Abstract
Aims/hypothesis
Using a mouse model of lipoatrophic diabetes, we hypothesised that the chemokine (C–C motif) ligand 2 (CCL2)/chemokine (C–C motif) receptor 2 (CCR2) pathway contributes to hepatic macrophage accumulation and insulin resistance through induction of a chronic inflammatory state.
Methods
Metabolic variables of insulin resistance and inflammation were characterised in wild-type and lipoatrophic A-ZIP/F-1 transgenic (AZIP-Tg) mice. The AZIP-Tg mice were then treated with a CCR2 antagonist (RS504393, 2 mg kg−1 day−1) or vehicle for 28 days via a subcutaneous mini-osmotic pump to examine the role of the CCL2/CCR2 pathway in lipoatrophic diabetes.
Results
The lipoatrophic AZIP-Tg mice were diabetic with high fasting glucose and serum insulin concentrations compared with littermate controls. The livers of AZIP-Tg mice were more than threefold enlarged and exhibited increased triacylglycerol content. CCL2 levels were highly elevated in both liver and serum of the AZIP-Tg mice compared with controls. In addition, the circulating CCL2 concentration was associated with increased macrophage accumulation and inflammation as documented by upregulation of Cd68 gene and Tnf-α [also known as Tnf] gene in livers from the AZIP-Tg mice. Treatment of the lipoatrophic AZIP-Tg mice with the CCR2 antagonist ameliorated the hyperglycaemia, hyperinsulinaemia and hepatomegaly in conjunction with a reduction in liver inflammation.
Conclusions/interpretation
These findings demonstrate a significant role of the CCL2/CCR2 pathway in lipoatrophy-induced diabetes and provide clear evidence that metabolic improvements resulting from the inhibition of this inflammatory pathway are not adipose tissue-dependent.
Similar content being viewed by others
Introduction
Liver steatosis afflicts approximately 20–30% of adults in the USA and other Western countries [1, 2] and has been associated with insulin resistance in both obese and lipodystrophic individuals [3, 4]. Liver steatosis is probably initiated at an early stage of type 2 diabetes without clinical symptoms or consequences. However, liver steatosis accompanied by other metabolic disorders more often progresses to severe stages of non-alcoholic fatty liver disease (e.g. steatohepatitis and cirrhosis) later in life, which is associated with a major compromise of liver function and increased morbidity [2].
Although liver steatosis is typically associated with excessive adipose tissue or alcohol intake, insufficient adipose tissue (lipoatrophy) also induces insulin resistance and promotes metabolic abnormalities such as dyslipidaemia, lipotoxicity and hepatic steatosis [5]. As adipose tissue is considered the primary site of triacylglycerol storage, the absence of adipose tissue has profound detrimental metabolic consequences. For example, human lipoatrophic patients (who lack adequate adipose tissue) store triacylglycerol in other insulin-responsive tissues such as liver and skeletal muscle. These patients typically have severe insulin resistance, hyperglycaemia and dyslipidaemia [6]. Similarly, A-ZIP/F-1 transgenic (AZIP-Tg) mice, a model of lipoatrophy, also have lipid accumulation in the liver, insulin resistance and diabetes [7]. Although a strong link is evident between hepatic steatosis and insulin resistance, the underlying mechanism for this link is poorly understood. The aetiology is considered to be dynamic and complex at both cellular and molecular levels with alterations in signalling molecules and upregulation of pro-inflammatory cytokines and chemokines.
Inflammation is believed to be a key factor in the development of both obesity- and lipoatrophy-induced type 2 diabetes. In obesity, the presence of excessive adipose tissue does not appear to inherently drive insulin resistance, rather the infiltration of adipose tissue by pro-inflammatory macrophage cells may initiate the detrimental effects of excess adiposity [8–10]. Similarly, the presence of increased lipid in the liver does not directly result in insulin resistance. Rather, the subsequent pro-inflammatory state of the liver that results from an excessive influx of NEFA appears to exert detrimental effects on insulin sensitivity [11–13]. Interestingly, liver inflammation appears to have several parallels to adipose tissue inflammation. The most striking parallel is macrophage infiltration of the inflamed tissue promoting a positive feedback of increased cytokine production and additional macrophage recruitment [8, 13–15]. In obesity, chemokine (C–C motif) ligand 2 (CCL2) has been demonstrated to be produced in adipose tissue by resident macrophages [16] and inhibition of its receptor (chemokine (C–C motif) receptor 2 [CCR2]) has resulted in improvements in insulin resistance and attributed to reductions in adipose tissue inflammation [17]. However, the potential role of the CCL2/CCR2 pathway to exert effects on insulin resistance independently of adipose tissue has not been examined. Furthermore, the role of this inflammatory pathway in lipoatrophic insulin resistance has not been described.
