Abstract
Aims/hypothesis
Excess glucose transport to embryos during diabetic pregnancy causes congenital malformations. The early postimplantation embryo expresses the gene encoding the high-K m GLUT2 (also known as SLC2A2) glucose transporter. The hypothesis tested here is that high-K m glucose transport by GLUT2 causes malformations resulting from maternal hyperglycaemia during diabetic pregnancy.
Materials and methods
Glut2 mRNA was assayed by RT-PCR. The K m of embryo glucose transport was determined by measuring 0.5–20 mmol/l 2-deoxy[3H]glucose transport. To test whether the GLUT2 transporter is required for neural tube defects resulting from maternal hyperglycaemia, Glut2 +/− mice were crossed and transient hyperglycaemia was induced by glucose injection on day 7.5 of pregnancy. Embryos were recovered on day 10.5, and the incidence of neural tube defects in wild-type, Glut2 +/− and Glut2 −/− embryos was scored.
Results
Early postimplantation embryos expressed Glut2, and expression was unaffected by maternal diabetes. Moreover, glucose transport by these embryos showed Michaelis–Menten kinetics of 16.19 mmol/l, consistent with transport mediated by GLUT2. In pregnancies made hyperglycaemic on day 7.5, neural tube defects were significantly increased in wild-type embryos, but Glut2 +/− embryos were partially protected from neural tube defects, and Glut2 −/− embryos were completely protected from these defects. The frequency of occurrence of wild-type, Glut2 +/− and Glut2 −/− embryos suggests that the presence of Glut2 alleles confers a survival advantage in embryos before day 10.5.
Conclusions/interpretations
High-K m glucose transport by the GLUT2 glucose transporter during organogenesis is responsible for the embryopathic effects of maternal diabetes.
Similar content being viewed by others
Introduction
Maternal diabetes significantly increases the risk of congenital malformations: while rigorous glycaemic control in the periconception period reduces the incidence of congenital malformations, the incidence remains three to fivefold greater than that for non-diabetic pregnancy [1–5]. These malformations arise during the earliest stages of organogenesis, corresponding to approximately weeks 2–8 in human gestation [6]. Both type 1 and type 2 diabetes increases the risk of congenital malformations [2, 7]. The metabolic profiles of type 1 and type 2 diabetes are different, except for episodic hyperglycaemia. Numerous studies have shown that the incidences of early miscarriage and congenital malformations are associated with poor glycaemic control [8–10]. These observations suggest that excess glucose, or a metabolic process activated by high glucose concentration in both type 1 and type 2 diabetes, is responsible for the teratogenic effect of diabetic pregnancy.
There are 14 known members of the solute carrier 2 (SLC2) family of facilitative hexose and polyol transporters, characterised by 12 transmembrane domains and the presence of several conserved amino acids [11, 12]. The different members of the SLC2 family differ in substrate specificity, affinity for cytochalasin B, inhibition by phloretin or phlorizin, and regulation by insulin [11]. Of the 14 SLC2 gene family members, expression of Glut1, Glut2, Glut3, Glut8 and Glut12 (also known as Slc2a1, Slc2a2, Slc2a3, Slc2a8 and Slc2a12) is detected in preimplantation mouse embryos [13–18]. GLUT12 protein is not detected in early postimplantation embryos, but it is detected later, during fetal development [17, 19]. Only expression of Glut1, Glut2 and Glut3 has been detected during the stage of postimplantation development that is susceptible to diabetic embryopathy (day 7.5) [12, 13, 20–23]. Glut1 is expressed primarily in the ectoplacental cone, amnion, chorion and mesodermal layer of the yolk sac, and lower levels are expressed in the embryonic ectoderm. Northern blotting shows that Glut2 mRNA is expressed at high levels on days 7.5 and 8.5 but is barely detectable on day 9.5; most of the expression is in the endodermal layer of the visceral yolk sac. Glut3 expression is primarily in the amnion, chorion and endodermal layer of the yolk sac [20]. Both GLUT1 and GLUT3 have affinities that approximate physiological glucose concentrations. GLUT2, however, has a K m that is two- to threefold higher than physiological glucose concentrations [24]. Postnatally, GLUT2 is produced by pancreatic beta cells, hepatocytes, intestine and kidney—tissues that must transport glucose with high efficiency when its concentration is high, for example after intestinal absorption of nutrients following feeding [11, 25]. GLUT2 is essential for glucose-stimulated insulin release, and also regulates glucose sensing by extrapancreatic tissues [26, 27]. However, the early embryo is not normally exposed to glucose concentrations approaching the K m of the GLUT2 transporter. Thus, during normal, non-diabetic gestation, glucose transporters with a low K m (high affinity) would transport glucose into the embryo cells more efficiently than the GLUT2 transporter. There have been some reports that GLUT1 and GLUT3, which are produced in the postimplantation embryo during early organogenesis, are not downregulated during exposure to a hyperglycaemic environment, and so could continue to transport glucose even during maternal hyperglycaemia [21, 22]. However, the rate of glucose transport by GLUT1 and GLUT3 would saturate during hyperglycaemia. In contrast, transport by the high-K m GLUT2 transporter would become more efficient during hyperglycaemia and might allow the rate of glucose transport into embryo cells to increase two to threefold.
