Abstract
Aims/hypothesis
The fetal insulin hypothesis suggests that variation in the fetal genotype influencing insulin secretion or action may predispose to low birthweight and type 2 diabetes. We examined associations between 25 confirmed type 2 diabetes risk variants and birthweight in individuals from the Danish Inter99 population and in meta-analyses including Inter99 data and reported studies.
Methods
Midwife records from the Danish State Archives provided information on mother’s age and parity, as well as birthweight, length at birth and prematurity of the newborn in 4,744 individuals of the population-based Inter99 study. We genotyped 25 risk alleles showing genome-wide associations with type 2 diabetes.
Results
Birthweight was inversely associated with the type 2 diabetes risk alleles of ADCY5 rs11708067 (β = −33 g [95% CI −55, −10], p = 0.004) and CDKAL1 rs7756992 (β = −22 g [95% CI −43, −1], p = 0.04). The association for the latter locus was confirmed in a meta-analysis (n = 24,885) (β = −20 g [95% CI −29, −11], p = 5 × 10−6). The HHEX-IDE rs1111875 variant showed no significant association among Danes (p = 0.09); however, in a meta-analysis (n = 25,164) this type 2 diabetes risk allele was associated with lower birthweight (β = −16 g [95% CI −24, −8], p = 8 × 10−5). On average, individuals with high genetic risk (≥25 type 2 diabetes risk alleles) weighed marginally less at birth than those with low genetic risk (<25 type 2 diabetes risk alleles) (β = −35 g [95% CI −69, −2], p = 0.037).
Conclusions/interpretation
We report a novel association between the fetal ADCY5 type 2 diabetes risk allele and decreased birthweight, and confirm in meta-analyses associations between decreased birthweight and the type 2 diabetes risk alleles of HHEX-IDE and CDKAL1. No strong general effect on birthweight can be ascribed to the 25 common type 2 diabetes risk alleles.
Similar content being viewed by others
Introduction
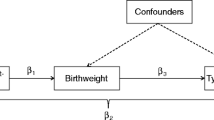
Previous studies have found that reduced birthweight is associated with impaired glucose tolerance and type 2 diabetes later in life [1, 2]. A recent meta-analysis of 14 studies demonstrated that the odds ratio of developing type 2 diabetes in adulthood is 1.47 for individuals born with low birthweight [3]. However, the aetiopathogenic mechanisms behind this association are far from elucidated. Twin studies have indicated a non-genetic origin of the association between birthweight and type 2 diabetes [4], and the ‘thrifty phenotype hypothesis’ suggests that poor nutritional conditions during critical periods of fetal life alter beta cell function and/or insulin action, thereby predisposing to type 2 diabetes in later life [2]. Insulin is important for fetal growth and for metabolism throughout life. The ‘fetal insulin hypothesis’ states that variation in the fetal genotype affecting pancreatic beta cell function or insulin sensitivity and thereby availability of insulin as a fetal growth factor predisposes to reduced birth size and risk of type 2 diabetes in later life [5]. This hypothesis is supported by the finding that newborns with mutations in GCK, KCNJ11, HNF1B and INS have marked insulin deficiency and considerably reduced birthweight [6–9]. In contrast, newborns with mutations in HNF4A, which also cause adult insulin deficiency and monogenic diabetes, have a higher birthweight due to elevated insulin secretion by the fetus [10], demonstrating that fetal and adult insulin secretion are not always correlated.
Maternal blood glucose level during pregnancy is a main determinant of fetal insulin secretion and thus fetal growth. Maternal hyperglycaemia may lead to fetal hyperinsulinaemia and consequently macrosomia is a well-known complication of untreated gestational diabetes. The maternal genotype may thereby influence fetal exposure to maternal glucose and thus interact with the effect of fetal genotype on fetal growth and subsequent birthweight of the newborn [6].
A total of 25 confirmed type 2 diabetes risk gene variants have been reported [11–31]. Of these, variants in or near NOTCH2, THADA, PPARG, ADAMTS9, IGF2BP2, CDKAL1, JAZF1, SLC30A8, CDKN2A/B, CDC123, HHEX-IDE, TCF7L2, KCNQ1, KCNJ11, MTNR1B, TSPAN8, GCK and FTO have previously been investigated in relation to birthweight [32–36]. However, only type 2 diabetes risk variants near HHEX-IDE and CDKAL1 have been associated with lower birthweight [32–34]. Zhao et al. found a highly significant effect of CDKAL1 rs7756992, but no significant association for the HHEX-IDE variant [34]. This is in contradiction with a Finnish cohort study, in which only an association for the HHEX-IDE locus was observed [33]; however, another CDKAL1 variant (rs7754840) was investigated in the latter study. Type 2 diabetes risk variants near TCF7L2 and CDKN2A/B have been associated with increased birthweight [33, 36].
