Abstract
Aims/hypothesis
Exposure to excess glucocorticoid is associated with pancreatic beta cell damage and decreased glucose-stimulated insulin secretion (GSIS). Inactive glucocorticoids (cortisone, 11-dehydrocorticosterone) are converted to active cortisol and corticosterone by 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1), which requires NADPH as cofactor, which is generated by hexose-6-phosphate dehydrogenase (H6PDH). We investigated the localisation and activity of 11β-HSD1 within pancreatic islets, and determined its functional role in the regulation of insulin and glucagon secretion.
Methods
mRNA expression of 11β-HSD1 (also known as HSD11B1), glucocorticoid receptor and H6PDH (also known as H6PD) in human pancreas and murine islets was examined by real-time PCR. 11β-HSD1 protein levels were examined by immunohistochemistry and immunofluorescence. 11β-HSD1 activity was assessed in intact tissue and isolated islets of wild-type (WT) and both 11β-Hsd1- and H6pdh-null mice. Glucagon secretion and insulin secretion were analysed by RIA and ELISA respectively in isolated murine islets incubated with dexamethasone.
Results
11β-HSD1 co-localised with glucagon in the periphery of murine and human islets, but not with insulin or somatostatin. Dexamethasone, 11-dehydrocorticosterone and corticosterone induced a dose-dependent decrease in GSIS and glucagon secretion following low glucose stimulation. Reduction of 11β-HSD1 activity with specific inhibitors or in experiments carried out in H6pdh-null mice reversed the effects of 11-dehydrocorticosterone, but had no effect following treatment with corticosterone.
Conclusions/interpretation
Local regeneration of glucocorticoid via 11β-HSD1 within alpha cells regulates glucagon secretion and in addition may act in a paracrine manner to limit insulin secretion from beta cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Exposure to glucocorticoid excess leads to a classical phenotype, including obesity, insulin resistance and in some cases type 2 diabetes. The precise mechanisms by which glucocorticoids mediate these effects are not fully defined. Acting through the glucocorticoid receptor (GR), glucocorticoids increase hepatic gluconeogenesis via the induction of key enzymes including glucose-6-phosphatase and phosphoenolpyruvate carboxykinase [1, 2], causing in addition global insulin resistance [3]. Both of these processes contribute to hyperglycaemia. They have also been shown to have a direct inhibitory effect on insulin release from pancreatic beta cells [4–6]. GR immunoreactivity has been found to be exclusively present in the nuclei and cytoplasm of beta cells of rat pancreatic islets [7]. The effects of glucocorticoid on insulin secretion are dependent upon the dose and duration of administration [8]. While most studies report inhibition of insulin secretion by glucocorticoids [5, 9–11], long-term culture in hydrocortisone [12] and dexamethasone-treatment of islets from adrenalectomised rats [13] increase insulin release. However, transgenic mice overexpressing GR (also known as NR3C1) specifically in the beta cell have impaired glucose tolerance due to decreased insulin release, suggesting a direct inhibitory action of glucocorticoid upon the beta cell [14].
Pre-receptor regulation of glucocorticoid availability by the enzyme 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1) has been implicated in the pathogenesis of the metabolic syndrome, obesity and type 2 diabetes [15]. 11β-HSD1 is present at high levels in liver, adipose tissue and muscle, but it has also been reported to be present in pancreatic islets [4]. The activity of 11β-HSD1 primarily generates active glucocorticoid and cortisol (corticosterone in rodents) from inactive cortisone (11-dehydrocorticosterone in rodents) via its oxo-reductase activity [16]. Critically, this oxo-reductase activity is cofactor (NADPH)-dependent and regulated by a tightly associated endo-luminal enzyme, hexose-6-phosphate dehydrogenase (H6PDH). Decreases in H6PDH production and activity have been shown to decrease 11β-HSD1 oxo-reductase and increase dehydrogenase activity [17].
Rodent models have significantly contributed to our understanding of the role of 11β-HSD1 in the pathogenesis of disease. Tissue-specific overexpression models in liver and adipose tissue have highlighted potentially important roles in the control of adiposity, carbohydrate metabolism and insulin sensitivity [18–20]. 11β-Hsd1-null mice are protected from the metabolic consequences of obesity and have improved glucose tolerance in comparison with wild-type (WT) animals [21]. Similarly, H6pdh knockout animals have improved glucose tolerance [22]. However, studies examining insulin secretion in these animals in response to glucose administration, either in vivo or in explanted tissues, have not been performed. In both of these models, decreased glucocorticoid generation within the pancreatic islet may contribute to their phenotype.
11β-Hsd1 mRNA, and 11β-HSD1 protein and dehydrogenase activity have been detected in islets isolated from ob/ob mice [4, 6]. While enzyme activity and cellular localisation studies have not been performed, incubation with 11-dehydrocorticosterone decreased glucose-stimulated insulin secretion (GSIS) in a dose-dependent manner. This was reversed by incubation with 11β-HSD1 inhibitors carbenoxolone [4, 6] and BVT.2733 [6], and partially reversed by GR antagonist RU38486 [6].