In the rat, the intracellular glucose concentration in the embryo neuroepithelium is at equilibrium with maternal serum, even when the mother is hyperglycaemic [28]. This indicates that glucose is freely transportable into embryo cells, even when maternal glucose concentrations are above the K m for low-K m glucose transporters.
Neural tube defects (NTD), which are among the most common malformations that occur in the offspring of diabetic human mothers [29, 30], are significantly increased in the embryos of diabetic mice and rats [31–33]. That high glucose concentration is responsible for the teratogenic effects of diabetic pregnancy has been demonstrated using three approaches: (1) inducing hyperglycaemia in pregnant non-diabetic mice by glucose injection causes NTD; (2) lowering blood glucose concentrations in pregnant diabetic animals with phlorizin to cause renal glucose clearance reduces NTD; and (3) culturing fragments of neurulating embryos in media containing concentrations of glucose that are equivalent to those in serum during diabetes (15 mmol/l) inhibits expression of Pax3, a gene required for neural tube closure, compared with culture in media containing 5 mmol/l glucose [34]. It was noteworthy that in glucose-injected and phlorizin-treated animals, the incidence of NTD was not linearly correlated with maternal blood glucose concentration. Rather, the increase in NTD was not statistically significant until maternal blood glucose concentrations were ≥250 mg/dl (13.89 mmol/l) on the day before the onset of Pax3 expression [34]. This indicates that the threshold of maternal glycaemia above which there is a significant increase in NTD corresponds to the K m for the GLUT2 glucose transporter. Similarly, in human diabetic pregnancy, the relationship of adverse pregnancy outcome (spontaneous abortion and major malformation) with HbA1 is not linear but sigmoidal [8]. Although high HbA1 levels do not distinguish between episodic glycaemic excursions and chronic hyperglycaemia, they do indicate the steady-state exposure of maternal and embryo tissues to glucose during the preceding several weeks. A sigmoidal, rather than linear, association of poor glycaemic control with adverse pregnancy outcome is consistent with a model in which there is a threshold of maternal glycaemia above which damage to embryo development occurs.
In this study, we tested the hypothesis that the high-K m GLUT2 glucose transporter is essential for the embryopathic effects of maternal hyperglycaemia.
Materials and methods
Animal procedures
ICR mice (Taconic, Germantown, NY, USA) were obtained at 5–6 weeks of age and were used to generate embryos for the assay of Glut2 mRNA and 2-deoxy[3H]glucose transport. For the assay of Glut2 mRNA, mice were made diabetic with streptozotocin (STZ) (Sigma Chemicals, St Louis, MO, USA) as described [35]. Briefly, female mice to be made diabetic were injected intraperitoneally with STZ to destroy pancreatic beta cells. Hyperglycaemia before pregnancy was controlled with subcutaneously implanted insulin pellets (Linshin, Inc., Scarborough, ON, Canada). Diabetic and age-matched non-diabetic female mice were mated with non-diabetic ICR male mice about 3 weeks after insertion of insulin pellets and checked daily for copulation plugs. Day 0.5 of pregnancy was determined to be at 12.00 h on the day in which a copulation plug was found. The STZ-diabetic female mice became hyperglycaemic beginning on day 4.5 of pregnancy because of insufficiency of the insulin pellets during pregnancy [35]. Pregnant mice were killed by cervical dislocation to recover embryos on day 7.5 for the assay of Glut2 mRNA or 2-deoxy-d-[3H]glucose transport.
Mice carrying a Glut2 knockout allele [26] on a 129/SvJ background were used to generate embryos that were GLUT2-deficient. The Glut2 knockout strain was originally generated on a mixed C57Bl/6J × 129/Sv background. C57Bl/6J embryos are resistant to diabetic embryopathy [36]. Therefore, a congenic strain was generated to place the Glut2 +/− allele on a 129/SvJ background [37]. Offspring at each generation with the least residual donor background (C57Bl/6J) were identified by marker-assisted gene analysis [38] performed by the Speed Congenics facility of the Jackson Laboratory (Bar Harbor, ME, USA). The strain was considered to be congenic once it retained <0.2% C57Bl/6J DNA [37].