Complete consistency among previous studies has not been achieved. Moreover, to our knowledge, five newly identified type 2 diabetes risk variants [13] have not been investigated in relation to fetal growth. The overall aim of this study was therefore to investigate the association between the 25 confirmed type 2 diabetes risk variants and birthweight in 4,213 individuals from the Danish Inter99 population (ClinicalTrials.gov NCT00289237) [37]. We also examined associations between type 2 diabetes risk variants and birthweight in meta-analyses including our own data and published studies.
Methods
Study population
Individuals examined in the present study were from the Danish Inter99 Study, which at baseline comprised 6,784 individuals living in the region of Copenhagen. The Inter99 is a population-based randomised non-pharmacological intervention study of prevention of ischaemic heart disease conducted at the Research Centre for Prevention and Health in Glostrup, Denmark (www.inter99.dk) [37, 38]. For 4,744 participants, midwife journals were traced through the Danish State Archives. These journals contained information on mothers’ age, parity and marital status as well as birthweight, length at birth and prematurity of the newborn. Ponderal index was calculated as birthweight (kg)/birth length (m3). Information about mothers’ diabetes status was obtained by a questionnaire during the baseline visits in 1999 to 2001. The age of onset of maternal diabetes was not registered.
Pregnancies were considered at term when gestation attained 36 complete weeks and did not exceed 41 complete weeks. Pre-term singleton deliveries (n = 446) and individuals born from multiple pregnancies (n = 85) were excluded, since these newborns are lighter presumably due to non-genetic factors. The final number of individuals included in the study was 4,213. All individuals were Danes by self-report. All participants gave written informed consent and the protocol was in accordance with the Helsinki Declaration and approved by local ethic committees.
Genotyping
Genotyping was performed using a genotyping device (KASPar; KBioscience, Hoddesdon, UK). All genotyping success rates were >96% with an error rate of <0.5%, except ADAMTS9 rs4607103, for which the error rate was 0.9%. All genotypes obeyed Hardy–Weinberg equilibrium in the Danish population (p > 0.05) except HHEX-IDE rs1111875 (p = 0.03), TCF7L2 rs7903146 (p = 0.02), DGKB/TMEM195 rs2191349 (p = 0.01) and SLC30A8 rs13266634 (p = 0.009).
Statistical analysis
All statistical analyses were performed using RGui version 2.8.1 (available at http://www.r-project.org). The effect of the genetic variants on birthweight, length at birth and ponderal index in the Inter99 population was calculated using linear regression models adjusted for sex, maternal diabetes (yes vs no/not available) and parity (0, 1, 2, 3 or ≥4). No transformation of data was performed. Only additive genetic models were considered assuming a constant change in birthweight per risk allele, with p < 0.05 being considered significant.
Statistical power was estimated using 1,000 simulations. We used the empirical variance of the observed traits adjusted for sex, maternal diabetes and parity to simulate phenotypes from a normal distribution, so that variance across genotypes is drawn from the estimated variance. In the Danish Inter99 study, we had more than 80% statistical power to detect effects of 45 g, 35 g and 30 g, assuming minor allele frequencies of 10%, 20% and 40%, respectively.
Fixed-effect meta-analyses (up to n = 25,957) were performed using effect size estimates and standard errors derived from linear regression analyses from this and three other studies [32, 33, 36]. Weight of studies in the meta-analyses was estimated using inverse variance assuming fixed effects. Heterogeneity was measured by Q-statistics.
A combined analysis of variants within CDKAL1, HHEX-IDE and ADCY5 loci was performed by summing up risk alleles of the three variants, where individuals can have from zero to six risk alleles.
Information from the 25 type 2 diabetes risk variants in 2,733 individuals with available genotype data on all 25 variants was combined into a binary risk allele score (low vs high genetic risk). In this population, the median number of risk alleles was 25. The combined effect was calculated by comparing two groups according to their number of risk alleles (low genetic risk, i.e. <25 type 2 diabetes risk alleles, n = 1,366 vs high genetic risk, i.e. ≥25 type 2 diabetes risk alleles, n = 1,367). In the combined analyses similar (fixed) effects of the variants were assumed.