The evidence for glucocorticoid modulation of insulin secretion is clear. However, the contribution of pre-receptor glucocorticoid metabolism through 11β-HSD1 needs to be clarified. Furthermore, the impact upon glucagon secretion has not been examined. The aims of this study were to determine the precise cellular localisation of 11β-HSD1 in mouse and human pancreatic islets and to assess the functional impact of 11β-HSD1 on islet insulin and glucagon secretion.
Methods
Animals
We used 10- to 12-week-old male and female C57BL/6 mice unless otherwise specified. All procedures were carried out in accordance with the UK Animals (Scientific Procedures) Act, 1986. Mice with a targeted inactivation of H6pd (H6PDH-KO) were generated as previously described [22]. 11β-Hsd1-null mice (11β-HSD1-KO) were generated in-house (G. G. Lavery, unpublished data). Where human samples were used, local research ethics committee approval was in place.
Tissue collection and histology
Mice were killed by cervical dislocation and the whole pancreas immediately removed. Tissues were fixed in 10% (vol./vol.) formalin, embedded in a random orientation in paraffin and cut into 5 μm sections. Liver and kidney were collected and prepared as positive controls. Human pancreatic tissue was obtained with appropriate ethical approval from the South Birmingham Regional Ethics Committee. Tissue was excised by the consultant pathologist reporting the specimen, with ‘normal’ resection margins observed for distance from the pancreatic tumour in Whipple’s specimens. All samples were processed immediately after collection from the operating theatre.
Immunohistochemistry and immunofluorescence
Sub-cellular localisation of the pancreatic hormones insulin, glucagon, somatostatin and pancreatic polypeptide, as well as 11β-HSD1 and GR from both male and female murine tissues was assessed using immunohistochemistry. Slides underwent dewaxing, rehydration, antigen retrieval in citrate buffer and treatment with methanol-hydrogen peroxide (1:1000, vol./vol.). Slides were blocked for non-specific binding in 10% (vol./vol.) normal donkey serum. Antibodies for insulin and glucagon were raised in mice (Sigma, Poole, UK) and used at a dilution of 1:500. Rabbit anti-somatostatin (VectorLab, Burlingame, CA, USA) and anti-pancreatic polypeptide (Progen, Heidelberg, Germany) were used at 1:50 and mouse anti-GR (Affinity BioReagents, Golden, CO, USA) at 1:10 dilutions. The antibody for 11β-HSD1 was raised in sheep (amino acid residues 18–33), as previously reported [23] and used at a dilution of 1:100. The negative control for 11β-HSD1 comprised the primary antibody preabsorbed with the immunising peptide at a dilution of 1:100, while the negative controls for pancreatic hormones and GR were carried out using normal donkey or goat serum respectively in place of a primary antibody. All slides were incubated with the primary antibody or serum substitute for 90 min. Horseradish peroxidase-conjugated secondary antibodies raised against mouse (VectorLab), rabbit (Dako, Glostrup, Denmark) and sheep (The Binding Site, Birmingham, UK) were added for 30 min at 1:100 working dilution. Staining was detected using peroxidase substrate 3,3′-diaminobenzidine (Sigma). All sections were counterstained with Mayer’s Haematoxylin and mounted with DPX (BHD, Poole, UK). This technique was repeated eight times for consistency. Human pancreas sections were processed in the same way.
Immunofluorescence was carried out to detect co-localisation of 11β-HSD1 with each of the pancreatic hormones. Primary antibodies were as described above. Anti-mouse Texas Red, anti-rabbit Texas Red (VectorLab) and anti-sheep FITC (The Binding Site) were used at a dilution of 1:100 and slides were covered in foil for the remainder of the procedure. Slides were mounted in Prolong Gold antifade reagent with DAPI (Invitrogen, Paisley, UK).
Islet isolation and treatment
Female mice were killed by cervical dislocation and the pancreas removed to 0.1% (vol./vol.) KRB on ice. The organ was inflated with a cocktail of liberase (Roche, Lewes, UK) and trypsin inhibitors (Sigma, UK), and digested by repeated cycles of manual shaking followed by incubation in a 37°C water-bath for 3 min until digestion was complete. Tissue was pelleted and washed three times with KRB. Islets were hand-picked under a dissection microscope and incubated for 12 to 16 h in 12 mmol/l glucose RPMI media, with or without a range of treatments and inhibitors as outlined in the Results.
For analysis of insulin secretion, three islets were seeded per well in a 96 well plate, equilibrated to 3 mmol/l glucose in KRB and then treated for a further 2 h with the same control or glucocorticoid treatment at a concentration of 3 or 20 mmol/l glucose. Selective inhibition of 11β-HSD1 was tested using a novel pharmaceutical compound (PF-877423; Pfizer Global, La Jolla, CA, USA) [24]. Treatments were repeated using islets from H6PDH-KO mice.
For glucagon analysis, five islets were used per well in silicon-coated plates and were treated with glucocorticoid in 7 mmol/l or 1 mmol/l glucose.
