Abstract
Aims/hypothesis
Glycogen synthase kinase-3 (GSK3) has been implicated in the pathophysiology of several prevalent diseases, including diabetes. However, despite recent progress in our understanding of the role of GSK3 in the regulation of glucose metabolism in peripheral tissues, the involvement of GSK3 in islet beta cell growth and function in vivo is unknown. We therefore sought to determine whether over-activation of GSK3β would lead to alterations in islet beta cell mass and/or function.
Methods
Transgenic mice overexpressing a constitutively active form of human GSK3β (S9A) under the control of the rat insulin promoter (RIP-GSK3βCA) were created. Studies using mouse insulinoma cells (MIN6) were conducted to investigate the regulation of GSK3β activity and its impact on pancreas/duodenum homeobox protein-1 (PDX-1) levels.
Results
We demonstrated that phosphorylation of GSK3β was decreased, indicating increased GSK3β activity in two animal models of diabetes, Lepr −/− mice and Ins2 Akita/+ mice. In MIN6 cells, the activity of GSK3β was regulated by glucose, in a fashion largely dependent on phosphatidylinositol 3-kinase. RIP-GSK3βCA transgenic mice showed impaired glucose tolerance after 5 months of age. Histological studies revealed that transgenic mice had decreased beta cell mass and decreased beta cell proliferation, with a 50% decrease (p < 0.05) in the level of PDX-1.
Conclusions/interpretation
We showed direct evidence that GSK3β activity is associated with beta cell failure in diabetic mouse models and that its overactivation resulted in decreased pancreatic beta cell proliferation and mass. GSK3 modulates PDX-1 stability in both cultured insulinoma cells and islets in vivo. These results may ultimately facilitate the development of potential therapeutic interventions targeting type 2 diabetes and/or islet transplantation.
Similar content being viewed by others
Introduction
The prevalence of obesity and diabetes mellitus is increasing with alarming rapidity [1]. Insulin resistance and beta cell failure are the hallmarks of type 2 diabetes [2]. The importance of insulin receptor (InsR) signalling in the development of insulin resistance and beta cell failure has been shown by studies of genetic mouse models deficient in InsR and its downstream signalling components [3]. Knockout of Irs2 in mice resulted in overt diabetes due to increased insulin resistance in peripheral tissues and a concurrent loss of pancreatic beta cells [4]. Recent studies of mouse models lacking functional receptors for both insulin and IGF-1 only in beta cells (βDKO) have provided compelling genetic evidence that InsR signalling is critical for beta cell growth and function [5]. Stimulation of InsR signalling leads to activation of phosphatidylinositol 3-kinase (PI3K) and protein kinase B/Akt, which promote cell proliferation, growth and survival in various tissue types [6]. βDKO mice developed diabetes 3 weeks after birth due to reduced beta cell mass with reduced level of phosphorylated Akt, indicating decreased Akt activity [5]. Conversely, overexpression of Akt in beta cells resulted in a marked increase in beta cell mass and resistance to streptozotocin-induced diabetes [7]. While it is known that the more proximal components of insulin signalling are critical for the regulation of beta cell mass and function, less is known about the downstream components that relay specific signals controlling beta cell mass and function.
Glycogen synthase kinase-3 (GSK3) was the first substrate shown to be phosphorylated by Akt [8]. GSK3 has two isoforms, GSK3α and GSK3β, both of which are serine/threonine protein kinases whose activities are inhibited by Akt-mediated phosphorylation. An increasing body of literature has demonstrated the diverse functions of GSK3 in the regulation of cellular structure, mobility, proliferation, apoptosis and metabolism [9, 10]. Originally identified as a modulator of glycogen metabolism [11], GSK3 shows enhanced activity in insulin-resistant states [12, 13] and has been proposed as a potential therapeutic target for the treatment of diabetes [14–16]. GSK3 expression and activity were shown to be increased in skeletal muscle samples from patients with type 2 diabetes [13]. In diabetic or insulin-resistant animal models, two studies have reported increased GSK3 activity in the epididymal fat tissue of mice on a high-fat diet and db/db mice [12, 17]. Although mice with knock-ins of constitutively active GSK3α and GSK3β showed no major metabolic phenotypes [18], transgenic mice with overexpression of GSK3β in skeletal muscle became glucose-intolerant [19]. More importantly, administration of GSK3 inhibitors to experimental animals has been shown to improve glucose tolerance and reduce insulin resistance [20–23].
Despite recent progress in our understanding of the role of GSK3 in the regulation of glucose metabolism in peripheral tissues, there have been virtually no reports of the in vivo phosphorylation state of GSK3 in pancreatic islets of diabetic animal models and of how it could regulate beta cell growth and function. The purpose of the current studies was to determine the level of phosphorylated GSK3 in pancreatic islets of diabetic animal models and to assess whether over-activation of GSK3β would lead to alterations in islet beta cell mass and/or function. The results of our studies indicate that GSK3 activity can contribute to beta cell dysfunction, possibly enabling identification of a new therapeutic target geared to enhancing islet beta cell growth and preventing type 2 diabetes.