Results
Quantitative analyses of birthweight in the Danish Inter99 population
Characteristics of the Inter99 participants are shown in Electronic supplementary material [ESM] Table 1. The 25 confirmed type 2 diabetes risk variants were investigated for an association with birthweight in 4,213 individuals from the Danish Inter99 population and the results of the quantitative analyses are shown in Table 1. The risk allele of rs11708067 at the ADCY5 locus was associated with a reduction in birthweight (per allele β = −33 g [95% CI −55, −10], p = 0.004) (Table 1). Also carriers of the CDKAL1 rs7756992 risk allele had lower birthweight (per allele β = −22 g [95% CI −43, −1], p = 0.04) (Table 1). The risk allele of rs1111875 near HHEX-IDE showed a tendency towards lower birthweight (per allele β = −17 g [95% CI −36, 2], p = 0.09) (Table 1). ADCY5 rs11708067 was also associated with a slightly decreased ponderal index (per allele β = −0.1 kg/m3 [95% CI −0.2, −0.02], p = 0.02) (Table 2), while CDKAL1 rs7756992 was associated with reduced birth length (−0.1 cm [95% CI −0.2, −0.01], p = 0.04) (Table 2). The risk allele of WFS rs10010131 showed a trend towards higher birthweight (per allele β = 19 g [95% CI −1, 39], p = 0.06) (Table 1). In the Inter99 study population, none of the associations remained significant after correction for multiple testing.
Meta-analyses
Meta-analyses including previously published data on type 2 diabetes loci in relation to birthweight were performed for CDKAL1 (n = 24,885), HHEX-IDE (n = 25,164), TCF7L2 (n = 19,745), SLC30A8 (n = 24,908), IGF2BP2 (n = 24,393), CDKN2A/B (n = 25,957), PPARG (n = 6,206), KCNJ11 (n = 6,206) and JAZF1 (n = 6,206) [32, 33, 36]. No data were available for the remaining variants.
In the meta-analysis of CDKAL1, three different proxies in linkage disequilibrium (HapMap Centre d'Etude du Polymorphisme [Utah residents with northern and western European ancestry] [CEU] r > 0.67) were used (rs7756992, rs10946398 and rs7754840). Type 2 diabetes risk variants within the CDKAL1 locus were associated with reduced birthweight in a fixed-effect meta-analysis (per allele β = −20 g [95% CI −29, −11], p = 5 × 10−6) (Fig. 1). Likewise, the HHEX-IDE rs1111875 type 2 diabetes risk allele was associated with reduced birthweight (per allele β = −16 g [95% CI −24, −8], p = 8 × 10−5) (Fig. 2).
Meta-analysis of HHEX-IDE rs1111875 fetal genotype and birthweight including up to 25,164 European individuals. Effect size estimates and standard errors obtained from previous published studies [32, 33] and the present study were combined in a meta-analysis using the inverse variance method. Black diamond, combined change in birthweight per fetal risk allele (β = −16 g [95% CI −24, −8], p = 8 × 10−5); black squares, effects in single studies sized according to their weight in the meta-analysis
Meta-analysis of CDKAL1 fetal genotype and birthweight including 24,885 European individuals. Effect size estimates and standard errors obtained from previous published studies [32, 33] and the present study were combined in a meta-analysis using the inverse variance method. Three different proxies rs7756992 (present study), rs7754840 [33] and rs10946398 [32] in linkage disequilibrium (HapMap CEU r > 0.67) were used. Black diamond, combined change in birthweight per fetal risk allele (β = −20 g [95% CI −29, −11], p = 5 × 10−6); black squares, effects in single studies sized according to their weight in the meta-analysis
No other published type 2 diabetes variants were associated with reduced birthweight in our meta-analyses (ESM Fig. 1). However, fetal TCF7L2 rs7903146 and CDKN2A/B rs10811661 type 2 diabetes risk alleles were associated with slightly increased birthweight (ESM Fig. 1a, f). No heterogeneity was observed in any of the meta-analyses (p > 0.2).
Combined effect of HHEX-IDE, CDKAL1 and ADCY5 type 2 diabetes risk alleles on birthweight
Information from the CDKAL1, HHEX-IDE and ADCY5 variants in the Danish population was combined into a fetal risk allele score (0–6 risk alleles) and the association with birthweight was tested. This analysis showed an average birthweight difference of −22 g [95% CI −34, −10], p = 0.0003 per risk allele (Fig. 3). The 14% of the examined Inter99 population carrying five to six risk alleles weighed on average 110 g [95% CI 42, 179] less than the 6% carrying zero to one risk alleles. In combined analyses, the three variants were also associated with modest decreases in birth length and ponderal index (per allele: β = −0.07 cm [95% CI −0.12, −0.01], p = 0.01 and β = −0.07 kg/m3 [95% CI −0.13, 0.00], p = 0.04, respectively).