Non-diabetic Glut2 +/− male and female mice were mated and hyperglycaemia or oxidative stress was induced on day 7.5 as described previously [34, 39]. Briefly, transient hyperglycaemia was induced by injecting 2 ml of 12.5% glucose–PBS solution subcutaneously approximately every 1–2 h between 09.00 and 17.00 h. Blood glucose concentrations were checked hourly, and animals were re-injected as needed to maintain the blood glucose concentration ≥300 mg/dl (16.65 mmol/l). Oxidative stress was induced with a single injection of 3 mg/kg antimycin A (Sigma Chemicals), a mitochondrial complex III inhibitor [40, 41], dissolved in 25% (v/v) propylene glycol. Control mice were injected with PBS or propylene glycol. Embryos were dissected from uteri and removed from surrounding membranes on day 10.5 as described [42] under a Nikon SMZ stereo microscope. Embryos were inspected externally for NTD as defined by an open or malformed cranium or spinal neural tube. Embryos were photographed with a Spot colour digital camera mounted on the stereo microscope using Spot 3.5 software (Micro Video Instruments, Avon, MA, USA).
All procedures performed using animals followed the National Institutes of Health’s Principles of laboratory animal care and were approved by the Institutional Animal Care and Use Committee of the Joslin Diabetes Center.
RT-PCR assay of Glut2 mRNA
Day-7.5 embryos from individual diabetic or non-diabetic pregnancies were pooled. RNA was isolated and reverse-transcribed, and serial dilutions of the reverse transcription products were amplified by PCR as described previously [35]. The cDNA products were amplified using primers complementary to the Glut2 amplicon [43] and the PCR conditions described below, or to constitutively expressed 36B4 (also known as Arbp), which was used as a normalisation control, as described [35, 44]. Autoradiographs of the electrophoresed PCR products were scanned, and unsaturated bands were quantified using Adobe Photoshop (version 9.0.1, Adobe Systems, Inc., San Jose, CA). The amount of Glut2 RT-PCR product was expressed relative to that of the 36B4 RT-PCR product.
Measurement of glucose transport kinetics
Uptake of 2-deoxy-d-[3H]glucose by day-7.5 embryos was assayed using a procedure modified after that of Cheatham et al. [45]. Briefly, embryos with surrounding amniotic and yolk sac membranes were dissected in cold DMEM containing 5 mmol/l glucose (Invitrogen, Carlsbad, CA, USA) with 10% FCS. Pooled embryos were washed with KRH buffer [45], and incubated for 5 min with collagenase, while passing up and down with a 1 ml micropipette tip. The embryo fragments were rinsed with KRH buffer, and the equivalent of three or four embryos was distributed into individual tubes. Tissues were incubated for 30 s with 0.5–20 mmol/l 2-deoxy-d-[3H]glucose (2-deoxy-d-[1,2-3H]glucose, specific activity 969 GBq/mmol; Perkin Elmer–New England Nuclear, Boston, MA, USA) at a constant specific activity of 185 Bq/mmol. Samples were incubated without or with cytochalasin B (Sigma), added at 0.4 or 4.0 μmol/l. Samples incubated with 0.5–20 mmol/l l-[3H]glucose (l-[1-3H] glucose; Perkin Elmer–New England Nuclear) were used as controls for non-specific glucose uptake. The specific activity of l-[3H]glucose was comparable with that of 2-deoxy-d-[3H]glucose, and was added to the l-glucose incubation solution to give a constant specific activity of 185 Bq/mmol. Reactions were terminated by adding 1 ml cold PBS, followed by centrifugation and three washes with PBS. Pellets were solubilised with 0.5 ml of 0.05% SDS. Four-hundred microlitres of the solubilised pellet was counted for radioactivity and 100 μl was used for protein measurement (Bio-Rad, Hercules, CA, USA). The K m and V max of 2-deoxy-d-glucose uptake were determined using non-linear curve fitting analysis with the Michaelis–Menten equation (Prism, version 4.0; GraphPad Software, Inc., San Diego, CA, USA).
Genotype analysis of Glut2 allele
Glut2 +/− pups were identified by PCR analysis of tail DNA using the previously reported primer sequences [42, 43] and the following conditions: 94°C for 5 min, followed by 36 cycles of 94°C for 30 s, 53°C for 30 s, 72°C for 30 s and 72°C for 10 min. DNA was prepared using DNAzol (Molecular Research Center, Cincinnati, OH, USA) according to the manufacturer’s instructions. Genotypes of embryos of Glut2 +/− × Glut2 +/− matings were determined similarly using yolk sac DNA.