Methods
Generation of transgenic mice
To create transgenic mice overexpressing a constitutively active form of human GSK3β(S9A) under the rat insulin promoter (RIP-GSK3βCA), the rat insulin-1 promoter in a pBS-KS vector was fused with human GSK3β(S9A) cDNA (provided by M. Birnbaum, Department of Medicine, University of Pennsylvania, PA, USA). The transgene was linearised with PvuI, purified and microinjected into fertilised eggs of B6/CBA mice by the Washington University Mouse Genetics Core Facility. Transgenic mice were identified by PCR genotyping from tail DNA. Two transgenic founders were established and crossed to wild-type C57BL/6J mice (Jackson Laboratories, Bar Harbor, Maine, USA). Ins2 Akita mice and Lepr −/− mice were obtained from Jackson Laboratories and analysed at 3 months of age with average fed glucose above 33.3 mmol/l. All animal procedures were approved by the Washington University Animal Studies Committee.
Islet immunohistological and morphometric analysis
Immunohistological and morphometric analysis was as previously described [7]. Antibodies used in this study were as follows: insulin and Ki67 (Dako North America, Carpinteria, CA, USA), phospho-GSK3β (Cell Signaling Technology, Danvers, MA, USA), haemagglutinin (Covance, Emeryville, CA, USA). Beta cell mass was quantified using NIH ImageJ software version 1.37n [24].
Fed and fasted glucose and insulin measurements
Fed and fasted glucose were measured as previously described [7]. Insulin levels were determined on 10 μl aliquots using rat insulin ELISA kits with mouse insulin standards (Alpco Diagnostics, Salem, NH USA). Total pancreatic insulin content was measured after acid-ethanol extraction by radioimmunoassay at the Washington University RIA Core.
Intraperitoneal glucose tolerance tests
After mice were fasted overnight (18–20 h), an intraperitoneal glucose tolerance test (IPGTT), consisting of 50% dextrose (2 g/kg body weight) injected intraperitoneally, was performed. Blood was collected from the tail vein at 0, 30, 60 and 120 min after injection for glucose measurements. Plasma for insulin measurements was also collected at 0 and 10 min after glucose injection and submitted to the Washington University RIA Core.
Glucose-stimulated insulin secretion and insulin content from isolated islets
Islets were isolated by collagenase distension/digestion of the pancreas as previously described [25]. Handpicked islets were cultured overnight in RPMI media. Islets were then preincubated for 1 h at 37°C in KRB buffer containing 2 mmol/l glucose. Islets of similar size were handpicked into groups of ten islets in triplicate and incubated for 1 h at 37°C with 1 ml KRB buffer containing either 2 or 20 mmol/l glucose. The supernatant fractions were stored at −20°C prior to insulin measurements. After insulin secretion experiments, islets were washed twice with PBS and extracted with acid-ethanol overnight at 4°C. Insulin levels were measured by radioimmunassay by the Washington University RIA Core.
Assessment of islet beta cell proliferation and apoptosis
Beta cell replication was determined by immunostaining for Ki67 on pancreatic sections. Rate of proliferation was measured by percentage of Ki67-positive cells per total number of insulin-positive cells (about 1,000 cells were counted per animal, four animals per genotype). Cleaved caspase-3 staining (Cell Signaling Technology) and TUNEL (Chemicon, Temecula, CA, USA) were used to measure rate of apoptosis.
MIN6 cell culture and western blotting
MIN6 cells were maintained in DMEM [26]. Cells with passage numbers of less than 35 were used in these experiments. Protein was extracted with a cell lysis buffer (Cell Signalling). Protein samples (20–40 μg) were separated by standard SDS-PAGE gels, transferred to polyvinylidene fluoride membranes and then immunoblotted. Antibodies used in this study were as follows: anti-phospho-Ser473 Akt, anti-phospho-GSK3, anti-GSK3β (Cell Signaling Technology), anti-phospho-glycogen synthase (Biosource, Camarillo, CA, USA), anti-beta catenin (BD Transduction Laboratories, San Jose, CA, USA), anti-cyclin D1 (Chemicon, Temecula, CA, USA), anti-IRS-1 (Upstate, Billerica, MA, USA) and anti-tubulin (Sigma, St Louis, MO, USA).
Statistical analysis
Unless otherwise indicated, all values are expressed as mean ± SEM and statistical analyses were carried out using an unpaired Student’s t test. Differences were considered to be statistically significant when p < 0.05.