The association between birthweight and the number of fetal type 2 diabetes risk alleles at CDKAL1 (rs7756992), HHEX-IDE (rs1111875) and ADCY5 (rs11708067) in the Danish Inter99 population (n = 4,213). Raw birthweight data (mean, SD) were plotted according to the number of risk alleles. Analyses were performed by summing up risk alleles assuming an additive genetic model adjusted for sex, maternal diabetes status and parity. Effect per allele: β = −22 g (95% CI −34, −10), p = 3 × 10−4
Combined analyses of effect of 25 type 2 diabetes risk alleles on birthweight
To estimate the effect of carrying a high vs low load of risk alleles, a combined analysis of all 25 variants was performed. Information from the 25 type 2 diabetes risk variants was combined into a binary risk allele score (low vs high genetic risk) and plotted against birthweight (Fig. 4). The association with birthweight was tested. Individuals with a high risk allele score (≥25 type 2 diabetes risk alleles) were on average slightly lighter than individuals with a low risk allele score (<25 type 2 diabetes risk alleles) (β = −35 g [95% CI −69, −2], p = 0.037). A similar analysis excluding the HHEX-IDE, CDKAL1 and ADCY5 variants failed to reveal a significant effect (β = −24 g [95% CI −56, 9], p = 0.16).
Distribution of birthweight in 2,733 individuals with low (n = 1,366; white bars) and high (black bars) genetic risk (n = 1,367) from the Inter99 study. Raw birthweight data were plotted against number of individuals with either a low (<25 risk alleles) or high (≥25 risk alleles) genetic risk score. The effect, calculated adjusted for sex, maternal diabetes status and parity, was β = −35 g (95% CI −69, −2), p = 0.037
Discussion
Our analysis of the fetal genotype of 25 type 2 diabetes risk variants showed a novel association between ADCY5 rs11708067 risk allele and birthweight, with a 33 g reduction in birthweight per risk allele. Although this novel finding does not withstand correction for multiple testing in the Inter99 study population, independent statistical evidence for this locus was provided by Freathy et al. at the ASHG meeting 2009 [39]. Moreover, in meta-analyses we confirmed that the risk-conferring alleles at CDKAL1 and HHEX-IDE loci are associated with lower birthweight. Finally, we showed that no strong general effect on birthweight can be ascribed to the 25 type 2 diabetes risk alleles confirmed as of today. Our study thus adds important knowledge to current understanding of the effect of genes on birthweight and subsequent development of type 2 diabetes.
As fetal insulin is a crucial fetal growth factor, the ‘fetal insulin hypothesis’ suggests that genetic variants predisposing to decreased insulin secretion or action causes reduced intrauterine growth and thereby lower birthweight as well as late-onset type 2 diabetes [5]. This hypothesis assumes that insulin deficiency is already present during fetal life. Indeed, the birthweight-lowering alleles of CDKAL1 and HHEX-IDE predispose to type 2 diabetes due to reduced insulin secretion and beta cell dysfunction [11, 40]. The associations with lower birthweight for these two loci therefore support the ‘fetal insulin hypothesis’ by indicating that beta cell dysfunction may already be present in pre-natal life. This contrasts with other type 2 diabetes risk alleles that are also believed to increase susceptibility to type 2 diabetes through decreased beta cell function, but which were not found to have a decreasing effect on birthweight by us and others [32–34, 36]. No strong phenotype related to beta cell function has been reported for variants at the ADCY5 locus [13]; therefore the mechanism by which the ADCY5 risk allele decreases birthweight and increases the risk of type 2 diabetes may be different. Interestingly, the ADCY5 variant, but not the HHEX-IDE or CDKAL1 variant, was also significantly associated with a lower ponderal index, indicating that newborns with the ADCY5 variant had disproportional intrauterine growth. Thinness at birth, as reflected by a lower ponderal index, has been related to insulin resistance and type 2 diabetes later in life [41]. The CDKAL1 locus was significantly associated with reduced birth length, while ADCY5 and HHEX-IDE loci were not. These heterogeneous associations for the three loci could indicate differential effects, but may also be due to study sample size and thereby to lack of statistical power.