In this study of lipoatrophic mice, we observed a robust upregulation of CCL2 and hypothesised that the CCL2/CCR2 pathway in a model of lipoatrophy contributes to hepatic macrophage accumulation and insulin resistance. Whether the alteration in the CCL2/CCR2 pathway is functionally significant in the lipoatrophic diabetic mouse model was tested by treatment with a CCR2 antagonist.
Methods
Animals
AZIP-Tg FVB male and KK/HIJ female mice were purchased from Jackson Laboratory (Bar Harbor, ME, USA) and bred to generate FVB/KK F1 offspring. This breeding strategy was used to improve the viability of the offspring as AZIP-Tg mice on the FVB background have poor survival [18]. The AZIP transgene was genotyped and found to be in the expected Mendelian ratio (∼50%) with non-transgenic siblings. Mice were maintained in a temperature- and humidity-controlled room with a 12 h light/dark cycle and fed Purina LabDiet 5001 rodent chow diet (5% wt/wt fat; Purina Mills, Richmond, IN, USA) ad libitum. Purina LabDiet 5008 rodent chow diet (6.5% wt/wt fat; Purina Mills) was provided to breeders.
Blood and tissue collection
Twenty-week-old non-transgenic mice (wild-type, n = 23) and AZIP-Tg mice (n = 15) on the FVB/KK F1 background were anaesthetised with sodium pentobarbital after a 5 h fast and blood was collected via cardiac puncture. After blood collection, tissues were harvested and stored at −20°C or −80°C until further analysis. All animal experimental protocols were approved by the Animal Investigation Committee at Wayne State University.
Histology and immunohistochemistry
Livers from wild-type and AZIP-Tg mice were fixed overnight in 10% zinc formalin (vol./vol.), dehydrated in a graded series of alcohol washes, cleared in toluene and embedded in paraffin. Using a microtome, 5 µm sections were generated, collected on slides and then stained with haematoxylin and eosin. For immunohistochemistry, macrophages in liver sections were identified with anti-CD68 (1:50 dilution; AbD Serotec, Raleigh, NC, USA) and anti-integrin alpha M (CD11B; 1:10 dilution; AbD Serotec) monoclonal antibodies. Aminoethyl carbazole (Invitrogen, Carlsbad, CA, USA) staining followed by counterstaining with haematoxylin was performed.
Proteome profiler array
Following a 5 h fast, blood was collected from 13-week-old wild-type (n = 6) and AZIP-Tg (n = 3) mice. Blood was collected into serum separator tubes (BD, Franklin Lakes, NJ, USA) and allowed to clot for 2 h before being centrifuged at 2,000×g for 20 min. One hundred microlitres of serum was analysed using a proteome profiler array (Mouse Cytokine Array Panel A; R&D Systems, Minneapolis, MN, USA), which can identify 40 different cytokines simultaneously. Serum was conjugated with 40 different antibodies that were spotted in duplicate on nitrocellulose membranes. The conjugates were captured by horseradish peroxidase and were detected by chemiluminescence. The intensity of signals was scanned by a Chemidoc XRS gel scanner (Bio-Rad, Hercules, CA, USA) and quantified by densitometry.
Metabolic variables
Blood obtained via submandibular bleeding after a 5 h fast was immediately analysed for glucose concentration using a Glucometer Elite (Bayer, Mishawaka, IN, USA). Commercially available ELISA kits were used for the measurements of adiponectin (B-Bridge International, Mountain View, CA, USA), insulin and leptin (Crystal Chem, Downers Grove, IL, USA), CCL2 and IL-6 (R&D Systems), and plasminogen activator inhibitor-1 (PAI-1) (Molecular Innovations, Novi, MI, USA). Triacylglycerol concentration was measured with an enzymatic assay (Sigma, St Louis, MO, USA). Total cholesterol concentration was measured by a Cholesterol E test (Wako Pure Chemical Industries, Richmond, VA, USA). All values of triacylglycerol and total cholesterol in liver and muscle were normalised to protein concentration.
Gene expression analysis
Total RNA was isolated from liver with the use of an RNAqueous kit (Ambion, Austin, TX, USA). Reverse transcription was performed using a high-capacity cDNA RT kit (Applied Biosystems, Foster city, CA, USA) following the manufacturer’s instructions. mRNA expression was quantified by real-time PCR (Stratagene MX 3005P; Stratagene, La Jolla, CA, USA). Synthesised cDNA was mixed with TaqMan Universal PCR Master Mix (Applied Biosystems) and a gene-specific primer and probe mixture (TaqMan Gene Expression Assays; Applied Biosystems). Individual reactions for target and 18S cDNA were carried out separately with negative controls lacking cDNA. The conditions used were as follows: 50°C for 2 min, 95°C for 10 min followed by 40 cycles of denaturation (95°C for 15 s) and annealing/extension (60°C for 1 min). The cycle number for the threshold of detection was determined by MxPro QPCR software (Stratagene). mRNA expression of each target was normalised to that of the 18S gene and expressed as fold change relative to controls.