Hormone concentrations were assayed in cell culture media using mouse insulin ELISA (Mercodia, Uppsala, Sweden) or glucagon RIA (Millipore, Billerica, MA, USA). Glucose-stimulated insulin (20 mmol/l glucose) and glucagon (1 mmol/l glucose) concentrations for control and glucocorticoid-treated islets were normalised to their equivalent basal concentrations (3 and 7 mmol/l glucose respectively). Resulting fold-change values were analysed by one-way ANOVA; all data were tested for homogeneity of variance and significant differences were further investigated by Bonferroni post hoc tests.
RNA extraction, RT reaction and real-time PCR
Sufficient human samples were only available for immunohistochemical analysis; gene expression studies were therefore performed on commercially available pancreatic RNA (Clontech Laboratories, Mountainview, CA, USA). Mouse islet RNA was extracted from isolated islets using a kit (GenElute mammalian Total RNA Miniprep; Sigma) according to the manufacturer’s protocol. Integrity and concentration of RNA was assessed by electrophoresis and spectrophotometry, respectively. Reverse transcription of 1 μg of total RNA was carried out using a kit (Multiscribe enzyme kit; Applied Biosystems, Warrington, UK) at 37°C for 1 h.
Quantitative mRNA expression levels of 11β-HSD1, H6PDH and GRα were measured by real-time PCR using an ABI 7500 system (Perkin-Elmer Biosystems, Warrington, UK). PCR was performed in 25 µl reactions on 96 well plates. Reactions contained TaqMan universal PCR master mix (Applied Biosystems), 900 nmol primers, 100–200 nmol TaqMan probe and 25–50 ng cDNA. All reactions were correlated to expression of ribosomal 18S rRNA (provided as a pre-optimised mix; Perkin-Elmer) as an internal reference. All target gene probes were labelled with the fluorescent label carboxyfluorescein and the 18S probe with the fluorescent label VIC. Reactions were as follows: 50°C for 2 min, 95°C for 10 min and then 40 cycles of 95°C for 15 s and 60°C for 1 min. Data were analysed according to the manufacturer’s guidelines. They were obtained as C t values (the cycle number at which logarithmic PCR plots cross a calculated threshold line) and used to determine ΔC t values (ΔC t = C t of the target gene minus C t of the internal reference, 18S). Real-time primers and probes for 11β-HSD1, H6PDH and GRα were purchased as pre-designed expression assays (Applied Biosystems).
11β-HSD1 activity assay
Conversion of 11-dehydrocorticosterone to corticosterone was determined by incubating intact murine pancreatic tissue or 120 isolated islets in 100 nmol/l 11-dehydrocorticosterone and tracer amounts of 11-[3H]dehydrocorticosterone (50,000 cpm) that was synthesised in-house. Conversion of dehydrogenase activity was measured by similar incubation in 100 nmol/l corticosterone and tracer amounts (1.5 nmol/l) of [3H]corticosterone (Perkin-Elmer).
After 24 h incubation, steroids were extracted from the medium with ten volumes of dichloromethane, separated by thin-layer chromatography with chloroform:ethanol (92:8, vol./vol.) as a mobile phase and the fractional conversion of steroids was calculated after scanning analysis using a Bioscan 2000 radioimaging detector (Bioscan, Washington, DC, USA). Activity was expressed as pmol g−1 h−1 where g represented total protein for islets or wet weight of tissue. The assay was repeated using isolated islets and pancreatic tissue from 11β-HSD1-KO and H6PDH-KO mice.
Results
11β-Hsd1 expression and 11β-HSD1 activity in murine and human pancreas
Immunohistochemistry revealed that insulin was localised to the core of the murine endocrine islets (Fig. 1a), while glucagon, somatostatin and pancreatic polypeptide were localised to the periphery (Fig. 1b–d). 11β-HSD1 was predominantly localised to the periphery of the islet (Fig. 1e). GR staining occurred throughout the whole islet and additionally in the pancreatic exocrine tissue (Fig. 1g). These observations were endorsed in human pancreatic tissue with positive 11β-HSD1 immunostaining mainly in the periphery of the islet, together with glucagon, in contrast to central insulin staining (Fig. 2a–c).
Immunostaining of representative murine pancreatic sections for insulin (a), glucagon (b), somatostatin (c), pancreatic polypeptide (d), 11β-HSD1 in pancreas (e) and in liver as a positive control (f), and GR in pancreas (g) and liver (h). Images are presented adjacent to their respective negative controls (right). Magnifications as shown
To provide a more accurate insight into cellular localisation, immunofluorescence staining of murine pancreatic sections was undertaken. 11β-HSD1 did not co-localise with insulin (Fig. 3a) or somatostatin (Fig. 3c). However, staining for 11β-HSD1 did co-localise with glucagon within alpha cells (Fig. 3b) and with pancreatic polypeptide (Fig. 3d).