The ADCY5 locus was initially identified in a large meta-analysis of fasting plasma glucose levels, including data from 21 genome-wide association studies conducted by the Meta-Analyses of Glucose and Insulin-Related Traits Consortium (MAGIC) investigators [13, 31]. The intronic rs11708067 variant was associated with increased fasting plasma glucose levels (0.027 mmol/l, p = 1.7 × 10−14) and risk of type 2 diabetes (OR 1.12, p = 9.9 × 10−21) at a genome-wide level [13]. In the same study, the rs11708067 risk allele was also associated with decreased HOMA of beta cell function (HOMA-B) (p = 3.6 × 10−8) but not with HOMA of insulin resistance (p = 0.16). Simultaneously, a large meta-analysis undertaken by MAGIC investigators on post-OGTT values identified the ADCY5 locus to be associated with increased 2 h plasma glucose (0.09 mmol/l, p = 4.2 × 10−16) [31]. This association was reported with another single nucleotide polymorphism (rs2877716) in strong linkage disequilibrium with rs11708067 (HapMap CEU population r 2 = 0.82). The rs2877716 variant was also associated with lower 2 h serum insulin levels adjusted for 2 h plasma glucose levels (p = 1.43 × 10−6), but not with the insulinogenic index or AUC for insulin and glucose (p > 0.1) [31]. As variation in ADCY5 is associated with higher fasting and 2 h plasma glucose levels, as well as with lower HOMA-B and 2 h serum insulin levels in non-diabetic individuals, the ADCY5 variants may predispose to type 2 diabetes and low birthweight through an effect on insulin secretion rather than through insulin resistance. During revision of this manuscript Freathy et al. reported a meta-analysis of genome-wide association studies followed by replication studies showing that the C allele of rs9883204 in ADCY5 in linkage disequilibrium with rs11708067 (HapMap CEU phase III r 2 = 0.72) was associated with lower birthweight (p = 7 × 10−15) [42].
ADCY5 is expressed in multiple tissues including the pancreatic islets and beta cells, but with the highest expression levels observed in the heart and brain [13, 43]. ADCY5 (also known as AC5) encodes adenylate cyclase 5 (ADCY5), which catalyses generation of cyclic AMP. ADCY5 may be involved in insulin release, since cyclic AMP mediates activation of protein kinase A, which induces calcium influx, subsequent insulin secretion and transcription of the proinsulin gene [44]. Interestingly, Adcy5-knockout mice live significantly longer than control mice [45]. This has been proposed to be due to a protective effect on the heart, where disruption of ADCY5 inhibits cardiac apoptosis and thereby protects against pressure overload and oxidative stress [45, 46]. From these observations, it could be speculated that ADCY5 may also be involved in apoptosis of beta cells, possibly leading to decreased beta cell mass and decreased insulin-secreting capacity. This scenario could explain the associations with type 2 diabetes and low birthweight.
In the Danish Inter99 population as such, we were only able to show significant associations for the CDKAL1 and ADCY5 loci. In the present meta-analyses, we confirmed the associations with decreased birthweight for the HHEX-IDE and CDKAL1 loci. The lack of significant association for the HHEX-IDE variant in the Inter99 population may be due to insufficient statistical power, if the variant has a less pronounced impact on birthweight, as suggested previously [34]. In meta-analyses we also observed that fetal TCF7L2 rs7903146 and CDKN2A/B rs10811661 risk alleles were associated with slightly increased birthweight. Mother–offspring pair analyses have previously shown that this effect of the TCF7L2 risk allele is merely a reflection of the maternal genotype effect, which is observed because maternal and fetal genotypes are 50% correlated [36]. A maternal type 2 diabetes risk genotype may predispose to increased birthweight due to a predisposition towards increased glucose levels during pregnancy. The same explanation could account for the reported association between the CDKN2A/B risk allele and increased birthweight.
Although the individual effects of the three type 2 diabetes risk variants on birthweight are relatively small, combined additive analyses of CDKAL1, HHEX and ADCY5 showed a mean birthweight reduction of 110 g for carriers of five or six risk alleles compared with carriers of zero or one risk alleles. This magnitude can be compared with the impact of mothers smoking four additional cigarettes per day during third trimester of pregnancy [47].