Statistical analysis
χ 2 analyses were performed using Prism (version 4.0) software for Macintosh (GraphPad Software).
Results
Mouse embryos produce a functional high-Km GLUT2 glucose transporter
It had been shown previously that mouse embryos express Glut2 mRNA from the eight-cell stage until at least day 9.5 [13]. However, expression had not been examined during diabetic pregnancy. Whereas expression of Glut1 and Glut3 is not downregulated during maternal hyperglycaemia in the postimplantation embryo [21, 22], expression of Glut1, Glut2 and Glut3 has been found to be downregulated by high glucose concentration in the preimplantation embryo [46]. Glut2 mRNA was assayed in embryos recovered on day 7.5, the day of embryonic development that is susceptible to subsequent development of NTD in response to maternal hyperglycaemia [34]. As shown in Fig. 1, Glut2 mRNA was expressed on day 7.5 by embryos of both diabetic and non-diabetic mice, and there was no effect of maternal diabetes on expression of Glut2 mRNA.
RT-PCR of Glut2 and 36B4 RNA from day 7.5 embryos of diabetic and non-diabetic mice. Embryos from individual diabetic (D) or non-diabetic (ND) pregnancies were pooled and assayed for Glut2 or 36B4 RNA as described in Materials and methods. The abundance of the Glut2 PCR product is expressed relative to the abundance of the 36B4 PCR product. The data are the results of three diabetic and three non-diabetic pregnancies (mean ± SEM). There is no significant difference between the abundance of Glut2 RNA relative to that of 36B4 (p = 0.74). AU Arbitrary units
To determine whether glucose transport by day-7.5 mouse embryos exhibits high-K m kinetics, the Michaelis–Menten kinetics of glucose transport were assayed. Embryo tissues were incubated with 2-deoxy-d-[3H]glucose in the presence of 0.5–20 mmol/l 2-deoxy-d-glucose. Analysis of the glucose transport curve using the Michaelis–Menten equation demonstrated that the embryo glucose transporter had a K m of 16.19 mmol/l, which is consistent with the K m of the GLUT2 glucose transporter (Fig. 2a). Transport of 2-deoxy-d-glucose was not inhibited by 0.4 μmol/l cytochalasin B (Fig. 2b), a concentration that inhibits glucose transport by GLUT1 and GLUT3, but 2-deoxy-d-glucose transport was inhibited by 4.0 μmol/l cytochalasin B (Fig. 2c), a concentration that inhibits glucose transport by GLUT2. The embryo glucose transporter was specific for the d-glucose isoform, as specific, saturable transport of l-glucose did not occur (Fig. 2d).
Kinetics of glucose uptake by day 7.5 embryos. a Transport of 0.5–20 mmol/l 2-deoxy-d-[3H]glucose. V max = 0.109 mmol/l, K m = 16.91 mmol/l. b Transport of 0.5–20 mmol/l 2-deoxy-d-[3H]glucose in the presence of 0.4 μmol/l cytochalasin B. c Transport of 0.5–20 mmol/l 2-deoxy-d-[3H]glucose in the presence of 4.0 μmol/l cytochalasin B. d Transport of 0.5–20 mmol/l l-[3H]glucose
Mouse embryos lacking a functional GLUT2 glucose transporter are resistant to hyperglycaemia-induced NTD
If glucose uptake by the GLUT2 glucose transporter is essential for diabetic embryopathy, then embryos in which only GLUT2-mediated glucose uptake is non-functional should be resistant to the teratogenic effects of hyperglycaemia. It is possible to test this using Glut2 −/− embryos.
Female and male Glut2 +/− mice were crossed to generate wild-type, Glut2 +/− and Glut2 −/− embryos. On day 7.5 of pregnancy, female mice were made hyperglycaemic by subcutaneous glucose injection at approximately hourly intervals. This is sufficient to induce NTD associated with diabetic embryopathy [34]. Control pregnancies were injected with PBS. The mean blood glucose concentration was 18.91 ± 0.54 mmol/l, compared with 6.88 ± 0.18 mmol/l in PBS-injected controls.