Immunofluorescence staining of mouse pancreatic islet for insulin (a), glucagon (b), somatostatin (c) and pancreatic polypeptide (d) are shown in red. 11β-HSD1 immunofluorescent staining is shown in green. Positive yellow staining indicates that 11β-HSD1 is co-localised with glucagon- and pancreatic polypeptide-producing cells. Magnification ×40
Functional 11β-HSD1 enzyme activity was observed in WT murine pancreatic explant tissue. Activity was predominantly oxo-reductase, generating the active glucocorticoid, corticosterone (mean±SEM, 61.2 ± 6.4 pmol g−1 h−1, n = 4) (Fig. 4a), but dehydrogenase activity was also detected (13.1 ± 6.2 pmol g−1 h−1, n = 7). Using isolated intact islets, oxo-reductase activity again predominated, but bidirectional activity was observed (oxo-reductase 222 ± 23, dehydrogenase 184 ± 24 pmol g−1 h−1, n = 3) (Fig. 4b). Using real-time PCR, 11β-HSD1-KO mice had no detectable 11β-Hsd1 mRNA expression in liver, muscle and pancreatic islets, contrasting with our observations in WT animals (mean ΔC t ± SE 4.5 ± 0.1 [liver], 13.1 ± 0.1 [muscle], 18.1 ± 0.1 [pancreatic islet]; n = 3). In addition, there was no detectable oxo-reductase or dehydrogenase activity in microsomes from 11β-HSD1-KO liver, adipose tissue or muscle (data not shown). As expected, in 11β-HSD1-KO mice activity was abolished in whole tissue explants (n = 5) and isolated islets (n = 2). However, while H6PDH-KO mice lacked 11β-HSD1 oxo-reductase activity, dehydrogenase activity increased (tissue 23.7 ± 4.0 pmol g−1 h−1, p = NS, n = 6; islets 272 ± 73 pmol g−1 h−1, n = 2) (Fig. 4a,b).
Real-time PCR showed that 11β-HSD1, H6PDH and GRα were all expressed in murine islets and human pancreas. ΔCt values expressed relative to 18S as internal housekeeping control are presented in Table 1 (n = 6).
Functional impact of glucocorticoid metabolism on insulin and glucagon secretion
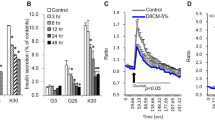
In all experiments, isolated islet viability was confirmed through the ability to secrete insulin following exposure to high glucose concentrations (20 mmol/l, data not shown). Preliminary data demonstrated no difference in the response in male and female mice (data not shown); in subsequent experiments only female mice were used. Dexamethasone treatment (0.5, 5 and 50 nmol/l for 2 h) decreased GSIS in a dose-dependent manner (18.7 ± 2.5 [control], 4.7 ± 1.8 [0.5 nmol/l] p < 0.05, 2.3 ± 0.9 [5 nmol/l] p < 0.001, 1.9 ± 1.0 [50 nmol/l] p < 0.001, n = 6; data expressed as fold increase in insulin secretion following high glucose stimulation). In addition, the effect of dexamethasone (50 nmol/l) was partially reversed by co-incubation with the GR antagonist RU38486 (1.9 ± 1.0 [dexamethasone] vs 11.1 ± 9.6-fold [dexamethasone + RU38486], p = 0.07, n = 6) (Fig. 5a).
Similarly, dexamethasone (2 h) decreased glucagon secretion from isolated islets following induction of hypoglycaemia (3.6 ± 0.6 [control], 2.1 ± 0.5 [0.5 nmol/l], 1.0 ± 0.2 [5 nmol/l] p < 0.05, 1.1 ± 0.2 [50 nmol/l], n = 4; data expressed as fold increase in glucagon secretion following low glucose stimulation). While co-incubation of dexamethasone with RU38486 increased glucagon secretion, this failed to reach statistical significance (1.1 ± 0.2 [dexamethasone] vs 1.9 ± 0.1 [dexamethasone + RU38486] p = NS, n = 4) (Fig. 5b).
To assess the impact of pre-receptor glucocorticoid metabolism upon insulin and glucagon secretion, endogenous rodent glucocorticoids, 11-dehydrocorticosterone and corticosterone, were used. Consistent with the activation of 11-dehydrocorticosterone to corticosterone by 11β-HSD1, both 11-dehydrocorticosterone and corticosterone inhibited GSIS in WT islets (28.8 ± 0.9 [control], 6.8 ± 3.2 [50 nmol/l 11-dehydrocorticosterone], 5.6 ± 2.2 [50 nmol/l corticosterone], p < 0.01; data expressed as fold increase in insulin secretion following high glucose stimulation) (Fig. 6a). Specific 11β-HSD1 inhibition with PF-877423 ablated the effect of 11-dehydrocorticosterone (6.8 ± 3.2 [50 nmol/l 11-dehydrocorticosterone] vs 30.2 ± 5.1 [50 nmol/l 11-dehydrocorticosterone + PF-877423], p < 0.01) but had no effect on the impact of corticosterone treatment (5.6 ± 2.2 [50 nmol/l corticosterone] vs 6.8 ± 0.01 [50 nmol/l corticosterone + PF-877423], p = NS). Furthermore, treatment with corticosterone in isolated islets from H6PDH-KO mice (which are unable to convert 11-dehydrocorticosterone to corticosterone) decreased GSIS, while treatment with 11-dehydrocorticosterone was without effect (8.0 ± 0.4 [control], 3.4 ± 0.7 [50 nmol/l corticosterone] p < 0.001, 8.3 ± 0.06 [50 nmol/l 11-dehydrocorticosterone], p = NS) (Fig. 6b).