Results
Acute inhibition of GSK3β activity by glucose-induced insulin signalling in mouse insulinoma (MIN6) cells
Activation of InsR stimulates a signalling cascade leading to phosphorylation of GSK3, which decreases its activity [8]. Previous pharmacological experiments have shown that IGF-1 induced rapid phosphorylation of GSK3 in insulinoma cells [27]. Our preceding studies documented that glucose activated Akt through an autocrine/paracrine effect of insulin with subsequent activation of the PI3K pathway [26, 28]. To extend these observations, we sought to test whether changes in glucose could regulate GSK3β activity in beta cells. MIN6 cells were cultured in reduced glucose (5 mmol/l) overnight, then treated with 25 mmol/l glucose for 45 min. Consistent with previous studies [26, 28], phosphorylated Akt was increased by high glucose (Fig. 1a). Western blotting showed increased levels of phosphorylated GSK3β after high glucose treatment (Fig. 1a,b). Phosphorylated GSK3β is the inhibited form of the enzyme. In contrast, glucose-stimulated phosphorylation of Akt and GSK3 was diminished by co-treatment with LY294002, a PI3K inhibitor known to reduce Akt activity (Fig. 1a,b). To test whether the observed glucose-induced changes in the phosphorylation state of GSK3 resulted in changes in activity, samples were blotted with an antibody recognising phospho-glycogen synthase (pGS), a direct target of GSK3. Figure 1a,c shows decreased levels of pGS after high glucose treatment, a decrease restored by co-treatment with LY294002. Taken together, these experiments demonstrate that glucose-induced InsR signalling and GSK3 activity could be regulated by glucose in beta cells and that this regulation is mediated largely through glucose-induced activation of PI3K, presumably via glucose effects on insulin secretion [26, 28].
Regulation of GSK3β by glucose in MIN6 cells and its decreased phosphorylation in diabetic islets. a MIN6 cells were treated overnight with 5 mmol/l glucose in DMEM medium with 2% serum (control [Con]) and then treated with 25 mmol/l glucose same medium for 45 min (G45′) with or without PI3K inhibitor LY294002 (G45’ + LY). Proteins from whole cell lysates were separated by SDS-PAGE and western blot analyses performed using the antibodies as labelled. Quantification of relative GSK3β phosphorylation (b) and glycogen synthase phosphorylation (c) compared with total GSK3 level. The results are the means ± SEM of three independent experiments. *p < 0.002, **p < 0.05. d Immunohistochemical analyses of phospho-GSK3β on representative pancreatic sections from Lepr −/− mice, Ins2 Akita/+ mice and their respective controls. Anti-phospho-GSK3β antibody was labelled with Cy3 (red) and anti-insulin antibody was labelled with FITC (green). Note the markedly reduced abundance of pGSK3 in diabetic Lepr −/− mice and Ins2 Akita/+ mice
Chronic activation of GSK3β in islets of diabetic mice with impaired insulin signalling
In animal models with reduced beta cell insulin signalling, either through reduction in InsR [5] or IRSs [4], reduction in beta cell mass and diabetes develops with age. Reduced insulin signalling in beta cells would be anticipated to lead to activation of the negatively regulated downstream targets of insulin/PI3K/Akt signalling, forkhead box protein O1A (FOXO1) and GSK3. While there is evidence for increased FOXO1 activity contributing to beta cell loss in animal models [29], the activity of GSK3 under conditions of impaired insulin signalling has not been studied. As insulin signalling results in suppression of GSK3β activity through Akt phosphorylation, we examined the level of phosphorylated GSK3β as a measure of activity in two diabetic animal models, Lepr −/− mice and Ins2 Akita/+ mice. As shown in Fig. 1d, the levels of phosphorylated GSK3β were markedly diminished in islets of Lepr −/− mice and Ins2 Akita/+ mice compared with those from control animals, suggesting increased GSK3β activity in these diabetic models. These results led to the hypothesis that a transgenic model of overexpression of GSK3β in beta cells would result in beta cell dysfunction and glucose intolerance.
Overexpression of a constitutively active form of GSK3β in pancreatic beta cells
The regulation of GSK3β by glucose/InsR/PI3K/Akt activation in cultured beta cells and its decreased phosphorylation in islets of diabetic mice suggest that GSK3β may play an important role in beta cell growth or function and contribute to the diabetic phenotype seen in Lepr −/− mice and Ins2 Akita/+mice. To test the hypothesis that over-activation of GSK3β would result in beta cell dysfunction, we created transgenic mice with overexpression of a constitutively active form of human GSK3β in pancreatic beta cells. Increased GSK activity was achieved by using a serine 9 to alanine mutant. This mutant renders GSK3β unable to be phosphorylated by Akt and thus refractory to insulin inhibition [11]. We utilised this constitutively active form of human GSK3β containing a haemagglutinin tag, subcloned downstream of the rat insulin promoter, to drive transgenic expression in islet beta cells (RIP-GSK3βCA). Expression of the transgene was confirmed by western blotting of haemagglutinin (Fig. 2a). The level of total GSK3β was also assessed by western blotting using an antibody that recognises both the endogenous wild-type protein and the mutant human GSK3β protein. As shown in Fig. 2a, the level of total GSK3β was increased about two to threefold in the transgenic islets. No expression of the transgene was detected in liver, skeletal muscles or brain tissues (data not shown). By immunohistochemistry, most insulin-positive beta cells showed co-expression of the transgene, but some beta cells within the same islet did not express the transgene (Fig. 2b). This type of mosaic expression has been reported in other transgenic animal models [30, 31].