Treatment of CCR2 antagonist using osmotic pump implantation
In total, 23 AZIP-Tg mice at 4 weeks of age were treated with either the CCR2 antagonist (n = 11; six males and five females) or vehicle (n = 12; seven males and five females). The CCR2 antagonist, RS504393 (2 mg kg−1 day−1; Tocris Bioscience, Ellisville, MO, USA), or vehicle (50% DMSO in water [vol./vol.]) was administered by continuous subcutaneous infusion (0.11 µl/h) for 28 days via a mini-osmotic pump (Alzet Model 1004; Durect Corporation, Palo Alto, CA, USA). The osmotic pump was incubated in PBS for 24 h at 37°C prior to implantation and was implanted dorsally using isoflurane anaesthesia. The condition of mice and body weight were monitored daily following the pump implantation. Blood was collected at day 0, 14, and 28 following a 5 h fast and analysed for glucose and serum insulin. After treatment, blood and liver tissue were collected and stored for further analysis.
Statistical analysis
All statistical analyses were performed using SPSS 16.0 (SPSS, Chicago, IL, USA). Data are expressed as means ± SEM. The Student’s t test was performed to compare two groups. One-way ANOVA was used when more than two groups were compared and significance of observed differences among the groups was evaluated with a least significant difference post hoc test. Pearson’s correlation coefficients (r) were used to describe the linear association between variables. Values of p < 0.05 were considered statistically significant.
Results
AZIP-Tg mice are characterised by hepatic steatosis and insulin resistance
Body weights were similar in both groups within the same sex (Table 1). As expected, the expression of the AZIP transgene resulted in no discernible white adipose tissue in males or females (Fig. 1a, Table 1). Livers from AZIP-Tg mice showed hepatomegaly with 309–389% enlargement compared with wild-type mice and were pale in colour (Fig. 1b). Histological analyses demonstrated that AZIP-Tg livers were filled with large lipid droplets and had evidence of macrovesicular steatosis while wild-type livers exhibited a normal morphology (Fig. 1c,d). In addition, other collected organs (heart, spleen, kidney and lung) were heavier in AZIP-Tg mice demonstrating organomegaly compared with wild-type mice (Table 1). The AZIP-Tg mice were diabetic with high levels of fasting blood glucose and serum insulin compared with littermate controls (Fig. 2a,b). AZIP-Tg mice had very low or undetectable levels of serum leptin and adiponectin (Fig. 2c), demonstrating that these adipocytokines are primarily produced in adipose tissue. Levels of triacylglycerol and total cholesterol in plasma and liver were increased in AZIP-Tg mice (Fig. 2d–g), but muscle triacylglycerol was not affected (wild-type, 9.33 ± 1.36; AZIP-Tg, 6.66 ± 0.23 μg/mg protein; p = 0.100).
Representative photographs of wild-type and AZIP-Tg mice at age 20 weeks. Dorsal view (a) and liver appearance (b) of wild-type (left) and AZIP-Tg mice (right). Haematoxylin and eosin-stained sections of liver from wild-type (c) and AZIP-Tg mice (d). Original magnification, ×200 for light microscopy
Levels of fasting blood glucose (a), serum insulin (b) and leptin (c), plasma triacylglycerol (TG) (d) and total cholesterol (TC) (e), and liver TG (f) and TC (g) in wild-type and AZIP-Tg (AZIP) mice. Values of liver TG and TC were normalised with respect to protein concentrations. Data are means ± SEM (n = 10–21 per group). *p < 0.05 vs wild-type mice
Levels of CCL2 expression in liver and circulating CCL2 are highly increased in lipoatrophic AZIP-Tg mice
We expected that excessive secretion of pro-inflammatory mediators from liver would play a major role in lipoatrophy-induced insulin resistance. To characterise the main circulating cytokines altered in this extreme insulin-resistant state, we conducted a screening test of serum using a proteome profiler array. Among 40 tested cytokines, levels of circulating CCL2 were increased 9.8-fold in AZIP-Tg mice compared with wild-type littermates. Using this technique, no other cytokines were found to be consistently altered between wild-type and AZIP-Tg mice. It should be noted that this technique has less sensitivity compared with other techniques (e.g. ELISA and real-time PCR). Given that the cytokine array showed a robust elevation of circulating CCL2 in AZIP-Tg mice, we hypothesised that CCL2 may be a central mediator of pro-inflammatory conditions promoting insulin resistance in this lipoatrophic model. To provide a more sensitive determination of CCL2 concentration, CCL2 analyses in serum and liver were performed using ELISA. These studies revealed that serum CCL2 was significantly increased in both male and female AZIP-Tg mice compared with wild-type mice (Fig. 3a). Liver CCL2 protein levels were also significantly increased in both male (15.2-fold) and female (16.3-fold) AZIP-Tg mice compared with wild-type mice (Fig. 3b). A strong correlation was evident between circulating CCL2 and liver CCL2 concentrations (r = 0.937, p < 0.001), suggesting that the liver may direct the systemic elevations in CCL2. Subsequently, we performed gene expression studies and demonstrated that the Ccl2 mRNA expression in liver was highly upregulated (21.0-fold) in AZIP-Tg mice compared with wild-type littermates (Fig. 3c), providing further evidence that the liver was a source of the elevated CCL2.