The combined analysis of all 25 type 2 diabetes risk variants showed that individuals belonging to the high-risk group weighed marginally less than individuals belonging to the low-risk group. No significant effect was observed when excluding HHEX-IDE, CDKAL1 and ADCY5 from the analysis. This indicates that no strong general effect on birthweight can be ascribed to these 25 risk alleles. Together with the single variant analyses, the results from the combined analyses suggest that for some of the variants insulin deficiency and/or resistance may only be present later in life, while for others the defect may already be noticeable in pre-natal life. However, concordance between maternal and fetal genotypes may potentially offset the impact of fetal risk alleles, because mothers of newborns with a high number of risk alleles are likely to have a high number of risk alleles themselves, making them more susceptible to hyperglycaemia during pregnancy. Interestingly, none of the variants associated with insulin resistance seem to be associated with low birthweight. The 25 type 2 diabetes variants examined in the present study explain only ∼2% of the total variation in birthweight. The heritability of birthweight is 38%, as estimated in a Danish population-based twin cohort [48], suggesting that multiple additional genetic variants are likely to be involved. These may include yet undiscovered low-frequency variants overlapping with variants involved in type 2 diabetes pathogenesis, as well as variants with no influence on type 2 diabetes development. Moreover, the heritability estimate also suggests that the variation in birthweight is largely explained by non-genetic factors that may affect the intrauterine environment and thereby fetal growth [4, 48].
To strengthen the analyses, we have in the present study of Inter99 participants adjusted the analyses for sex, maternal diabetes status and parity, since these variables all affect birthweight in this population (personal communication, K. Pilgaard, Steno Diabetes Center, Gentofte, Denmark). Maternal diabetes status is related to genotype and offspring birthweight, and is therefore considered a confounding factor. In this study parental diabetes status was assessed through a questionnaire and age of onset was not reported, which is a limitation. However, higher birthweight in newborns whose mothers develop diabetes at some point in adult life has been reported [49]. This observation is probably explained by maternal hyperglycaemia during pregnancy, masking genetic effects working in the opposite direction and making it important to adjust for this confounder. However, adjusting for maternal diabetes status assessed several years after the pregnancy may not sufficiently account for the total effect of gestational hyperglycaemia, so we may have underestimated the effect of type 2 diabetes gene variants on birthweight in this study.
Another limitation of this study is the lack of exact information regarding gestational age between weeks 37 and 42. However, none of the investigated variants have to our knowledge been associated with gestational age and thus an even genotype distribution can be presumed. In addition, we do not have information on parental genotypes and could not therefore exclude a parental genotype effect.
In conclusion, we report a novel association with decreased birthweight in carriers of the ADCY5 type 2 diabetes risk allele. We also confirm associations with lower birthweight for the HHEX-IDE and CDKAL1 type 2 diabetes risk alleles in large meta-analyses.
Abbreviations
- CEU:
-
Centre d'Etude du Polymorphisme (Utah residents with northern and western European ancestry)
- HOMA-B:
-
HOMA of beta cell function
- MAGIC:
-
Meta-Analyses of Glucose and Insulin-Related Traits Consortium
References
Frayling TM, Hattersley AT (2001) The role of genetic susceptibility in the association of low birth weight with type 2 diabetes. Br Med Bull 60:89–101
Hales CN, Barker DJ, Clark PM et al (1991) Fetal and infant growth and impaired glucose tolerance at age 64. BMJ 303:1019–1022
Harder T, Rodekamp E, Schellong K, Dudenhausen JW, Plagemann A (2007) Birth weight and subsequent risk of type 2 diabetes: a meta-analysis. Am J Epidemiol 165:849–857
Poulsen P, Vaag AA, Kyvik KO, Moller Jensen D, Beck-Nielsen H (1997) Low birth weight is associated with NIDDM in discordant monozygotic and dizygotic twin pairs. Diabetologia 40:439–446
Hattersley AT, Tooke JE (1999) The fetal insulin hypothesis: an alternative explanation of the association of low birthweight with diabetes and vascular disease. Lancet 353:1789–1792