Overexpression of a constitutively active form of GSK3β in pancreatic beta cells. a Protein samples from lysates of isolated islets with indicated genotypes were separated by SDS-PAGE, and western blot analyses performed using the antibodies as labelled. TG, transgenic; WT, wild-type. b Immunohistochemical analysis of the transgene on representative pancreatic sections from both WT and TG mice. Anti-HA antibody was labelled with Cy3 (red) and anti-insulin antibody was labelled with FITC (green), and images merged as shown. Strong stains of vascular structures were probably due to the use of mouse-origin antibody directed against HA
RIP-GSK3βCA mice had normal growth and metabolism during early adult life. Body weight was measured weekly beginning on postnatal day 21. No significant body weight differences between RIP-GSK3βCA and control mice were observed (data not shown). Glucose and insulin levels and the various tolerance tests were performed upon fasted mice (16 h overnight fast) or random-fed mice at 6 weeks and 3 months after birth. Our studies indicated that these transgenic mice had normal glucose metabolism during these periods (data not shown).
RIP-GSK3βCA male mice showed impaired glucose tolerance and decreased beta cell mass at 5 months
IPGTTs performed in adult mice (5 months old) showed impaired glucose tolerance in male RIP-GSK3βCA mice compared with wild-type littermates (Fig. 3a). We measured insulin levels at 0 and 10 min time points during the IPGTTs. Consistent with their impaired glucose tolerance, plasma insulin levels at 2, 5 and 10 min after glucose injection were lower in male RIP-GSK3βCA mice than in their non-transgenic siblings, although these differences were not statistically significant (Fig. 3b and data not shown). No difference was observed in IPGTT on female mice (data not shown). The results of these studies demonstrate that constitutive activation of GSK3β in islet beta cells resulted in impaired glucose tolerance in male mice, suggesting defects in either beta cell mass and/or insulin secretion.
RIP-GSK3βCA male mice showed impaired glucose tolerance and decreased beta cell mass at 5 months of age. a IPGTT in male transgenic mice (black squares) compared with control animals (white diamonds). Following an 18 h fast, 2 g of 50% glucose (wt/vol) per kg body weight was injected intraperitoneally and blood glucose values were assessed at 0, 30, 60, and 120 min after injection. Wild-type (WT), n = 5; transgenic (TG), n = 5; *p < 0.05. b Plasma insulin levels in male TG mice (grey bars) compared with controls (white bars) at 0 and 10 min time points in IPGTT (n = 4–7). c Glucose-stimulated insulin secretion (pmol ml−1 h−1) of isolated islets from TG (black bars) and control (white bars) mice with low glucose (LG; 5 mmol/l) and high glucose (HG; 25 mmol/l) concentrations. The secretion assays were performed on triplicate groups of ten islets for each mouse, with three mice for each genotype. d Whole pancreatic insulin content (pmol/mg) of TG and control mice (three mice for each genotype). e Beta cell mass in 5-month-old TG male mice compared with controls. WT, n = 4; TG, n = 4; *p < 0.05. f Rate of beta cell proliferation as measured by the percentage of Ki67+/insulin+cells. WT, n = 4; TG, n = 4; *p < 0.05. All results are expressed as mean ± SEM
To test whether insulin secretion was impaired in RIP-GSK3βCA pancreases in response to high glucose, we did glucose-stimulated insulin secretion assays on islets isolated from both RIP-GSK3βCA and control mice. No difference was observed between these two groups either in low or high glucose conditions (Fig. 3c). The difference in whole pancreatic insulin content was also not statistically significant, although in transgenic islets it was approximately 20% lower (Fig. 3d). Histological study revealed that RIP-GSK3βCA mice had a ~35% decrease in beta cell mass (p = 0.025) compared with that of wild-type control animals (Fig. 3e). Given that the reduction in islet beta cell mass was greater than the reduction in insulin content, we considered that the rate of insulin synthesis per islet may have been increased. However, measurement of insulin content in isolated islets revealed no significant difference (wild-type 1.2 ± 0.5 pmol/islet vs transgenic 1.0 ± 0.5 pmol/islet, p > 0.05). This suggested that the apparent decrease in insulin content was accounted for by decreased mass rather than an effect of GSK3β on insulin synthesis. Assessment of the rate of beta cell proliferation showed a ~25% decrease in the percentage of Ki67-positive cells (p = 0.010) (Fig. 3f). No difference was observed in the rate of beta cell apoptosis, measured by cleaved-caspase-3 and TUNEL assay, between the transgenic mice and littermate controls (data not shown). These studies indicate that constitutive activation of GSK3β in pancreatic beta cells impairs islet beta cell proliferation and subsequently beta cell mass.