Levels of circulating CCL2 and liver CCL2 expression in wild-type (white columns) and AZIP-Tg (black columns) mice. a Serum CCL2 concentrations were assessed by ELISA. b Liver CCL2 concentrations measured by ELISA. Values for liver were normalised with respect to protein concentrations. c Liver mRNA expression levels of Ccl2 were measured using real-time RT-PCR and were normalised with respect to those of the 18S gene. Data are means ± SEM (n = 13–18 per group). *p < 0.05 vs wild-type mice
To examine whether other markers of systemic inflammation were elevated in the lipoatrophic diabetic state, additional circulating inflammatory cytokines were assessed by ELISA. Serum IL-6 (wild-type, 0.60 ± 0.22; AZIP-Tg, 1.52 ± 0.35 pmol/l; p = 0.041) and plasma PAI-1 concentrations (wild-type, 78.67 ± 8.89; AZIP-Tg, 260.89 ± 47.33 pmol/l; p < 0.001) were significantly elevated in AZIP-Tg mice compared with wild-type littermates.
Elevated CCL2 is associated with increased macrophage accumulation and inflammation in livers from lipoatrophic mice
We next examined whether the elevation in CCL2 was associated with monocyte/macrophage recruitment, inflammation and hepatic steatosis using gene expression studies of the livers of wild-type and AZIP-Tg mice (Fig. 4). CD68 is a transmembrane glycoprotein that is specifically expressed by the monocyte and macrophage and is used as a macrophage-specific marker. We found an elevation in mRNA expression of Cd68 and the pro-inflammatory cytokine Tnf-α [also known as Tnf], in AZIP-Tg mice compared with wild-type littermate controls. The upregulated mRNA expression of Cd68 and Tnf-α in AZIP-Tg mice demonstrates a pro-inflammatory state with marked macrophage accumulation. In addition, mRNA expression of the Lpl gene for liver lipoprotein lipase (LPL) was highly upregulated in AZIP-Tg mice compared with wild-type mice, suggesting that LPL may contribute to the excessive fat accumulation in the liver of this lipoatrophic mouse model.
A correlational analysis was conducted by Pearson’s correlation coefficient using data from 20-week-old wild-type and AZIP-Tg mice. Liver CCL2 was positively associated with hepatomegaly (r = 0.483, p = 0.003), liver triacylglycerol content (r = 0.598, p < 0.001), liver Cd68 mRNA (r = 0.712, p = 0.006), serum CCL2 (r = 0.937, p < 0.001), serum insulin (r = 0.612, p < 0.001) and plasma PAI-1 (r = 0.872, p < 0.001).
Inhibition of the CCL2/CCR2 pathway using a CCR2 antagonist ameliorates lipoatrophy-induced insulin resistance and inflammation
To assess whether the lipoatrophy-induced elevation in CCL2 is functionally significant, the CCR2 antagonist, RS504393 (2 mg kg−1 day−1), was administered to the AZIP-Tg mice via mini-osmotic pumps for 28 days. Control pumps delivering only the vehicle were used for comparison. There was no difference in weight change between the groups during the 4 week infusion period. However, liver weight was significantly lower in the CCR2 antagonist-treated group compared with controls demonstrating reduced hepatomegaly (Table 2). This effect appeared liver-specific as other tissue weights were not different between groups following the treatment period (Table 2).