Embryos were recovered on day 10.5 of gestation and scored for NTD. Embryo genotype was determined as described in Materials and methods. In the PBS-injected pregnancies, all embryos of all genotypes were normal, except for one heterozygous embryo, which displayed a mild defect (a closed neural tube with a slightly underexpanded IVth ventricle, resembling holoprosencephaly) (Fig. 3a). However, in glucose-injected pregnancies there was a significant effect of embryo genotype on the incidence of NTD (Fig. 3b). Thirty-seven per cent of wild-type embryos displayed NTD (severe, open NTD, primarily exencephaly, as shown in Fig. 4), whereas less than half as many (16%) of haploinsufficient Glut2 +/− embryos displayed NTD, and none of the GLUT2-deficient Glut2 −/− embryos were affected by NTD.
Incidences of malformed (open bars) and normal (solid bars) neural tube development in wild-type, Glut2 +/− and Glut2 −/− embryos in pregnancies treated with a PBS (n = 7 pregnancies), b glucose (n = 11 pregnancies) or c antimycin A (n = 10 pregnancies) on day 7.5. There was a significant difference in the incidence of malformation in embryos of different genotypes by χ 2 analysis only in (b) (p < 0.02). +/+, Glut2 wild type; +/−, Glut2 +/−; −/−, Glut2 −/−
To determine whether GLUT2-deficient embryos were susceptible to NTD caused by biochemical events distal to glucose transport, pregnant mice were given a single injection of antimycin A on day 7.5. Antimycin A is a mitochondrial complex III inhibitor that stimulates superoxide production [40, 41] and mimics the effects of maternal diabetes on Pax3 expression and NTD [39, 47]. As shown in Fig. 3c, antimycin A induced NTD in embryos of all genotypes. While the incidence of NTD in the Glut2 −/− embryos was less than in Glut2 +/+and Glut2 +/− embryos (15 vs 44%), there was no significant difference in the incidence of NTD of embryos of any genotype.
It was noteworthy that, whereas the average number of embryos recovered per pregnancy from each treatment group did not differ (6.7, 6.3 and 7 from PBS-, glucose- and antimycin A-injected pregnancies, respectively), the genotypes of embryos did not occur with the expected Mendelian frequency of one-fourth wild-type, one-half heterozygous and one-fourth homozygous Glut2-deficient (Table 1). Indeed, the percentages of the three genotypes were not 25:50:25 but 52:29:17. χ 2 analyses showed that the variance with regard to the expected Mendelian frequency of each genotype was statistically significant, and that the incidence of each genotype was not different in any of the treatment groups. This suggests that the presence of two wild-type Glut2 alleles confers a survival advantage before day 10.5 of embryonic development, and that the presence of one wild-type Glut2 allele is advantageous over total Glut2 deficiency, at least on a 129Sv/J background.
Discussion
The data reported here confirm that the early postimplantation embryo, at the stage of development that is susceptible to NTDs induced by diabetic pregnancy, expresses the gene encoding the high K m GLUT2 glucose transporter. Expression of Glut1, Glut2 and Glut3 is suppressed in preimplantation embryos of diabetic mice [46], and expression of Glut1 has been found to be both unchanged or suppressed by maternal diabetes or high-glucose culture in postimplantation embryos [21, 22]. However, in the present study, expression of Glut2 was unaffected by maternal diabetes. Furthermore, the early embryo produces a functional high-K m transporter, as the K m of glucose uptake is 16.19 mmol/l, and it was not inhibited by 0.4 μmol/l cytochalasin B but it was inhibited by 4.0 μmol/l cytochalasin B. GLUT2-deficient embryos of hyperglycaemic mothers were resistant to hyperglycaemia-induced NTD, indicating that glucose transported into embryo cells by GLUT2, but not other glucose transporters, mediates the embryopathic effects of maternal hyperglycaemia.
It is interesting to note that in patients with diabetes, the tissues that suffer from the adverse effects of hyperglycaemia during the pathogenesis of diabetic complications, such as the vasculature and nerves, do not express GLUT2. However, if the rate of glucose phosphorylation by these tissues is sufficiently high, a concentration gradient driving sustained glucose uptake can be maintained. On the other hand, it may take years for the accumulated damage from hyperglycaemia to be clinically detectable, whereas the adverse effects of maternal hyperglycaemia on the embryo are apparent within hours. Therefore, the rate of glucose metabolism and ensuing adverse effects on embryo physiology may be far in excess of that which occurs in tissues producing only low-K m glucose transporters.
During non-diabetic pregnancy, the embryo or fetus would not be exposed to glucose at concentrations approaching the K m of the GLUT2 transporter. Therefore, there does not appear to be an occasion when this transporter would mediate glucose uptake. Furthermore, since embryos also produce GLUT1 and GLUT3, which mediate low-K m (high-affinity) glucose transporters at normal, non-diabetic, circulating glucose concentrations, the need for a high-K m (low-affinity) transporter is not obvious.