In WT islets, corticosterone (CORT) and 11-dehydrocorticosterone (11DHC) decreased GSIS in isolated intact murine pancreatic islets. Co-incubation of 11-dehydrocorticosterone with the selective 11β-HSD1 inhibitor, PF-877423, completely abolished its action (a). Consistent with a lack of 11β-HSD1 oxo-reductase activity in islets isolated from H6PDH-KO mice, GSIS was decreased by corticosterone, but 11-dehydrocorticosterone was without effect (b). Similarly (c), the ability of 11-dehydrocorticosterone (but not corticosterone) to decrease glucagon secretion in WT pancreatic islets was partially reversed by co-incubation with PF-877423. *p < 0.05, **p < 0.01, ***p < 0.001
In WT islets, 11-dehydrocorticosterone and corticosterone inhibited glucagon secretion following low glucose stimulation (3.0 ± 0.9 [control], 1.2 ± 0.1 [50 nmol/l 11-dehydrocorticosterone] p < 0.05, 1.5 ± 0.1 [50 nmol/l corticosterone] p < 0.05, n = 4; data expressed as fold increase in glucagon secretion) (Fig. 6c). Co-incubation of 11-dehydrocorticosterone with the specific 11β-HSD1 inhibitor PF-877423 partially restored glucagon secretion (1.2 ± 0.1 [50 nmol/l 11-dehydrocorticosterone] vs 1.9 ± 0.3 [50 nmol/l 11-dehydrocorticosterone + PF-877423], p < 0.05). In contrast, co-incubation of corticosterone and PF-877423 was without effect (1.5 ± 0.1 [50 nmol/l corticosterone] vs 1.1 ± 0.2 [50 nmol/l corticosterone + PF-877423] p = NS) (Fig. 6c).
Discussion
In this study, we have characterised the expression and activity of 11β-HSD1 in the mouse and human pancreas. While we performed detailed studies on murine pancreas and isolated islets, our studies in humans were more limited due to tissue sample availability. We have shown that pre-receptor metabolism of endogenous glucocorticoid has significant implications for the control of insulin and glucagon secretion. Immunohistochemical analysis of 11β-HSD1 in pancreatic islets demonstrated localisation within the glucagon-producing alpha cells and not in the beta cells in human and murine tissue. Previous studies have shown 11β-Hsd1 mRNA expression in the ob/ob mouse and human islets using RT-PCR [4], but crucially this present study has now determined the precise localisation of 11β-HSD1 within islets at the protein level. Previous studies had failed to show convincing protein levels in rat pancreatic islets [25]. Species differences in expression may be important and our observations with regard to GR abundance would endorse this. We observed GR immunoreactivity throughout the whole murine islet and not exclusively in the beta cells as reported in rat tissue [7].
Our mRNA expression data endorse the observations in other rodent models [4] and extend these findings to human samples. While whole-islet expression levels were lower than those seen in liver and fat, this may be an underestimate of specific alpha cell expression, due to the high proportion of beta cells within the islet that, based upon our immunohistochemical analysis, were lacking in 11β-HSD1 expression.
Demonstrating functional enzyme activity is fundamentally important. We have shown that 11β-HSD1 is active within the islet and is capable of generating active glucocorticoid with predominant oxo-reductase activity. Other studies have only inferred 11β-HSD1 activity based upon observations following the use of 11β-HSD1 inhibitors [4]. However, we have now extended these findings and shown that, in knockout rodent models and following treatment with a selective 11β-HSD1 inhibitor, enzyme activity and active glucocorticoid generation is decreased.
Our data are consistent with previous observations that have shown decreased GSIS following glucocorticoid treatment [4]. GR overproduction in rodent beta cells leads to impaired glucose tolerance, decreased insulin secretion, hyperglycaemia and eventual diabetes in the context of unaltered insulin sensitivity [14]. The mechanisms that underpin these observations are poorly understood, but all of the following have been implicated: decreased GLUT2 protein stability [26]; increased glucose-6-phosphatase activity [27], glucose cycling [28], neuropeptide Y expression [29] and α2-adrenergic receptor expression [30]; decreased efficacy of cytoplasmic calcium ions on the exocytotic machinery [5]; and a reduction of insulin gene expression resulting in decreased insulin content [31].