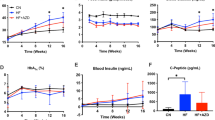
Despite no differences in weight gain during the treatment period, lipoatrophic mice given the CCR2 antagonist exhibited a significant improvement in concentrations of fasting blood glucose and serum insulin (Fig. 5a,b), consistent with a protective effect on the progression of diabetes in this mouse model. Plasma triacylglycerol and total cholesterol concentrations in plasma and liver were significantly lowered with the CCR2 antagonist treatment; however, the reduction of liver triacylglycerol concentration was not statistically significant (p = 0.144) (Fig. 5c–f). Levels of circulating CCL2 and liver CCL2 expression (protein and mRNA) were lower in the CCR2 antagonist-treated group (Table 3). Furthermore, the liver mRNA expression of Cd68 and Tnf-α were significantly lower in CCR2 antagonist-treated mice compared with vehicle-treated mice (Fig. 6), demonstrating an effective reduction in the pro-inflammatory state of the livers of these mice in parallel to the improvements in fasting glucose and insulin. Immunohistochemical analysis of macrophage markers, CD68 and CD11B, revealed that the CCR2 antagonist treatment reduced macrophage accumulation in liver (Fig. 7).
The beneficial effect of a CCR2 antagonist (RS504393) on fasting blood glucose (a), serum insulin (b), plasma triacylglycerol (TG) (c) and total cholesterol (TC) (d), and liver TG (e) and TC (f) in AZIP-Tg mice. Black circles, vehicle; white circles, CCR2 antagonist. Values of liver TG and TC were normalised with respect to protein concentrations. Data are means ± SEM (n = 10–12 per group). *p < 0.05 vs vehicle-treated mice
Gene expression analysis of Cd68 and Tnf-α in livers of vehicle- (white columns) or CCR2 antagonist (RS504393) (black columns)-treated AZIP-Tg mice. The gene expression levels were normalised with respect to those of the 18S gene. Data are means ± SEM (n = 10–12 per group). *p < 0.05 vs vehicle-treated mice
Discussion
Increasing evidence demonstrates that lipoatrophy induces insulin resistance with characteristics similar to those of obese individuals inflicted with hepatic steatosis [5, 6]. In this paper, we have demonstrated that lipoatrophy-induced lipid accumulation in the liver leads to a pro-inflammatory state similar to that observed in obesity-induced inflammation, marked by elevations in CCL2, TNF-α, PAI-1 and IL-6 [19, 20]. Of particular interest, we have demonstrated that blocking the CCL2/CCR2 pathway by use of a CCR2 antagonist results in attenuation of the lipoatrophy-induced inflammation and diabetes. Previous pre-clinical studies have provided evidence that the CCL2/CCR2 pathway improves insulin sensitivity in conjunction with reduced adipose tissue inflammation [17]. This paper extends our understanding of the role of the CCL2/CCR2 pathway in diabetes, as our results demonstrate an influential role of this pathway in the near or complete absence of adipose tissue.
Lipoatrophy-induced insulin resistance has been hypothesised to result from the toxicity of elevated circulating NEFA levels as well as increased lipid accumulation in insulin-sensitive tissues such as liver and muscle [5, 7]. Pro-inflammatory signals, which result from the accumulation of fatty acid metabolites in peripheral tissues, are often considered a central factor to explain both obesity- and lipoatrophy-induced insulin resistance [11–13, 21]. In normal physiological conditions, toxicity from excessive NEFA is prevented by well-controlled protective mechanisms including triacylglycerol synthesis, mitochondrial β-oxidation, binding to fatty acid binding proteins and secretion as VLDL [1]. However, when these mechanisms are compromised or become dysfunctional, the excess influx of NEFA into peripheral tissues is toxic to cells and results in membrane disruption, mitochondrial dysfunction and alterations in intracellular signalling pathways [1, 11–13]. The current study provides evidence that there is also a robust increase in CCL2 in both the liver and systemic circulation of lipoatrophic mice that parallels the metabolic abnormalities. Presumably, the excessive influx of NEFA into the liver triggers an activation of specific pro-inflammatory signalling pathways (e.g. inhibitor of kappa B kinase beta/nuclear factor-kappa B and Jun N-terminal kinase) that results in the overproduction of CCL2 and subsequent liver macrophage recruitment. This appears to be a detrimental positive feedback cycle resulting in an uncontrolled pro-inflammatory state and leading to the extreme hyperglycaemia, hepatic steatosis and hepatomegaly that is evident in lipoatrophy. The treatment of the lipoatrophic mice with a CCR2 antagonist provided a successful attenuation of this vicious cycle and resulted in a reduction in the diabetes as well as the hepatic steatosis, hepatomegaly and liver inflammation. Further studies are needed to examine whether interruption of the CCL2/CCR2 pathway following advanced disease progression has the same potent glucose-lowering effects.