Before we began this study, we considered that, because Glut2 −/− pups are viable until weaning [26], GLUT2 is not necessary for embryonic or fetal development. Therefore, as explained above, its presence or absence would appear to have little consequence during non-diabetic pregnancy, and so the expression of Glut2 may be vestigial. For example, embryos of oviparous animals derive glucose that is stored as glycogen in egg yolk at quantities sufficient to provide energy until hatching. The concentration of glucose that is transported to the embryo from the egg yolk might approach the K m of GLUT2. Indeed, the concentration of glucose in the yolk of a neurulating chick embryo is approximately 11 mmol/l (Fine and Loeken, unpublished data). Thus, there might be no selective pressure to retain expression of Glut2, but also no selective pressure against its expression during normal mammalian gestation.
However, the frequency of occurrence of each Glut2 genotype in embryos recovered from Glut2 +/− × Glut2 +/− matings suggests that, although the expression of Glut2 is not absolutely required for embryonic life, GLUT2 sufficiency confers a significant survival advantage before embryonic day 10.5 over GLUT2 deficiency. It is not known when, before day 10.5, the GLUT2-deficient embryos are lost, but because there were no implantation sites containing reabsorbing embryos, and implantation sites of embryos that die at day 7.5 or later were still detectable on day 10.5, the embryos must have died before day 7.5. Glut2 mRNA is detected beginning at the eight-cell stage [13], so the embryos were probably lost between the eight-cell stage and very early postimplantation development.
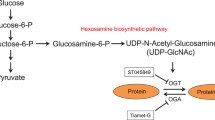
The non-Mendelian occurrence of Glut2 +/− and Glut2 −/− embryos was not expected, because when the Glut2 knockout line was first generated the occurrence of each of the genotypes from Glut2 +/− parents was Mendelian [26]. However, the original Glut2 knockout line was generated on a mixed C57Bl/6J × 129/Sv background, whereas the mice used here were on a pure 129Sv/J background. This suggests that there are polymorphic modifier genes that can complement the function of GLUT2 on some strain backgrounds but not on others. It is possible that GLUT2 transports a solute other than glucose during normal embryogenesis. It was recently recognised that GLUT2 is a high-affinity (low-K m) transporter of glucosamine [48]. Glucosamine can be a substrate for the intermediates of post-translational glycosylation. Carbohydrate modification of proteins is essential for the production of extracellular matrix, as well as secreted and intracellular glycoproteins. The principal site of serum glucosamine synthesis is the liver [49]. Although glucosamine-6-phosphate is synthesised from the glycolytic intermediate, fructose-6-phosphate, and glutamine, it can also be generated by phosphorylation of glucosamine transported from extracellular sources. Because the early embryo derives its energy primarily through glycolytic (anaerobic) glucose metabolism [50], it is possible that in 129Sv/J embryos the rate of conversion of fructose-6-phosphate to fructose-1,6-biphosphate leaves a suboptimal concentration of fructose 6-phosphate to serve as a substrate for hexosamine biosynthesis, thereby increasing the need to derive glucosamine from maternal circulation.
In conclusion, production of a functional, high K m GLUT2 glucose transporter confers sensitivity of the early postimplantation embryo to hyperglycaemia-induced malformations. Embryos lacking GLUT2 glucose transporters are structurally normal, although GLUT2-haploinsufficient and -deficient embryos are less viable than embryos that express two wild-type Glut2 alleles. However, when maternal glucose concentrations approach the K m of GLUT2, excessive glucose transport into embryo cells will affect embryonic development adversely.