Hattersley AT, Beards F, Ballantyne E, Appleton M, Harvey R, Ellard S (1998) Mutations in the glucokinase gene of the fetus result in reduced birth weight. Nat Genet 19:268–270
Slingerland AS, Hattersley AT (2006) Activating mutations in the gene encoding Kir6.2 alter fetal and postnatal growth and also cause neonatal diabetes. J Clin Endocrinol Metab 91:2782–2788
Edghill EL, Bingham C, Ellard S, Hattersley AT (2006) Mutations in hepatocyte nuclear factor-1beta and their related phenotypes. J Med Genet 43:84–90
Stoy J, Edghill EL, Flanagan SE et al (2007) Insulin gene mutations as a cause of permanent neonatal diabetes. Proc Natl Acad Sci U S A 104:15040–15044
Pearson ER, Boj SF, Steele AM et al (2007) Macrosomia and hyperinsulinaemic hypoglycaemia in patients with heterozygous mutations in the HNF4A gene. PLoS Med 4:e118
Steinthorsdottir V, Thorleifsson G, Reynisdottir I et al (2007) A variant in CDKAL1 influences insulin response and risk of type 2 diabetes. Nat Genet 39:770–775
Bouatia-Naji N, Bonnefond A, Cavalcanti-Proenca C et al (2009) A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat Genet 41:89–94
Dupuis J, Langenberg C, Prokopenko I et al (2010) New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet 42:105–116
Lyssenko V, Nagorny CL, Erdos MR et al (2009) Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat Genet 41:82–88
Prokopenko I, Langenberg C, Florez JC et al (2009) Variants in MTNR1B influence fasting glucose levels. Nat Genet 41:77–81
Altshuler D, Hirschhorn JN, Klannemark M et al (2000) The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet 26:76–80
Gloyn AL, Weedon MN, Owen KR et al (2003) Large-scale association studies of variants in genes encoding the pancreatic beta-cell KATP channel subunits Kir6.2 (KCNJ11) and SUR1 (ABCC8) confirm that the KCNJ11 E23K variant is associated with type 2 diabetes. Diabetes 52:568–572
Nielsen EM, Hansen L, Carstensen B et al (2003) The E23K variant of Kir6.2 associates with impaired post-OGTT serum insulin response and increased risk of type 2 diabetes. Diabetes 52:573–577
Grant SF, Thorleifsson G, Reynisdottir I et al (2006) Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet 38:320–323
Saxena R, Voight BF, Lyssenko V et al (2007) Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 316:1331–1336
Scott LJ, Mohlke KL, Bonnycastle LL et al (2007) A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science 316:1341–1345
Sladek R, Rocheleau G, Rung J et al (2007) A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 445:881–885
Zeggini E, Scott LJ, Saxena R et al (2008) Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat Genet 40:638–645
Zeggini E, Weedon MN, Lindgren CM et al (2007) Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science 316:1336–1341
Yasuda K, Miyake K, Horikawa Y et al (2008) Variants in KCNQ1 are associated with susceptibility to type 2 diabetes mellitus. Nat Genet 40:1092–1097
Unoki H, Takahashi A, Kawaguchi T et al (2008) SNPs in KCNQ1 are associated with susceptibility to type 2 diabetes in East Asian and European populations. Nat Genet 40:1098–1102
Sandhu MS, Weedon MN, Fawcett KA et al (2007) Common variants in WFS1 confer risk of type 2 diabetes. Nat Genet 39:951–953
Gudmundsson J, Sulem P, Steinthorsdottir V et al (2007) Two variants on chromosome 17 confer prostate cancer risk, and the one in TCF2 protects against type 2 diabetes. Nat Genet 39:977–983
Winckler W, Weedon MN, Graham RR et al (2007) Evaluation of common variants in the six known maturity-onset diabetes of the young (MODY) genes for association with type 2 diabetes. Diabetes 56:685–693
Rung J, Cauchi S, Albrechtsen A et al (2009) Genetic variant near IRS1 is associated with type 2 diabetes, insulin resistance and hyperinsulinemia. Nat Genet 41:1110–1115
Saxena R, Hivert M-F, Langenberg C et al (2010) Genetic variation in GIPR influences the glucose and insulin responses to an oral glucose challenge. Nat Genet 42:142–148
Freathy RM, Bennett AJ, Ring SM et al (2009) Type 2 diabetes risk alleles are associated with reduced size at birth. Diabetes 58:1428–1433
Pulizzi N, Lyssenko V, Jonsson A et al (2009) Interaction between prenatal growth and high-risk genotypes in the development of type 2 diabetes. Diabetologia 52:825–829
Zhao J, Li M, Bradfield JP et al (2009) Examination of type 2 diabetes loci implicates CDKAL1 as a birth weight gene. Diabetes 58:2414–2418
