cultures, with a decreasing prevalence rate from 38.8% of all isolates in 2003 to 22.4% in 2007. Among them, Enterobacteriaceae were the most frequent pathogens (22.7% of all isolates), including especially Escherichia coli (28.8% of Gram-negative bacteria) and Proteus mirabilis (27.6% of Gram-negative bacteria). Interestingly, P. aeruginosa was present in 8% of all isolates, but a non-significant downward trend was noted, from 12.8% in 2003 to 5.6% in 2007. Anaerobes accounted for fewer than 5% of all isolates, with no significant change over time.
MDRO were recovered from 29.8% of specimens, most of them being MRSA (37.7% of all MDRO). From 2003 to 2007, the percentage of MDRO significantly decreased from 35.2% to 16.3% of all isolates, with a decrease from 52.2% to 18.9% for MRSA and from 45.8% to 31.1% for ESC-resistant Enterobacteriaceae (p < 0.001) (Table 2). The percentage of patients with a MDRO-positive sample fell from 45.7% in 2003 to 23.4% in 2007 (p < 0.001).
The number of low-virulence bacteria fell dramatically, from 40.1% in 2003 to 16.4% of all isolates in 2007 (p < 0.001) (Table 2). Coagulase-negative Staphylococcus accounted for 15% of these isolates, with a significantly decreased prevalence rate in 2007 (5.8%) compared with 23.1% in 2003 (p < 0.001).
The distribution of bacteria isolated from bone biopsy was similar to that from other samples, with a predominance (60%) of Gram-positive aerobic bacteria. S. aureus was the most frequently isolated bacterium (25.3%), and coagulase-negative Staphylococci were the second most frequently cultured organisms, comprising 22.9% of all strains. Enterobacteriaceae and P. aeruginosa accounted for 19.4% and 9.4% of all isolates, respectively. No significant change in the distribution of organisms was noted between 2003 and 2007. The only significant difference was in the average number of isolates obtained by bone biopsy, which decreased over time from 3.2 in 2003 to 0.9 in 2007 (p < 0.001).
Effect on microbiology laboratory and drug costs
The number of samples decreased yearly, not only because the number of patients sampled decreased but also because the mean number of samples per patient decreased, leading to a decreasing mean cost per patient (Table 3). The resulting cost saving (compared with 2003) ranged from €1,940 in 2004 to €5,088 in 2007. The trend was similar for vancomycin: the number of doses per patient decreased (Table 3), resulting in a cost saving ranging from €1,070 in 2004 to €3,661 in 2007. The most important saving observed was for imipenem: from €6,926 in 2004 to €49,123 in 2007. This saving is explained by a decreased number of doses per patient (reduced about fivefold between 2003 and 2007). Finally, the total saving reached €57,872 (US$76,644) in 2007 (Table 3). This represented a 76.4% decrease in costs to the hospital. In total, a cost saving of €14,914 (US$20,046) related to the reduced microbiology laboratory workload was observed. Moreover, a cost saving of €9,379 (US$12,678) for MRSA and €99,926 (US$135,044) for Enterobacteriaceae was also achieved, due to decreased prescription of extended-spectrum antibiotic agents.
Discussion
Infection is a common and costly complication of foot ulcers in diabetic individuals and represents a major cause of morbidity and mortality [13]. The results of this study highlighted for the first time the beneficial effect of implementing guidelines on DFI in terms of microbiology and health economics.
In 2003, an internal audit on patients referred in our department for suspected DFI showed that too many samples were being taken, with frequent polymicrobial cultures and a high rate of commensal bacteria, making management of these wounds difficult. Moreover, prevalence of MDRO (especially S. aureus) was high. These results suggested that clinically non-infected ulcers were possibly being sampled, the quality of sampling techniques was far from optimal, and several steps in the pre-analytical stage were problematic. Following this, our local multidisciplinary group established guidelines on DFI based on IWGDF and IDSA recommendations [2, 4], as previously mentioned. From 2004 onwards, audits were conducted yearly to analyse trends in microbiological data.