Abbreviations
- NTD:
-
neural tube defect
- SLC2:
-
solute carrier 2
References
Suhonen L, Hiilesmaa V, Teramo K (2000) Glycaemic control during early pregnancy and fetal malformations in women with type I diabetes mellitus. Diabetologia 43:79–82
Schaefer-Graf UM, Buchanan TA, Xiang A, Songster G, Montoro M, Kjos SL (2000) Patterns of congenital anomalies and relationship to initial maternal fasting glucose levels in pregnancies complicated by type 2 and gestational diabetes. Am J Obstet Gynecol 182:313–320
Loffredo CA, Wilson PD, Ferencz C (2001) Maternal diabetes: an independent risk factor for major cardiovascular malformations with increased mortality of affected infants. Teratology 64:98–106
Wren C, Birrell G, Hawthorne G (2003) Cardiovascular malformations in infants of diabetic mothers. Heart 89:1217–1220
Evers IM, de Valk HW, Visser GH (2004) Risk of complications of pregnancy in women with type 1 diabetes: nationwide prospective study in The Netherlands. BMJ 328:915–919
Mills JL, Baker L, Goldman AS (1979) Malformations in infants of diabetic mothers occur before the seventh gestational week: implications for treatment. Diabetes 28:292–293
Farrell T, Neale L, Cundy T (2002) Congenital anomalies in the offspring of women with type 1, type 2 and gestational diabetes. Diabet Med 19:322–326
Greene MF, Jare JW, Cloherty JP, Cenacerraf BR, Soeldner JS (1989) First-trimester hemoglobin A1 and risk for major malformation and spontaneous abortion in diabetic pregnancy. Teratology 39:225–231
Miller E, Hare JW, Cloherty JP et al (1981) Elevated maternal hemoglobin A1c in early pregnancy and major congenital anomalies in infants of diabetic mothers. N Engl J Med 304:1331–1334
The DCCT Research Group (1996) Pregnancy outcomes in the diabetes control and complications trial. Am J Obstet Gynecol 174:1343–1353
Uldry M, Thorens B (2004) The SLC2 family of facilitated hexose and polyol transporters. Pflugers Arch 447:480–489
Wu X, Freeze HH (2002) GLUT14, a duplicon of GLUT3, is specifically expressed in testis as alternative splice forms. Genomics 80:553–557
Hogan A, Heyner S, Charon MJ et al (1991) Glucose transporter gene expression in early mouse embryos. Development 113:363–372
Aghayan M, Rao LV, Smith RM et al (1992) Developmental expression and cellular localization of glucose transporter molecules during mouse preimplantation development. Development 115:305–312
Dan-Goor M, Sasson S, Davarashvili A, Almagor M (1997) Expression of glucose transporter and glucose uptake in human oocytes and preimplantation embryos. Hum Reprod 12:2508–2510
Carayannopoulos MO, Chi MM, Cui Y et al (2000) GLUT8 is a glucose transporter responsible for insulin-stimulated glucose uptake in the blastocyst. Proc Natl Acad Sci USA 97:313–318
Zhou Y, Kaye PL, Pantaleon M (2004) Identification of the facilitative glucose transporter 12 gene Glut12 in mouse preimplantation embryos. Gene Expr Patterns 4:621–631
Pantaleon M, Harvey MB, Pascoe WS, James DE, Kaye PL (1997) Glucose transporter GLUT3: ontogeny, targeting, and role in the mouse blastocyst. Proc Natl Acad Sci USA 94:3795–3800
Macheda ML, Kelly DJ, Best JD, Rogers S (2002) Expression during rat fetal development of GLUT12—a member of the class III hexose transporter family. Anat Embryol (Berl) 205:441–452
Smith DE, Gridley T (1992) Differential screening of a PCR-generated mouse embryo cDNA library: glucose transporters are differentially expressed in early postimplantation mouse embryos. Development 116:555–561
Trocino RA, Akazawa S, Takino H et al (1994) Cellular-tissue localization and regulation of the GLUT-1 protein in both the embryo and the visceral yolk sac from normal and experimental diabetic rats during the early postimplantation period. Endocrinology 134:869–878
Takao Y, Akazawa S, Matsumoto K et al (1993) Glucose transporter gene expression in rat conceptus during high glucose culture. Diabetologia 36:696–706
Matsumoto K, Akazawa S, Ishibashi M et al (1995) Abundant expression of GLUT1 and GLUT3 in rat embryo during the early organogenesis period. Biochem Biophys Res Commun 209:95–102
Thorens B (1996) Glucose transporters in the regulation of intestinal, renal, and liver glucose fluxes. Am J Physiol 270:G541–G553
Pessin JE, Bell GI (1992) Mammalian facilitative glucose transporter family: structure and molecular regulation. Annu Rev Physiol 54:911–930
Guillam M-T, Hummler E, Schaerer E et al (1997) Early diabetes and abnormal postnatal pancreatic islet development in mice lacking Glut-2. Nat Genet 17:327–330
Thorens B (2001) GLUT2 in pancreatic and extra-pancreatic gluco-detection. Mol Membr Biol (Review) 18:265–273