GSK3β modulates PDX-1 stability
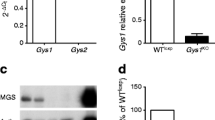
A recent study revealed that GSK3β could phosphorylate and accelerate pancreas/duodenum homeobox protein-1 (PDX-1) protein degradation in cultured insulinoma cells [32]. We thus sought to determine whether the level of total PDX-1 protein was decreased in the islets of our RIP-GSK3βCA transgenic mice. Immunoblot analysis of islet protein from RIP-GSK3βCA transgenic mice showed an increase in GSK3 activity, evidenced by increased levels of pGS (Fig. 4a). Interestingly, transgenic islets showed an approximately 50~60% decrease in PDX-1 protein level compared with that of wild-type mice (Fig. 4a,b). This was confirmed by immunoblotting for PDX-1 protein in islets from three additional transgenic mice. Islet proteins other than PDX-1 that might be involved in regulation of beta cell proliferation were examined, as shown in Fig. 4c. GSK3 activity was able to potentially regulate beta catenin, but this protein was not altered in islets of RIP-GSK3βCA transgenic mice. Additionally levels of cyclin D1 and IRS-1 were not altered, while an apparent reduction in the levels of IRS2 in islets of RIP-GSK3βCA transgenic mice was observed that could have contributed to the reduction in PDX-1 levels.
GSK3β modulates PDX-1 stability. a Protein samples from lysates of isolated islets with indicated genotypes (WT, wild-type; TG, transgenic) were separated by SDS-PAGE and western blot analyses were performed using the antibodies as labelled. Islet protein from WT mice (n = 4) and TG mice (n = 5) was blotted and quantified (b); *p < 0.05. c Western blotting analyses of several potential GSK3 targets, using isolated islets from both WT and TG mice. d MIN6 cells were treated with cycloheximide (25 μg/ml) for 4 h to inhibit protein synthesis. Protein samples with NaCl (Na; 40 mmol/l), LiCl (Li; 40 mmol/l) or LY294002 (LY; 50 μmol/l) co-treatment were blotted with antibodies as labelled. e Quantification of relative PDX-1 and (f) pGS levels compared with tubulin as shown (d). Results are the mean ± SEM of three independent experiments. *p < 0.05, † p < 0.02
To further assess the molecular mechanisms that might account for reduced PDX-1 protein level in RIP-GSK3βCA mice, we sought to confirm previous results implicating GSK3 post-translational effects on PDX-1. MIN6 cells were co-treated with cycloheximide to inhibit protein synthesis and observed 4 h after the following treatments. Application of LY294002, a PI3K inhibitor that mimics decreased insulin signalling with GSK3 activation, resulted in a marked decrease in PDX-1 protein compared with that in cells with no treatment (Fig. 4d,e). To specifically target GSK3, cells were treated with lithium, a well-known GSK3 inhibitor. Treatment with lithium resulted in a ~30% increase in total levels of PDX-1, along with a more than 50% reduction in GSK3 activity as shown by the level of pGS (Fig. 4d,f). Treatment with sodium as a control for lithium did not show any difference in either pGS or PDX-1 levels (Fig. 4d). Thus in summary the modulation of PDX-1 protein level by GSK3β activity provided a possible mechanism by which GSK3β overactivity in the RIP-GSK3βCA transgenic mice resulted in altered pancreatic beta cell growth and function.
Discussion
While it is clear that insulin signalling is critical for maintaining normal beta cell function in the adult mouse and that impaired insulin signalling leads to islet dysfunction, its mediators have not been fully assessed. GSK3 is a well known negatively regulated target of the InsR/PI3K/Akt pathway in many tissues, a topic that has been reviewed [9, 10], yet the hypothesis that impaired insulin signalling and enhanced GSK3 activity result in beta cell dysfunction has not been explored. The current studies report three novel and potentially important observations relevant to InsR/Akt/GSK3 signalling in pancreatic islet beta cells. First is the novel observation that in cultured beta cells GSK3 activity, as shown by phosphorylation of its direct target glycogen synthase, is regulated by changing levels of glucose and that in diabetic islets phosphorylation of GSK3 is decreased, indicating increased activity. Second, overactivation of GSK3 in pancreatic beta cells resulted in glucose intolerance in male mice after 5 months of age with reduced beta cell mass and decreased beta cell proliferation. Third, these results illustrate in an in vivo model that GSK3β overexpression results in reduced levels of PDX-1 protein, while in vitro results further confirmed the role of GSK3 in regulating PDX-1 protein stability. These results thus highlight a new mechanism, whereby signalling through the InsR/Akt/GSK3 pathway regulates beta cell growth; they also provide an explanation for the beta cell dysfunction associated with impaired insulin signalling leading to beta cell failure and diabetes.