Overall, our bacteriological results were in accordance with other studies showing that S. aureus is the most frequently isolated microorganism from infected DFU, with a rather high prevalence rate of MDRO [14, 15]. However, our study clearly showed that implementation of guidelines was associated with a decrease in number of samples, possibly due to optimal selection of patients suffering from DFI, as from 2004 onwards all cases of DFI were clinically diagnosed by an expert. This is supported by the fact that the number of patients with suspected DFI did not change significantly during the study period (data not shown). The decrease in number of samples per patient is probably related to a decrease in repeated sampling in any given patient, as indicated in the guidelines. The main results of this study were the quantitative and qualitative microbiological changes we recorded after implementation of the guidelines: the decrease in number of pathogens per sample, from 4.1 to 1.9, was striking; in parallel, the recovery rate of Gram-negative bacilli decreased steadily, mirroring the increased rate of Gram-positive cocci. Moreover, the prevalence rate of MDRO dramatically and steadily decreased, halving from 2003 to 2007; the most important decrease was for MRSA, whose prevalence was reduced almost threefold. The prevalence rate of bacteria considered as low-virulence pathogens or commensal flora was halved, from 40.1 to 16.4%. These changes are probably related to better sampling methods, as, according to the guidelines, we progressively modified our sampling technique, using deep tissue sampling instead of superficial swabbing (obtained by rolling a cotton swab across the surface of the wound). If the best sampling technique remains a matter of debate, most, though not all, experts [7, 16, 17] favour deep tissue specimens over superficial swabs, and these methods are recommended in many guidelines [1–4, 18]. Moreover changing our sampling technique probably contributed to the removal of colonising bacteria, notably MDRO, that we noticed in this study. As previously shown, these colonising S. aureus strains (especially MRSA) have a rather low virulence potential [19] and no significant impact on wound healing [20]. While we modified our sampling techniques, used adapted anaerobic transport tubes, promoted a rapid transport of samples and set up a more appropriate technique for bacterial isolation, the recovery rate of anaerobes remained low compared with the percentage usually reported in the literature [16]. This could be explained by the fact that the majority of our patients suffered from grade 2 DFI and by a particular microbiological profile in our diabetic foot clinic. As the prevalence of MRSA in DFI is reported to be emerging as a serious problem [15, 21], our results are rather encouraging. Nevertheless, we cannot attribute those changes only to the implementation of guidelines. Indeed, the French National Observatory for Epidemiology of Bacterial Resistance to Antimicrobials and the European Antimicrobial Resistance Surveillance System reported a decrease in the prevalence of MRSA in France [22, 23], and MRSA strains responsible for bacteraemia decreased from 33% in 2001 to 26% in 2007. This trend could be explained by a change in the major epidemic clone of MRSA detected in French hospitals (replacing the Iberic clone with the pandemic clone V) [24, 25]. Moreover, we cannot exclude a possible effect of national campaigns promoted by the French health authorities on a more sound use of antibiotic agents (1999) and on the usefulness of hydro-alcoholic solution for handwashing (2001–2002) [26], as these measures have been associated with a reduction in MRSA development and transmission [27, 28].
From the point of view of health economics, the cost saving for our hospital was estimated to be at least €110,000 (∼US$150,000), mainly due to decreased prescription of extended-spectrum antibiotics (in line with a decrease in DDD for those antibiotics) as a consequence of the reduction in MDRO prevalence. The discrepancy between the dramatic decrease in MRSA and the less marked decrease in DDD for vancomycin is best explained by our high suspicion of MRSA-related infections: empirical therapy using vancomycin was frequently started before the results of culture and sensitivity testing were known, particularly for Grade 4 DFI. Our cost-saving evaluation remained a conservative figure, as it was not possible to estimate the amount of money saved by avoiding the use of antibiotic agents in uninfected ulcers.
A main limitation of our study was the difficulty of assessing the specific impact of modifying our sampling techniques on patients’ outcome, because after 2004 not only those techniques, but also the whole management of patients suffering from DFU, were changed. Our diabetic foot clinic was radically reorganised, promoting a multidisciplinary strategy by a team made up of trained diabetologists, microbiologists and specialists in infectious diseases, radiologists, orthopaedic and vascular surgeons, physiotherapists, podiatrists and dedicated nurses, with regular meetings and readily available advice. Thus our improved microbiological data must be interpreted as a quality indicator in the global management of DFI. The decrease in amputation rate was also an indirect marker of the beneficial impact of the multidisciplinary approach and the efficacy of the guidelines.
In conclusion, this study demonstrated that implementation of evidence-based guidelines on DFI enabled us to reduce the number of pathogens per sample, and especially the prevalence of both MDRO and commensal flora, leading to an important saving of money for our hospital. A consensus involving all health professionals involved in diabetic foot problems, and an effective cooperation between them, are central for success.