Sussman I, Matschinsky FM (1988) Diabetes affects sorbitol and myo-inositol levels of neuroectodermal tissue during embryogenesis in rat. Diabetes 37:974–981
Becerra JE, Khoury MJ, Corder JF, Erickson JD (1990) Diabetes mellitus during pregnancy and the risks for the specific birth defects: a population-based case-control study. Pediatrics 85:1–9
Martinez-Frias ML (1994) Epidemiological analysis of outcomes of pregnancy in diabetic mothers: identification of the most characteristic and most frequent congenital anomalies. Am J Med Genet 51:108–113
Phelan S, Loeken M (1998) Identification of a new binding motif for the paired domain of Pax-3 and unusual characteristics of spacing and of bipartite recognition elements on binding and transcription activation. J Biol Chem 273:19153–19159
Viana M, Herrera E, Bonet B (1996) Teratogenic effects of diabetes mellitus in the rat. Prevention by vitamin E. Diabetologia 39:1041–1046
Eriksson UJ (1991) Diabetes in pregnancy: effects on post-implantation embryos. Isr J Med Sci 27:478–486
Fine E, Horal M, Chang TI, Fortin G, Loeken MR (1999) Hyperglycemia is responsible for altered gene expression, apoptosis, and neural tube defects associated with diabetic pregnancy. Diabetes 48:2454–2462
Phelan SA, Ito M, Loeken MR (1997) Neural tube defects in embryos of diabetic mice: role of the Pax-3 gene and apoptosis. Diabetes 46:1189–1197
Pani L, Horal M, Loeken MR (2002) Polymorphic susceptibility to the molecular causes of neural tube defects during diabetic embryopathy. Diabetes 51:2871–2874
Silver LM (1995) Mouse genetics: concepts and applications. Oxford University Press, New York
Markel P, Shu P, Ebeling C et al (1997) Theoretical and empirical issues for marker-assisted breeding of congenic mouse strains. Nat Genet 17:280–284
Chang TI, Horal M, Jain S, Wang F, Patel R, Loeken MR (2003) Oxidant regulation of gene expression and neural tube development: insights gained from diabetic pregnancy on molecular causes of neural tube defects. Diabetologia 46:538–545
Boveris A (1977) Mitochondrial production of superoxide radical and hydrogen peroxide. Adv Exp Med Biol 78:67–82
Turrens JF, Alexandre A, Lehninger AL (1985) Ubisemiquinone is the electron donor for superoxide formation by complex III of heart mitochondria. Arch Biochem Biophys 237:408–414
Hogan B, Costantini F, Lacy E (eds) (1986) Manipulating the mouse embryo: a laboratory manual. Cold Spring Harbor, Cold Spring Harbor, NY
Thorens B, Guillam MT, Beermann F, Burcelin R, Jaquet M (2000) Transgenic reexpression of GLUT1 or GLUT2 in pancreatic beta cells rescues GLUT2-null mice from early death and restores normal glucose-stimulated insulin secretion. J Biol Chem 275:23751–23758
Cai J, Phelan SA, Hill AL, Loeken MR (1998) Identification of Dep-1, a new gene that is regulated by the transcription factor, Pax-3, as a marker for altered embryonic gene expression during diabetic pregnancy. Diabetes 47:1803–1805
Cheatham B, Wang L, Blenis J, Kahn, CR (1994) Phosphatidylinositol 3-kinase activation is required for insulin stimulation of pp70 S6 kinase, DNA synthesis, and glucose transporter translocation. Mol Cell Biol 14:4902–4911
Moley KH, Chi MMY, Mueckler MM (1998) Maternal hyperglycemia alters glucose transport and utilization in mouse preimplantation embryos. Am J Physiol Endocrinol Metab 38:E38–E47
Li R, Chse M, Jung SK, Smith PJS, Loeken MR (2005) Hypoxic stress in diabetic pregnancy contributes to impaired embryo gene expression and defective development by inducing oxidative stress. Am J Physiol Endocrinol Metab 289:E591–E599
Uldry M, Ibberson M, Hosokawa M, Thorens B (2002) GLUT2 is a high affinity glucosamine transporter. FEBS Lett 524:199–203
Spiro RG (1959) Studies on the biosynthesis of glucosamine in the intact rat. J Biol Chem 234:742–748
Akazawa S, Unterman T, Metzger BE (1994) Glucose metabolism in separated embryos and investing membranes during organogenesis in the rat. Metabolism 43:830–835
Acknowledgements
This work was supported by grants from the National Institutes of Health (DK52865 and DK58300) to M.R. Loeken. We are grateful for technical assistance from Rakhi Patel and Julie Adams, and to members of the Loeken laboratory for helpful discussions.
Duality of interest
The authors do not have any duality of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, R., Thorens, B. & Loeken, M.R. Expression of the gene encoding the high-K m glucose transporter 2 by the early postimplantation mouse embryo is essential for neural tube defects associated with diabetic embryopathy. Diabetologia 50, 682–689 (2007). https://doi.org/10.1007/s00125-006-0579-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0579-7