The action of glucocorticoid upon glucagon secretion is more controversial with discrepancies reported in the literature. Results vary widely across species and with experimentation methods including clinical studies [32], animal models and islets in vitro [33]. Pre-treatment of mice with prednisolone increased glucagon release from the isolated islets [33], but glucocorticoids also decrease glucagon receptor expression [34]. In clinical studies, endogenous or exogenous glucocorticoid excess results in an increase in glucagon secretion [32]. However, the pathophysiological environment in these studies is complex, with a direct action of glucocorticoid upon carbohydrate metabolism (including glycogenolysis and gluconeogenesis) as well as insulin sensitivity. Therefore, extrapolation to a direct impact upon the glucagon-producing cells in the islet is difficult. In contrast to our observations with GSIS, RU38486 did not completely abolish the effects of dexamethasone upon glucagon secretion. This may reflect the complexities underpinning the regulation of glucagon secretion or the lack of specificity of action of RU38486. However it also raises the possibility that regulation of glucagon secretion by glucocorticoid may be controlled, at least in part, by non-GR-dependent mechanisms that have been described in other tissues [35].
Interestingly, glucagon stimulates insulin secretion from neighbouring beta cells by cAMP- and protein kinase A-dependent mechanisms [36]. Glucagon receptor knockout mice have diminished GSIS compared with WT mice, suggesting that disruption of glucagon signalling affects the insulin secretory pathway [37]. Human beta cells express functional glucagon receptors, which can generate signals for GSIS [38]; a glucocorticoid-mediated reduction in receptor number [34] could therefore impair insulin secretion.
The contribution of pre-receptor cortisol metabolism to the control of insulin and glucagon secretion has been explored in less detail. Incubation of islets from ob/ob mice in the presence of 11-dehydrocorticosterone led to a dose-dependent inhibition of insulin release, which was reversed with the non-selective 11β-HSD1 inhibitor, carbenoxolone, or with the selective 11β-HSD1 inhibitor, BVT.2733 [4, 6]. However, this inhibition of insulin release could not be repeated using islets from normal (C57BL/6) mice [6]. The reason for this discrepancy is not clear, but it may relate to basal levels of 11β-HSD1. Our data clearly demonstrate the negative impact of synthetic and endogenous glucocorticoids (active and inactive) upon GSIS and glucagon secretion, and have shown that the ability of 11-dehydrocorticosterone to inhibit GSIS and glucagon secretion is dependent upon its activation to corticosterone by 11β-HSD1. Blocking 11β-HSD1 oxo-reductase activity by means of a selective inhibitor or in rodent models that lack H6PDH and have decreased 11β-HSD1 oxo-reductase activity as a consequence of impaired cofactor generation completely reversed the impact of 11-dehydrocorticosterone in our studies.
The novel findings in this study make it conceivable that 11β-HSD1 and its ability to generate active glucocorticoid within the islet impact upon insulin and glucagon secretion by three distinct mechanisms: (1) directly at the level of the alpha cell, modulating glucagon secretion; (2) by decreasing glucagon secretion, which may decrease insulin secretion via glucagon receptors expressed on the beta cells (as described above); and (3) by glucocorticoid production from alpha cells acting in a paracrine manner, regulating insulin secretion from neighbouring beta cells.
Selective 11β-HSD1 inhibitors decrease local glucocorticoid generation in rodent and primate models and in humans [39–41]. To date, clinical efficacy has only been demonstrated in rodents, which showed improved glucose tolerance and lipid profiles, as well as increased insulin sensitivity and decreased atherogenesis [42, 43]. Studies to determine a specific impact upon insulin secretion have not been performed. However, if our observations are extrapolated to whole animal studies, enhanced insulin secretion may contribute to the beneficial effects of selective 11β-HSD1 inhibitors. Our observations in islets isolated from 11β-Hsd1 and H6pdh knockout animals may partially explain the improved glucose tolerance in these animals as a consequence of increased insulin secretion following glucose stimulation secondary to decreased local glucocorticoid availability [21, 22].
In summary, we have shown that 11β-HSD1 is localised to the alpha cells within pancreatic islets. Glucocorticoids generated through the activity of 11β-HSD1 decrease insulin and glucagon secretion, acting perhaps in an autocrine and a paracrine manner. Selective 11β-HSD1 inhibitors that enhance peripheral insulin sensitivity and potentially increase insulin secretion could therefore be a valuable tool in the treatment of patients with type 2 diabetes.