Weedon MN, Frayling TM, Shields B et al (2005) Genetic regulation of birth weight and fasting glucose by a common polymorphism in the islet cell promoter of the glucokinase gene. Diabetes 54:576–581
Freathy RM, Weedon MN, Bennett A et al (2007) Type 2 diabetes TCF7L2 risk genotypes alter birth weight: a study of 24,053 individuals. Am J Hum Genet 80:1150–1161
Jorgensen T, Borch-Johnsen K, Thomsen TF, Ibsen H, Glumer C, Pisinger C (2003) A randomized non-pharmacological intervention study for prevention of ischaemic heart disease: baseline results Inter99. Eur J Cardiovasc Prev Rehabil 10:377–386
Glumer C, Jorgensen T, Borch-Johnsen K (2003) Prevalences of diabetes and impaired glucose regulation in a Danish population: the Inter99 study. Diab Care 26:2335–2340
RM Freathy US, I Prokopenko, DO Mook-Kanamori, et al. for the Early Growth Genetics Consortium (2009) New loci on chromosomes 3q25 and 3q21 are associated with size at birth. (Abstract # 87). Presented at the 59th Annual Meeting of The American Society of Human Genetics, 23 October 2009, Honolulu, Hawaii. Available at www.ashg.org/2009meeting/abstracts/fulltext/, accessed 1 May 2010
Grarup N, Rose CS, Andersson EA et al (2007) Studies of association of variants near the HHEX, CDKN2A/B, and IGF2BP2 genes with type 2 diabetes and impaired insulin release in 10,705 Danish subjects: validation and extension of genome-wide association studies. Diabetes 56:3105–3111
Phillips DI, Barker DJ, Hales CN, Hirst S, Osmond C (1994) Thinness at birth and insulin resistance in adult life. Diabetologia 37:150–154
Freathy RM, Mook-Kanamori DO, Sovio U et al (2010) Variants in ADCY5 and near CCNL1 are associated with fetal growth and birth weight. Nat Genet 42:430–435
Leech CA, Castonguay MA, Habener JF (1999) Expression of adenylyl cyclase subtypes in pancreatic beta-cells. Biochem Biophys Res Commun 254:703–706
Prentki M, Matschinsky FM (1987) Ca2+, cAMP, and phospholipid-derived messengers in coupling mechanisms of insulin secretion. Physiol Rev 67:1185–1248
Yan L, Vatner DE, O'Connor JP et al (2007) Type 5 adenylyl cyclase disruption increases longevity and protects against stress. Cell 130:247–258
Okumura S, Vatner DE, Kurotani R et al (2007) Disruption of type 5 adenylyl cyclase enhances desensitization of cyclic adenosine monophosphate signal and increases Akt signal with chronic catecholamine stress. Circulation 116:1776–1783
Bernstein IM, Mongeon JA, Badger GJ, Solomon L, Heil SH, Higgins ST (2005) Maternal smoking and its association with birth weight. Obstet Gynecol 106:986–991
Grunnet L, Vielwerth S, Vaag A, Poulsen P (2007) Birth weight is nongenetically associated with glucose intolerance in elderly twins, independent of adult obesity. J Intern Med 262:96–103
Hypponen E, Smith GD, Power C (2003) Parental diabetes and birth weight of offspring: intergenerational cohort study. BMJ 326:19–20
Acknowledgements
The authors wish to thank A. Forman, I.-L. Wantzin and M. Stendal for technical assistance, and A. L. Nielsen, G. Lademann and M. M. H. Kristensen for management assistance. The study was supported by grants from the Lundbeck Foundation Centre of Applied Medical Genomics for Personalized Disease Prediction, Prevention and Care (LuCAMP), the Danish Health Research Council, the European Union (EXGENESIS, grant no. LSHM-CT-2004-005272), the Danish Diabetes Association, the Danish Council for Independent Research (Medical Sciences) and Novo Nordisk. The Inter99 was initiated by T. Jørgensen (principal investigator), K. Borch-Johnsen (co-principal investigator), H. Ibsen and T. F. Thomsen. The Steering Committee comprises the former two and C. Pisinger. The study was financially supported by research grants from the Danish Research Council, the Danish Centre for Health Technology Assessment, Novo Nordisk, Research Foundation of Copenhagen County, Ministry of Internal Affairs and Health, the Danish Heart Foundation, the Danish Pharmaceutical Association, the Augustinus Foundation, the Ib Henriksen Foundation, the Becket Foundation and the Danish Diabetes Association.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
E. A. Andersson and K. Pilgaard contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 33 kb)
ESM Fig. 1
(PDF 81 kb)
Rights and permissions
About this article
Cite this article
Andersson, E.A., Pilgaard, K., Pisinger, C. et al. Type 2 diabetes risk alleles near ADCY5, CDKAL1 and HHEX-IDE are associated with reduced birthweight. Diabetologia 53, 1908–1916 (2010). https://doi.org/10.1007/s00125-010-1790-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-1790-0