It is well established that macrophage infiltration into adipose tissue and the pro-inflammatory state often found in obesity contribute to insulin resistance and the risk of diabetes [9, 10]. For example, increased levels of pro-inflammatory cytokines including CCL2, TNF-α, IL-8, IFN-gamma-inducible protein-10 and C-reactive protein have been observed in obese individuals [22, 23] and diabetic patients [24–26]. CCL2 has previously been identified as one cytokine which may mediate these pro-inflammatory signals in obesity and insulin resistance. In addition, inhibition of the CCL2 receptor, CCR2, in obese mice has been shown to improve insulin sensitivity and reduce macrophage content in adipose tissue [17]. Consistent with this importance of the CCL2/CCR2 pathway in obesity-induced insulin resistance, the suppression of CCL2 using a dominant-negative mutant improved insulin resistance in both genetically diabetic and high-fat diet-induced obese mouse models [16]. However, there is controversy regarding the importance of the CCL2/CCR2 pathway in promoting macrophage infiltration into adipose tissue. For example, a recent paper by Inouye et al. did not observe a reduction in macrophage infiltration and even demonstrated poorer metabolic control in high-fat fed Ccl2-deficient mice compared with their wild-type controls [27]. The authors suggested that differences in genetic backgrounds and colonies may contribute to the disparity of the results. Although this controversy persists in regard to the importance of CCL2/CCR2 in adipose tissue inflammation, the current paper demonstrates a beneficial metabolic effect of CCR2 antagonism mediated via an adipose tissue-independent mechanism.
We speculate that interruption of the CCL2/CCR2 pathway may provide an effective therapeutic strategy for attenuating the progression of hepatic steatosis. In the current paper, we did not begin with a bias towards the importance of the CCL2/CCR2 pathway. Rather, we were influenced by the striking CCL2 elevation and the strong relationship between liver CCL2 concentration and other measured metabolic variables. Therefore, to determine whether the CCL2/CCR2 pathway is causally related to the metabolic abnormalities, we directly inhibited the pathway using a CCR2 antagonist and evaluated the effects on lipoatrophy-induced insulin resistance. Interestingly, this 4 week treatment not only resulted in improved glucose homeostasis compared with vehicle-treated mice but also a reduced liver size (by approximately 25%) and less liver inflammation. This reduced liver size between CCR2 antagonist-treated and vehicle-treated mice suggests that suppression of the CCL2/CCR2 pathway is adequate to reduce the hepatomegaly that is so profound in the lipoatrophic AZIP-Tg mice. In addition, a recently published paper by Tamura et al. [28] cited a 30% reduction in liver size in obese (db/db) mice treated for 12 weeks with propergermanium, another CCR2 antagonist. Regarding the reduced liver inflammation, it is also noteworthy that our CCR2 antagonist treatment reduced levels of total cholesterol in plasma and liver. This suggests that total cholesterol may be associated with liver inflammation, as shown previously [29]. Taken together, these studies suggest that CCR2 inhibition results in the suppression of hepatomegaly, liver inflammation and insulin resistance. So, although important differences exist between lipoatrophy-induced hepatic steatosis and that seen in non-alcoholic fatty liver disease (e.g. the presence of circulating adipocytokines like leptin and adiponectin), there appears to be protective effects of CCR2 inhibition in both models. Future studies will need to evaluate the relevance of this inflammatory pathway in the progression of the hepatic steatosis that accompanies lipodystrophy resulting from HIV infection and highly active anti-retroviral therapy.
Two important points regarding the dose of CCR2 antagonist that we used are (1) it was lower than the dose used by other research groups [30, 31] and (2) it did not cause any noticeable negative side effects associated with toxicity, such as significant weight loss or excessive immunosuppression. We speculate from our data that a modest inhibition of CCR2 is adequate to disrupt the detrimental positive feedback cycle that results in the uncontrolled pro-inflammatory state evident in lipoatrophic mouse liver. Although CCL2 antagonists are currently unavailable, several CCR2 antagonists have been tested for drug development to suppress the CCL2/CCR2 pathway. In fact, disruption of the CCR2 pathway has already been considered for the treatment of atherosclerosis, inflammation, rheumatoid arthritis and multiple sclerosis [32]. In addition, several pre-clinical studies also have shown promise for CCR2 inhibition including protective effects on diabetic nephropathy [33], renal fibrosis [31], and high-fat diet-induced insulin resistance and glucose intolerance [17]. However, it is worth noting that the complete absence of CCR2 probably has detrimental effects. For example, mice with complete CCR2 deficiency (i.e. Ccr2 gene knockout) have been shown to have a disruption in normal monocyte recruitment to the liver following paracetamol-induced hepatoxicity [34]. Similarly, studies in gene knockouts of Ccl2 and Ccr2 have suggested that both factors are important early responders to virus-induced liver pathology [35]. Therefore, it appears that the complete disruption of this pathway comes with a compromise in regard to the repair of drug- and virus-induced liver injury. Nevertheless, we have demonstrated that a modest dose of CCR2 antagonist is adequate to induce significant protection from the associated metabolic perturbations of lipoatrophy. Our findings provide evidence that CCR2 inhibition may be an effective therapeutic strategy for the treatment of lipoatrophy-induced insulin resistance and hepatic steatosis.