Abbreviations
- GR:
-
glucocorticoid receptor
- GSIS:
-
glucose-stimulated insulin secretion
- H6PDH:
-
hexose-6-phosphate dehydrogenase
- H6PDH-KO:
-
mice with a targeted inactivation of H6pd
- 11β-HSD1:
-
11β-hydroxysteroid dehydrogenase type 1
- 11β-HSD1-KO:
-
11β-Hsd1-null mice
- WT:
-
wild-type
References
Hanson RW, Garber AJ (1972) Phosphoenolpyruvate carboxykinase. 1. Its role in gluconeogenesis. Am J Clin Nutr 25:1010–1021
Voice MW, Webster AP, Burchell A (1997) The in vivo regulation of liver and kidney glucose-6-phosphatase by dexamethasone. Horm Metab Res 29:97–100
Larsson H, Ahren B (1996) Short-term dexamethasone treatment increases plasma leptin independently of changes in insulin sensitivity in healthy women. J Clin Endocrinol Metab 81:4428–4432
Davani B, Khan A, Hult M et al (2000) Type 1 11 beta-hydroxysteroid dehydrogenase mediates glucocorticoid activation and insulin release in pancreatic islets. J Biol Chem 275:34841–34844
Lambillotte C, Gilon P, Henquin JC (1997) Direct glucocorticoid inhibition of insulin secretion - An in vitro study of dexamethasone effects in mouse islets. J Clin Invest 99:414–423
Ortsater H, Alberts P, Warpman U, Engblom LOM, Abrahmsen L, Bergsten P (2005) Regulation of 11 beta-hydroxysteroid dehydrogenase type 1 and glucose-stimulated insulin secretion in pancreatic islets of Langerhans. Diabetes Metab Res Rev 21:359–366
Fischer B, Rausch U, Wollny P, Westphal H, Seitz J, Aumuller G (1990) Immunohistochemical localization of the glucocorticoid receptor in pancreatic beta-cells of the rat. Endocrinology 126:2635–2641
Jeong IK, Oh SH, Kim BJ et al (2001) The effects of dexamethasone on insulin release and biosynthesis are dependent on the dose and duration of treatment. Diabetes Res Clin Pract 51:163–171
Billaudel B, Sutter BCJ (1979) Direct effect of corticosterone upon insulin-secretion studied by 3 different techniques. Horm Metab Res 11:555–560
Barseghian G, Levine R (1980) Effect of corticosterone on insulin and glucagon-secretion by the isolated perfused rat pancreas. Endocrinology 106:547–552
Pierluissi J, Navas FO, Ashcroft SJH (1986) Effect of adrenal-steroids on insulin release from cultured rat islets of Langerhans. Diabetologia 29:119–121
Brunstedt J, Nielsen JH (1981) Direct long-term effect of hydrocortisone on insulin and glucagon-release from mouse pancreatic-islets in tissue-culture. Acta Endocrinol (Copenh) 96:498–504
Kawai A, Kuzuya N (1977) Role of glucocorticoid in glucose-induced insulin-secretion. Horm Metab Res 9:361–365
Delaunay F, Khan A, Cintra A et al (1997) Pancreatic beta cells are important targets for the diabetogenic effects of glucocorticoids. J Clin Invest 100:2094–2098
Bujalska IJ, Kumar S, Stewart PM (1997) Does central obesity reflect “Cushing’s disease of the omentum”? Lancet 349:1210–1213
Stewart PM (1996) 11 beta-hydroxysteroid dehydrogenase: implications for clinical medicine. Clin Endocrinol 44:493–499
Bujalska IJ, Draper N, Michailidou Z et al (2005) Hexose-6-phosphate dehydrogenase confers oxo-reductase activity upon 11 beta-hydroxysteroid dehydrogenase type 1. J Mol Endocrinol 34:675–684
Paterson JM, Morton NM, Fievet C et al (2004) Metabolic syndrome without obesity: hepatic overexpression of 11beta-hydroxysteroid dehydrogenase type 1 in transgenic mice. Proc Natl Acad Sci USA 101:7088–7093
Masuzaki H, Paterson J, Shinyama H et al (2001) A transgenic model of visceral obesity and the metabolic syndrome. Science 294:2166–2170
Masuzaki H, Yamamoto H, Kenyon CJ et al (2003) Transgenic amplification of glucocorticoid action in adipose tissue causes high blood pressure in mice. J Clin Invest 112:83–90
Kotelevtsev Y, Holmes MC, Burchell A et al (1997) 11 beta-hydroxysteroid dehydrogenase type 1 knockout mice show attenuated glucocorticoid-inducible responses and resist hyperglycemia on obesity or stress. Proc Natl Acad Sci USA 94:14924–14929
Lavery GG, Walker EA, Draper N et al (2006) Hexose-6-phosphate dehydrogenase knock-out mice lack 11 beta-hydroxysteroid dehydrogenase type 1-mediated glucocorticoid generation. J Biol Chem 281:6546–6551
Ricketts ML, Verhaeg JM, Bujalska I, Howie AJ, Rainey WE, Stewart PM (1998) Immunohistochemical localization of type 1 11 beta-hydroxysteroid dehydrogenase in human tissues. J Clin Endocrinol Metab 83:1325–1335
Bujalska IJ, Gathercole LL, Tomlinson JW et al (2008) A novel selective 11beta-hydroxysteroid dehydrogenase type 1 inhibitor prevents human adipogenesis. J Endocrinol 197:297–307