Insulin receptor signalling has been implicated in pancreatic beta cell growth, function and survival [3]. Our observation of increased GSK3 activity in two of the well-studied diabetic mouse models suggests a possible mechanism for the reduced islet beta cell mass observed in these animals. Additionally, the current results suggest that the decrease in islet beta cell mass and the resultant diabetic phenotype observed in mouse models with deficiency in receptors for both insulin and IGF-1 (βDKO) or the IRS2 may be related to enhanced GSK3 activity in beta cells. Of course, GSK3 may not be the only mediator of this process, as other distal components of the InsR signalling pathway, e.g. the transcription factor FOXO1, have also been implicated in beta cell growth and function. FOXO1 haploinsufficiency reverses beta cell failure in Irs2 −/− mice through partial restoration of beta cell proliferation and Pdx1 expression [29]. Overexpression of a constitutively nuclear Foxo1 in liver and pancreas prevented beta cell hyperplasia in two animal models [33]. Taken together, these studies highlight the importance of InsR/Akt signalling in maintenance of beta cell growth and function, with two of the direct Akt targets, both GSK3 and FOXO1, contributing to these complex regulations.
The function of GSK3 in pancreatic beta cells may be more related to regulation of cell survival and proliferation than to its effects on carbohydrate metabolism seen in other tissues previously studied. In islet beta cells, previous studies from our group showed siRNA knock-down of GSK3β protected MIN6 cells from endoplasmic reticulum (ER)-stress-induced apoptosis [34]. It has also been shown that inhibition of GSK3 protected beta cells from NEFA-induced apoptosis and this inhibition was also associated with increased beta cell proliferation in primary islets [35]. These observations, along with the results of the current study, thus indicate a predominant role of GSK3 in beta cell proliferation and survival as opposed to an effect on glucose metabolism. The mild glucose intolerance phenotype of transgenic RIP-GSK3βCA mice with a moderate decrease in beta cell mass suggests that additional defect(s) in insulin secretion are possible.
The results of the current studies suggest that a likely mechanism by which GSK3 regulates beta cell proliferation is through destabilisation of PDX-1 protein. GSK3 has been shown to phosphorylate PDX-1 leading to its proteasomal degradation in MIN6 cells [32]. Results of our current studies confirmed this observation not only in cultured insulinoma cells (Fig. 4d,e) but also in RIP-GSK3βCA mice, an in vivo mouse model with GSK3β overexpression and PDX-1 levels reduced by 50 to 60% (Fig. 4a,b). The possibility that PDX-1 levels are critical for maintaining beta cell mass was observed in the Irs2 knockout mouse, where PDX-1 levels were reduced to this magnitude, along with reduction of beta cell proliferation and mass [29]. Importantly, crossing these globally IRS2-deficient mice with mice expressing Pdx-1 specifically in beta cells maintained beta cell mass and rescued the diabetes phenotype [36]. Interestingly, FOXO1, another target of InsR/Akt signalling, has also been shown to regulate PDX-1 levels, but apparently through its effects on suppression of transcription [29]. Thus in beta cells with impaired insulin signalling increased GSK3 as well as increased FOXO1 activity may converge to suppress PDX-1 levels by different mechanisms. In addition to the modulation of PDX-1 stability, GSK3 could also potentially regulate beta cell proliferation through phosphorylation and degradation of cyclin D1 and/or p27. GSK3 has been shown to be an excellent in vitro kinase for cyclin D1 and p27 and also to regulate their stability [37, 38]. However, we did not detect a significant change in the levels of cyclin D1 or p27 in the transgenic islets (Fig. 4c and data not shown).
In transgenic mice, we noted a 20% reduction in pancreatic insulin content (NS). There is good reason to suspect the rate of insulin synthesis per beta cell is reduced, as PDX-1, an important transcription factor for insulin gene transcription, was also reduced in transgenic mice. Additionally, GSK3 could potentially regulate eukaryotic initiation factor 2B activity [39]. Alternatively ER stress could reduce insulin synthesis; indeed, our previous studies have shown that GSK3 activity was enhanced by ER stress [34]. However, GSK3 activation appeared to be downstream of ER stress, so any reduction of insulin synthesis that might be a consequence of increased GSK3 activity is unlikely to be the effect of GSK3 on ER stress.
The results of the current study suggest the possibility of GSK3β inhibition as a means of preserving beta cell mass. Because of the involvement of beta cell failure in common forms of diabetes, these observations have potential clinical implications. Interestingly, the recently approved diabetes treatment Exendin-4 has been shown to promote beta cell proliferation and survival through activation of the PI3K/Akt pathway, see review [40]. FOXO1 was shown to mediate this effect by activating PDX-1 [41]. Both the similar regulation of GSK3 by PI3K/Akt activation, and the modulation of PDX-1 stability by GSK3 suggest that GSK3 may serve as an additional mediator of the effects of Exendin-4 on beta cell function.
In conclusion, we showed direct evidence that GSK3β activity is associated with beta cell failure in diabetic mouse models and that its overactivation resulted in decreased pancreatic beta cell proliferation and mass. GSK3 modulates PDX-1 stability in both cultured insulinoma cells and islets in vivo. Further studies will probably identify additional Akt/GSK3β downstream targets responsible for control of beta cell proliferation. Ultimately, our results may facilitate the development of therapeutic interventions targeting type 2 diabetes and/or islet transplantation.