Sex differences appear to exist for fatty liver disease with approximately twice the prevalence of non-alcoholic steatohepatitis among obese men compared with obese women at 40 years of age [36]. In addition, it is widely observed that women tend to have a later onset of fatty liver disease than men, a difference proposed to relate to oestrogen-mediated effects on lipid metabolism [37] and/or mitochondrial function [38]. However, in this study using the AZIP-Tg lipoatrophic mice, we observed strikingly similarly levels of hepatic steatosis and liver inflammation between male and female mice. In addition, the response to CCR2 antagonist treatment was also very similar in regard to the suppression of inflammation, reduction in hyperinsulinaemia and improvement in circulating triacylglycerol. Therefore, in this model of lipoatrophic hepatomegaly, the beneficial effect of CCR2 treatment does not appear to be sex-specific.
The present study demonstrates that lipoatrophic AZIP-Tg mice are characterised by extreme elevations in CCL2 as well as severe hepatomegaly, increased liver macrophage accumulation and diabetes. The interruption of the CCL2/CCR2 pathway results in an amelioration of the pro-inflammatory state, including a reduction in hyperglycaemia, hyperinsulinaemia, hepatomegaly and overall liver inflammation. Our findings demonstrate that beneficial effects of CCR2 inhibition extend well beyond adipose tissue inflammation and obesity-induced diabetes to include direct effects on liver inflammation, hepatic steatosis, and lipoatrophy-induced diabetes.
Abbreviations
- AZIP-Tg mice:
-
A-ZIP/F-1 transgenic mice
- CCL2:
-
Chemokine (C–C motif) ligand 2
- CCR2:
-
Chemokine (C–C motif) receptor 2
- CD11B:
-
Anti-integrin alpha M
- PAI-1:
-
Plasminogen activator inhibitor-1
References
Neuschwander-Tetri BA, Caldwell SH (2003) Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology 37:1202–1219
Rector RS, Thyfault JP, Wei Y, Ibdah JA (2008) Non-alcoholic fatty liver disease and the metabolic syndrome: an update. World J Gastroenterol 14:185–192
Yki-Jarvinen H, Westerbacka J (2005) The fatty liver and insulin resistance. Curr Mol Med 5:287–295
Wanless IR, Lentz JS (1990) Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology 12:1106–1110
Ganda OP (2000) Lipoatrophy, lipodystrophy, and insulin resistance. Ann Intern Med 133:304–306
Seip M, Trygstad O (1996) Generalized lipodystrophy, congenital and acquired (lipoatrophy). Acta Paediatr Suppl 413:2–28
Kim JK, Gavrilova O, Chen Y, Reitman ML, Shulman GI (2000) Mechanism of insulin resistance in A-ZIP/F-1 fatless mice. J Biol Chem 275:8456–8460
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116:1793–1801
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr (2003) Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 112:1796–1808
Xu H, Barnes GT, Yang Q et al (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112:1821–1830
Krebs M, Roden M (2005) Molecular mechanisms of lipid-induced insulin resistance in muscle, liver and vasculature. Diabetes Obes Metab 7:621–632
Delarue J, Magnan C (2007) Free fatty acids and insulin resistance. Curr Opin Clin Nutr Metab Care 10:142–148
Boden G, She P, Mozzoli M et al (2005) Free fatty acids produce insulin resistance and activate the proinflammatory nuclear factor-kappaB pathway in rat liver. Diabetes 54:3458–3465
Haukeland JW, Damas JK, Konopski Z et al (2006) Systemic inflammation in nonalcoholic fatty liver disease is characterized by elevated levels of CCL2. J Hepatol 44:1167–1174
Westerbacka J, Kolak M, Kiviluoto T et al (2007) Genes involved in fatty acid partitioning and binding, lipolysis, monocyte/macrophage recruitment, and inflammation are overexpressed in the human fatty liver of insulin-resistant subjects. Diabetes 56:2759–2765
Kanda H, Tateya S, Tamori Y et al (2006) MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J Clin Invest 116:1494–1505
Weisberg SP, Hunter D, Huber R et al (2006) CCR2 modulates inflammatory and metabolic effects of high-fat feeding. J Clin Invest 116:115–124
Moitra J, Mason MM, Olive M et al (1998) Life without white fat: a transgenic mouse. Genes Dev 12:3168–3181