Brereton PS, van Driel RR, Suhaimi F, Koyama K, Dilley R, Krozowski Z (2001) Light and electron microscopy localization of the 11beta-hydroxysteroid dehydrogenase type I enzyme in the rat. Endocrinology 142:1644–1651
Gremlich S, Roduit R, Thorens B (1997) Dexamethasone induces posttranslational degradation of GLUT2 and inhibition of insulin secretion in isolated pancreatic beta cells - Comparison with the effects of fatty acids. J Biol Chem 272:3216–3222
Khan A, Cao HL, Landau BR (1995) Glucose-6-phosphatase activity in islets from ob/ob and lean mice and the effect of dexamethasone. Endocrinology 136:1934–1938
Khan A, Ostenson CG, Berggren PO, Efendic S (1992) Glucocorticoid increases glucose cycling and inhibits insulin release in pancreatic-islets of ob/ob mice. Am J Physiol 263:E663–E666
Jamal H, Jones PM, Byrne J et al (1991) Peptide contents of neuropeptide-Y, vasoactive intestinal polypeptide, and beta-calcitonin gene-related peptide and their messenger ribonucleic-acids after dexamethasone treatment in the isolated rat islets of Langerhans. Endocrinology 129:3372–3380
Hamamdzic D, Duzic E, Sherlock JD, Lanier SM (1995) Regulation of alpha(2)-adrenergic receptor expression and signaling in pancreatic beta-cells. Am J Physiol 32:E162–E171
Fernandez-Mejia C, Medina-Martinez O, Martinez-Perez L, Goodman PA (1999) The human insulin gene contains multiple transcriptional elements that respond to glucocorticoids. Pancreas 18:336–341
Wise JK, Hendler R, Felig P (1973) Influence of glucocorticoids on glucagon secretion and plasma amino-acid concentrations in Man. J Clin Invest 52:2774–2782
Marco J, Calle C, Hedo JA, Villanueva ML (1976) Enhanced glucagon-secretion by pancreatic-islets from prednisolone-treated mice. Diabetologia 12:307–311
Abrahamsen N, Nishimura E (1995) Regulation of glucagon and glucagon-like peptide-1 receptor messenger ribonucleic acid expression in cultured rat pancreatic islets by glucose, cyclic adenosine 3′,5′-monophosphate, and glucocorticoids. Endocrinology 136:1572–1578
Song IH, Buttgereit F (2006) Non-genomic glucocorticoid effects to provide the basis for new drug developments. Mol Cell Endocrinol 246:142–146
Gromada J, Ding WG, Barg S, Renstrom E, Rorsman P (1997) Multisite regulation of insulin secretion by cAMP-increasing agonists: evidence that glucagon-like peptide 1 and glucagon act via distinct receptors. Pflugers Arch 434:515–524
Sorensen H, Winzell MS, Brand CL et al (2006) Glucagon receptor knockout mice display increased insulin sensitivity and impaired beta-cell function. Diabetes 55:3463–3469
Huypens P, Ling Z, Pipeleers D, Schuit F (2000) Glucagon receptors on human islet cells contribute to glucose competence of insulin release. Diabetologia 43:1012–1019
Alberts P, Engblom L, Edling N et al (2002) Selective inhibition of 11beta-hydroxysteroid dehydrogenase type 1 decreases blood glucose concentrations in hyperglycaemic mice. Diabetologia 45:1528–1532
Kershaw EE, Morton NM, Dhillon H, Ramage L, Seck JR, Flier JS (2005) Adipocyte-specific glucocorticoid inactivation protects against diet-induced obesity. Diabetes 54:1023–1031
Bhat BG, Hosea N, Fanjul A et al (2008) Demonstration of proof of mechanism and pharmacokinetics and pharmacodynamic relationship with 4′-cyano-biphenyl-4-sulfonic acid (6-amino-pyridin-2-yl)-amide (PF-915275), an inhibitor of 11 -hydroxysteroid dehydrogenase type 1, in cynomolgus monkeys. J Pharmacol Exp Ther 324:299–305
Alberts P, Nilsson C, Selen G et al (2003) Selective inhibition of 11β-hydroxysteroid dehydrogenase type 1 improves hepatic insulin sensitivity in hyperglycemic mice strains. Endocrinology 144:4755–4762
Hermanowski-Vosatka A, Balkovec JM, Cheng K et al (2005) 11 beta-HSD1 inhibition ameliorates metabolic syndrome and prevents progression of atherosclerosis in mice. J Exp Med 202:517–527
Acknowledgements
This work was supported by Wellcome Trust programme grant 066357, project grant 074088 (to P. M. Stewart and E. A. Walker) and Clinical Scientist Fellowship 075322 (to J. W. Tomlinson). The authors wish to thank C. Shaikh at the Birmingham Midland Eye Centre for preparation of slides and D. Smith of Astra Zeneca for assistance with islet isolation.
Duality of interest
P. M. Stewart has received consultancy fees and an investigator-initiated research grant from Pfizer. All other authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Swali, A., Walker, E.A., Lavery, G.G. et al. 11β-Hydroxysteroid dehydrogenase type 1 regulates insulin and glucagon secretion in pancreatic islets. Diabetologia 51, 2003–2011 (2008). https://doi.org/10.1007/s00125-008-1137-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-008-1137-2