Abbreviations
- ER:
-
endoplasmic reticulum
- FOXO:
-
forkhead box protein O1A
- GSK3:
-
glycogen synthase kinase-3
- InsR:
-
insulin receptor
- IPGTT:
-
intraperitoneal glucose tolerance test
- PDX-1:
-
pancreas/duodenum homeobox protein-1
- pGS:
-
phospho-glycogen synthase
- PI3K:
-
phosphatidylinositol 3-kinase
References
Ford ES, Giles WH, Mokdad AH (2004) Increasing prevalence of the metabolic syndrome among U.S. Adults. Diabetes Care 27:2444–2449
Prentki M, Nolan CJ (2006) Islet beta cell failure in type 2 diabetes. J Clin Invest 116:1802–1812
Biddinger SB, Kahn CR (2006) From mice to men: insights into the insulin resistance syndromes. Annu Rev Physiol 68:123–158
Lee YH, White MF (2004) Insulin receptor substrate proteins and diabetes. Arch Pharm Res 27:361–370
Ueki K, Okada T, Hu J et al (2006) Total insulin and IGF-I resistance in pancreatic beta cells causes overt diabetes. Nat Genet 38:583–588
Woodgett JR (2005) Recent advances in the protein kinase B signaling pathway. Curr Opin Cell Biol 17:150–157
Bernal-Mizrachi E, Wen W, Stahlhut S, Welling CM, Permutt MA (2001) Islet beta cell expression of constitutively active Akt1/PKB alpha induces striking hypertrophy, hyperplasia, and hyperinsulinemia. J Clin Invest 108:1631–1638
Cross DA, Alessi DR, Cohen P, Andjelkovich M, Hemmings BA (1995) Inhibition of glycogen synthase kinase-3 by insulin mediated by protein kinase B. Nature 378:785–789
Doble BW, Woodgett JR (2003) GSK-3: tricks of the trade for a multi-tasking kinase. J Cell Sci 116:1175–1186
Woodgett JR (2001) Judging a protein by more than its name: GSK-3. Sci STKE 2001:RE12
Eldar-Finkelman H, Argast GM, Foord O, Fischer EH, Krebs EG (1996) Expression and characterization of glycogen synthase kinase-3 mutants and their effect on glycogen synthase activity in intact cells. Proc Natl Acad Sci USA 93:10228–10233
Eldar-Finkelman H, Schreyer SA, Shinohara MM, LeBoeuf RC, Krebs EG (1999) Increased glycogen synthase kinase-3 activity in diabetes- and obesity-prone C57BL/6J mice. Diabetes 48:1662–1666
Nikoulina SE, Ciaraldi TP, Mudaliar S, Mohideen P, Carter L, Henry RR (2000) Potential role of glycogen synthase kinase-3 in skeletal muscle insulin resistance of type 2 diabetes. Diabetes 49:263–271
Henriksen EJ, Dokken BB (2006) Role of glycogen synthase kinase-3 in insulin resistance and type 2 diabetes. Curr Drug Targets 7:1435–1441
Wagman AS, Johnson KW, Bussiere DE (2004) Discovery and development of GSK3 inhibitors for the treatment of type 2 diabetes. Curr Pharm Des 10:1105–1137
Kaidanovich O, Eldar-Finkelman H (2002) The role of glycogen synthase kinase-3 in insulin resistance and type 2 diabetes. Expert Opin Ther Targets 6:555–561
Clodfelder-Miller B, De Sarno P, Zmijewska AA, Song L, Jope RS (2005) Physiological and pathological changes in glucose regulate brain Akt and glycogen synthase kinase-3. J Biol Chem 280:39723–39731
McManus EJ, Sakamoto K, Armit LJ et al (2005) Role that phosphorylation of GSK3 plays in insulin and Wnt signalling defined by knockin analysis. Embo J 24:1571–1583
Pearce NJ, Arch JR, Clapham JC et al (2004) Development of glucose intolerance in male transgenic mice overexpressing human glycogen synthase kinase-3beta on a muscle-specific promoter. Metabolism 53:1322–1330
Cline GW, Johnson K, Regittnig W et al (2002) Effects of a novel glycogen synthase kinase-3 inhibitor on insulin-stimulated glucose metabolism in Zucker diabetic fatty (fa/fa) rats. Diabetes 51:2903–2910
Plotkin B, Kaidanovich O, Talior I, Eldar-Finkelman H (2003) Insulin mimetic action of synthetic phosphorylated peptide inhibitors of glycogen synthase kinase-3. J Pharmacol Exp Ther 305:974–980
Rao R, Hao CM, Redha R, Wasserman DH, McGuinness OP, Breyer MD (2007) Glycogen synthase kinase 3 inhibition improves insulin-stimulated glucose metabolism but not hypertension in high-fat-fed C57BL/6J mice. Diabetologia 50:452–460
Ring DB, Johnson KW, Henriksen EJ et al (2003) Selective glycogen synthase kinase 3 inhibitors potentiate insulin activation of glucose transport and utilization in vitro and in vivo. Diabetes 52:588–595
Girish V, Vijayalakshmi A (2004) Affordable image analysis using NIH Image/ImageJ. Indian J Cancer 41:47