Tilg H, Moschen AR (2006) Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol 6:772–783
Fantuzzi G (2005) Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol 115:911–919
Kolak M, Westerbacka J, Velagapudi VR et al (2007) Adipose tissue inflammation and increased ceramide content characterize subjects with high liver fat content independent of obesity. Diabetes 56:1960–1968
Dahlman I, Kaaman M, Olsson T et al (2005) A unique role of monocyte chemoattractant protein 1 among chemokines in adipose tissue of obese subjects. J Clin Endocrinol Metab 90:5834–5840
Kim CS, Park HS, Kawada T et al (2006) Circulating levels of MCP-1 and IL-8 are elevated in human obese subjects and associated with obesity-related parameters. Int J obesity 30:1347–1355
Herder C, Baumert J, Thorand B et al (2006) Chemokines as risk factors for type 2 diabetes: results from the MONICA/KORA Augsburg study, 1984–2002. Diabetologia 49:921–929
Barzilay JI, Abraham L, Heckbert SR et al (2001) The relation of markers of inflammation to the development of glucose disorders in the elderly: the Cardiovascular Health Study. Diabetes 50:2384–2389
Chen H, Ren A, Hu S, Mo W, Xin X, Jia W (2007) The significance of tumor necrosis factor-alpha in newly diagnosed type 2 diabetic patients by transient intensive insulin treatment. Diabetes Res Clin Pract 75:327–332
Inouye KE, Shi H, Howard JK et al (2007) Absence of CC chemokine ligand 2 does not limit obesity-associated infiltration of macrophages into adipose tissue. Diabetes 56:2242–2250
Tamura Y, Sugimoto M, Murayama T et al (2008) Inhibition of CCR2 ameliorates insulin resistance and hepatic steatosis in db/db mice. Arterioscler Thromb Vasc Biol 28:2195–2201
Wouters K, van Gorp PJ, Bieghs V et al (2008) Dietary cholesterol, rather than liver steatosis, leads to hepatic inflammation in hyperlipidemic mouse models of nonalcoholic steatohepatitis. Hepatology 48:474–486
Furuichi K, Wada T, Iwata Y et al (2003) CCR2 signaling contributes to ischemia-reperfusion injury in kidney. J Am Soc Nephrol 14:2503–2515
Kitagawa K, Wada T, Furuichi K et al (2004) Blockade of CCR2 ameliorates progressive fibrosis in kidney. Am J Pathol 165:237–246
Higgins P, Schwartz E, Nicolas J (2007) Small molecule CCR2 antagonists. In: Neote K, Letts G, Moser B (eds) Chemokine biology—basic research and clinical application. Birkhauser, Basel, pp 115–123
Kanamori H, Matsubara T, Mima A et al (2007) Inhibition of MCP-1/CCR2 pathway ameliorates the development of diabetic nephropathy. Biochem Biophys Res Commun 360:772–777
Dambach DM, Watson LM, Gray KR, Durham SK, Laskin DL (2002) Role of CCR2 in macrophage migration into the liver during acetaminophen-induced hepatotoxicity in the mouse. Hepatology 35:1093–1103
Hokeness KL, Kuziel WA, Biron CA, Salazar-Mather TP (2005) Monocyte chemoattractant protein-1 and CCR2 interactions are required for IFN-alpha/beta-induced inflammatory responses and antiviral defense in liver. J Immunol 174:1549–1556
Arun J, Clements RH, Lazenby AJ, Leeth RR, Abrams GA (2006) The prevalence of nonalcoholic steatohepatitis is greater in morbidly obese men compared to women. Obes Surg 16:1351–1358
Walsh BW, Schiff I, Rosner B, Greenberg L, Ravnikar V, Sacks FM (1991) Effects of postmenopausal estrogen replacement on the concentrations and metabolism of plasma lipoproteins. N Engl J Med 325:1196–1204
Grimbert S, Fisch C, Deschamps D et al (1995) Effects of female sex hormones on mitochondria: possible role in acute fatty liver of pregnancy. Am J Physiol 268:G107–G115
Acknowledgements
This work was supported by an American Diabetes Association Junior Faculty Award (J-05-JF-04). We thank G. Schweitzer for his technical assistance in muscle dissection.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, S.J., IglayReger, H.B., Kadouh, H.C. et al. Inhibition of the chemokine (C–C motif) ligand 2/chemokine (C–C motif) receptor 2 pathway attenuates hyperglycaemia and inflammation in a mouse model of hepatic steatosis and lipoatrophy. Diabetologia 52, 972–981 (2009). https://doi.org/10.1007/s00125-009-1309-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-009-1309-8