Abbreviations
- DDD:
-
Defined daily doses
- DFI:
-
Diabetic foot infection
- DFU:
-
Diabetic foot ulceration
- ESC:
-
Extended-spectrum cephalosporin
- IDSA:
-
Infectious Diseases Society of America
- IWGDF:
-
International Working Group on Diabetic Foot
- MDRO:
-
Multidrug-resistant organism
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
References
American Diabetes Association (1999) Consensus development conference on diabetic foot wound care. Diab Care 22:1354–1360
American Diabetes Association (2004) Nephropathy in diabetes. Diab Care 27:579–583
L’Assurance Maladie (2010) French nomenclature of medical biology acts. Available from www.ameli.fr/professionnels-de-sante/medecins/exercer-au-quotidien/nomenclatures-et-codage, accessed 4 February 2010
Barry J, Brown A, Ensor V et al (2003) Comparative evaluation of the VITEK 2 Advanced Expert System (AES) in five UK hospitals. J Antimicrob Chemother 51:1191–1202
Berendt AR, Peters EJG, Bakker K et al (2008) Diabetic foot osteomyelitis: a progress report on diagnosis and a systematic review of treatment. Diabetes Metab Res Rev 24:S145–S161
Carlet J, Astagneau P, Brun-Buisson C et al (2009) French national program for prevention of healthcare-associated infections and antimicrobial resistance, 1992–2008: positive trends, but perseverance needed. Infect Control Hosp Epidemiol 30:737–745
Chantelau E, Tanudjaja T, Altenhofer F, Ersanli Z, Lacigova S, Metzger C (1996) Antibiotic treatment for uncomplicated neuropathic forefoot ulcers in diabetes: a controlled trial. Diabet Med 13:156–159
Citron DM, Goldstein EJC, Merriam CV, Lipsky BA, Abramson MA (2007) Bacteriology of moderate-to-severe diabetic foot infections and in vitro activity of antimicrobial agents. J Clin Microbiol 45:2819–2828
Dang CN, Prasad YDM, Boulton AJ, Jude EB (2003) Methicillin-resistant Staphylococcus aureus in the diabetic foot clinic: a worsening problem. Diabet Med 20:159–161
European Antimicrobial Resistance Surveillance System (EARSS), Antibiotic Susceptibility Testing (2010). The European Antimicrobial Resistance Surveillance System. Available from www.rivm.nl/earss, accessed 4 February 2010
French National Observatory for Epidemiology of Bacterial Resistance to Antimicrobials (2010) Onerba. Available from www.onerba.org, accessed 4 February 2010
International Working Group on the Diabetic Foot, International Consensus on the diabetic foot (1999) International Working Group on the Diabetic Foot. Available from www.iwgdf.org, accessed 4 February 2010
Jeffcoate WJ, Lipsky BA, Berendt AR et al (2008) Unresolved issues in the management of ulcers of the foot in diabetes. Diabet Med 25:1380–1389
Leclercq R (2009) Epidemiological and resistance issues in multidrug-resistant staphylococci and enterococci. Clin Microbiol Infect 15:224–231
Lelievre H, Lina G, Jones ME et al (1999) Emergence and spread in French hospitals of methicillin-resistant Staphylococcus aureus with increasing susceptibility to gentamicin and other antibiotics. J Clin Microbiol 37:3452–3457
Lipsky BA (1997) Osteomyelitis of the foot in diabetic patients. Clin Infect Dis 25:1318–1326
Lipsky BA (2004) International consensus group on diagnosing and treating the infected diabetic foot: a report from the international consensus on diagnosing and treating the infected diabetic foot. Diabetes Metab Res Rev 20:S68–S77
Lipsky BA, Berendt AR, Deery HG et al (2004) Diagnosis and treatment of diabetic foot infections. Clin Infect Dis 39:885–910
Lipsky BA, Stoutenburgh U (2005) Daptomycin for treating infected diabetic foot ulcers: evidence from a randomized, controlled trial comparing daptomycin with vancomycin or semi-synthetic penicillins for complicated skin and skin-structure infections. J Antimicrob Chemother 55:240–245
Monnet DL, Molstad S, Cars O (2004) Defined daily doses of antimicrobials reflect antimicrobial prescriptions in ambulatory care. J Antimicrob Chemother 53:1109–1111
Pittet D, Hugonnet S, Harbarth S et al (2000) Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet 356:1307–1312
Prompers L, Huijberts M, Schaper N et al (2008) Resource utilisation and costs associated with the treatment of diabetic foot ulcers. Prospective data from the Eurodiale study. Diabetologia 51:1826–1834
Rao GG (1998) Risk factors for the spread of antibiotic-resistant bacteria. Drugs 55:323–330
Richard JL, Sotto A, Jourdan N et al (2008) Risk factors for and impact on healing of multidrug-resistant bacteria in diabetic foot ulcers. Diab Metab 34:363–369
Slater RA, Lazarovitch T, Boldur I et al (2004) Swab cultures accurately identify pathogens in diabetic foot wounds not involving bone. Diabet Med 21:705–709
Société de Pathologie Infectieuse de Langue Française (2007) Management of diabetic foot infections. Méd Mal Infect 37:1–25
Sotto A, Lina G, Richard JL et al (2008) Virulence potential of Staphylococcus aureus strains isolated from diabetic foot ulcers: a new paradigm. Diab Care 31:2318–2324
Soussy CJ, Carret G, Cavallo JD and the Antibiotic Susceptibility Testing Committee of the French Society for Microbiology, Antibiotic Susceptibility Testing (2010) French Society for Microbiology. Available from www.sfm.asso.fr, accessed 4 February 2010
Tentolouris N, Petrokkos G, Vallianou N et al (2006) Prevalence of methicillin-resistant Staphylococcus aureus in infected and uninfected diabetic foot ulcers. Clin Microbiol Infect 12:186–189
Acknowledgements
This work was supported by the French Speaking Association for Diabetes and Metabolic Diseases (ALFEDIAM grant), the University of Montpellier 1, the Languedoc-Roussillon area (Chercheur d’avenir grant) and the city of Nîmes. Part of this study was presented at the 8th scientific meeting of the Diabetic Foot Study Group of the European Association for the Study of Diabetes, Bled, Slovenia, September 2009.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sotto, A., Richard, JL., Combescure, C. et al. Beneficial effects of implementing guidelines on microbiology and costs of infected diabetic foot ulcers. Diabetologia 53, 2249–2255 (2010). https://doi.org/10.1007/s00125-010-1828-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-1828-3