Martinez SC, Cras-Meneur C, Bernal-Mizrachi E, Permutt MA (2006) Glucose regulates Foxo1 through insulin receptor signaling in the pancreatic islet β-cell. Diabetes 55:1581–1591
Ohsugi M, Cras-Meneur C, Zhou Y et al (2005) Reduced expression of the insulin receptor in mouse insulinoma (MIN6) cells reveals multiple roles of insulin signaling in gene expression, proliferation, insulin content, and secretion. J Biol Chem 280:4992–5003
Dickson LM, Lingohr MK, McCuaig J et al (2001) Differential activation of protein kinase B and p70(S6)K by glucose and insulin-like growth factor 1 in pancreatic beta-cells (INS-1). J Biol Chem 276:21110–21120
Srinivasan S, Bernal-Mizrachi E, Ohsugi M, Permutt MA (2002) Glucose promotes pancreatic islet beta-cell survival through a PI 3-kinase/Akt-signaling pathway. Am J Physiol Endocrinol Metab 283:E784–E793
Kitamura T, Nakae J, Kitamura Y et al (2002) The forkhead transcription factor Foxo1 links insulin signaling to Pdx1 regulation of pancreatic beta cell growth. J Clin Invest 110:1839–1847
Koster JC, Remedi MS, Flagg TP et al (2002) Hyperinsulinism induced by targeted suppression of beta cell KATP channels. Proc Natl Acad Sci USA 99:16992–16997
Heiser PW, Lau J, Taketo MM, Herrera PL, Hebrok M (2006) Stabilization of beta-catenin impacts pancreas growth. Development 133:2023–2032
Boucher MJ, Selander L, Carlsson L, Edlund H (2006) Phosphorylation marks IPF1/PDX1 protein for degradation by glycogen synthase kinase 3-dependent mechanisms. J Biol Chem 281:6395–6403
Okamoto H, Hribal ML, Lin HV, Bennett WR, Ward A, Accili D (2006) Role of the forkhead protein FoxO1 in beta cell compensation to insulin resistance. J Clin Invest 116:775–782
Srinivasan S, Ohsugi M, Liu Z, Fatrai S, Bernal-Mizrachi E, Permutt MA (2005) Endoplasmic reticulum stress-induced apoptosis is partly mediated by reduced insulin signaling through phosphatidylinositol 3-kinase/Akt and increased glycogen synthase kinase-3beta in mouse insulinoma cells. Diabetes 54:968–975
Mussmann R, Geese M, Harder F et al (2007) Inhibition of glycogen synthase kinase (GSK) 3 promotes replication and survival of pancreatic beta cells. J Biol Chem 282:12030–12037
Kushner JA, Ye J, Schubert M et al (2002) Pdx1 restores beta cell function in Irs2 knockout mice. J Clin Invest 109:1193–1201
Surjit M, Lal SK (2007) Glycogen synthase kinase-3 phosphorylates and regulates the stability of p27kip1 protein. Cell Cycle 6:580–588
Diehl JA, Cheng M, Roussel MF, Sherr CJ (1998) Glycogen synthase kinase-3beta regulates cyclin D1 proteolysis and subcellular localization. Genes Dev 12:3499–3511
Welsh GI, Miller CM, Loughlin AJ, Price NT, Proud CG (1998) Regulation of eukaryotic initiation factor eIF2B: glycogen synthase kinase-3 phosphorylates a conserved serine which undergoes dephosphorylation in response to insulin. FEBS Lett 421:125–130
Drucker DJ (2007) The role of gut hormones in glucose homeostasis. J Clin Invest 117:24–32
Buteau J, Spatz ML, Accili D (2006) Transcription factor FoxO1 mediates glucagon-like peptide-1 effects on pancreatic beta-cell mass. Diabetes 55:1190–1196
Acknowledgements
We gratefully acknowledge C. Cras-Méneur for helpful suggestions and stimulating discussion, as well as assistance with the preparation of the figures and manuscript and their submission, and C. Welling for editorial assistance. We also would like to acknowledge M. Birnbaum for the gift of the human GSK3βS9A cDNA. This work was supported in part by a National Institutes of Health grant R37 DK16746 (M. A. Permutt), a Postdoctoral Fellowship Award from the Juvenile Diabetes Research Foundation International 3-2005-968 (Z. Liu), the Washington University Diabetes Research and Training Center (5P60 DK020579) and the Morphology Core of the Digestive Diseases Research Core Center at Washington University (5P30 DK052574).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, Z., Tanabe, K., Bernal-Mizrachi, E. et al. Mice with beta cell overexpression of glycogen synthase kinase-3β have reduced beta cell mass and proliferation. Diabetologia 51, 623–631 (2008). https://doi.org/10.1007/s00125-007-0914-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-007-0914-7