Abstract
Aims/hypothesis
We investigated glucagon responses during OGTT and isoglycaemic i.v. glucose infusion, respectively, to further elucidate the mechanisms behind the glucose intolerance in patients with type 2 diabetes.
Materials and methods
Ten patients (eight men) with type 2 diabetes (age: 64 [51–80] years; BMI: 23 [21–26] kg/m2; HbA1c: 6.9 [6.2–8.7]%, values mean [range]) and ten control subjects matched for sex, age and BMI were studied. Blood was sampled on two separate days following a 4-h 50-g OGTT and an isoglycaemic i.v. glucose infusion, respectively.
Results
Isoglycaemia during the 2 days was obtained in both groups. In the control subjects no difference in glucagon suppression during the first 45 min of OGTT and isoglycaemic i.v. glucose infusion (−36 ± 12 vs −64 ± 23 mmol/l × 45 min; p = NS) was observed, whereas in the group of patients with type 2 diabetes significant glucagon suppression only occurred following isoglycaemic i.v. glucose infusion (−63 ± 21 vs 10 ± 16 mmol/l × 45 min; p = 0.002). The incretin effect was significantly reduced in patients with type 2 diabetes compared with control subjects, but no significant differences in the secretion of glucagon-like peptide-1 or glucose-dependent insulinotropic polypeptide between the two groups during OGTT or isoglycaemic i.v. glucose infusion, respectively, could explain this.
Conclusions/interpretation
Attenuated and delayed glucagon suppression in patients with type 2 diabetes occurs after oral ingestion of glucose, while isoglycaemic i.v. administration of glucose results in normal suppression of glucagon. We suggest that this phenomenon contributes both to the glucose intolerance and to the reduced incretin effect observed in patients with type 2 diabetes.
Similar content being viewed by others
Introduction
In type 2 diabetes plasma glucagon concentrations fail to decrease appropriately or, paradoxically, may even increase, after oral glucose or carbohydrate ingestion [1–4]. By increasing hepatic glucose production, this lack of glucagon suppression contributes significantly to postprandial hyperglycaemia in subjects with type 2 diabetes [5–8]. It has been proposed that the non-suppressible glucagon secretion could be an early alpha-cell-specific islet defect that precedes insulin deficiency [9], but the exact mechanisms underlying the disturbed regulation of glucagon in type 2 diabetes remain to be elucidated.
The phenomenon that oral glucose elicits a higher insulin response than does i.v. glucose, even at identical plasma glucose (PG) profiles (isoglycaemia), is called the incretin effect. The incretin effect is caused by the two incretin hormones: glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) [10]. Both hormones are secreted from endocrine mucosal cells in the small intestine (L- and K-cells, respectively) in response to ingestion of nutrients [10]. They are highly insulinotropic in a strictly glucose-dependent fashion [10]. GLP-1 is known to also inhibit glucagon secretion in a glucose-dependent manner [10, 11], whereas GIP appears to have glucagonotropic properties [10, 12]. In type 2 diabetes, the incretin effect has been shown to be markedly reduced or even absent [13]. In previous studies we found that the postprandial GLP-1 response [14, 15] as well as the insulinotropic potency of GLP-1 [16] were reduced. In addition the insulinotropic effect of GIP is almost absent in patients with type 2 diabetes [17].
In the present study we aimed to elucidate the interplay between glucagon secretion and the reduced incretin effect in patients with type 2 diabetes. Therefore, we investigated glucagon, insulin and incretin responses during a 50-g OGTT and an isoglycaemic i.v. glucose infusion, respectively, in patients with type 2 diabetes and in matched healthy control subjects.
Subjects and methods
Subjects
Patients
Ten patients (eight men, two women) with type 2 diabetes diagnosed according to the WHO criteria [18, 19] were studied. Patient characteristics were: age: 62 (51–80) years; BMI: 23.3 (21.1–26.0) kg/m2; WHR: 1.0 (0.9–1.0); fasting plasma glucose (FPG): 8.6 (6.2–12.2) mmol/l; HbA1c: 6.9 (6.2–8.7)%; values mean (range). Four patients were being treated with diet, five with sulfonylurea and one with sulfonylurea in combination with metformin. The duration of known type 2 diabetes was 61 ± 17 months (mean±SEM). Diabetic retinopathy, nephropathy or neuropathy had not been clinically established in any of the patients. Three patients were receiving antihypertensive treatment (ACE inhibitors, thiazide with amiloride and a combination of beta-blockers, angiotensin II receptor antagonists, thiazide with KCl and calcium antagonists). Five were being treated with statins because of hypercholesterolaemia and one patient was taking digoxin and warfarin due to atrial fibrillation. Finally, one patient was diagnosed with colitis ulcerosa and was taking mesalazine to prevent exacerbations (no clinical or biochemical signs of inflammatory activity during the examinations).
Healthy control subjects
Ten healthy subjects (eight men, two women) without a family history of diabetes mellitus served as control subjects. Their characteristics were: age: 58 (44–69) years; BMI: 23.1 (20.0–25.0) kg/m2; WHR: 1.0 (0.9–1.0); FPG: 5.4 (4.9–6.0) mmol/l; HbA1c: 5.5 (5.1–5.8)%; PG concentration 120 min after a 75-g OGTT (PG120 min), conducted to establish that control subjects had NGT: 4.3 (3.1–6.7) mmol/l. Two of the subjects had hypertension and were receiving: (1) combined ACE inhibitor and thiazide therapy; and (2) angiotensin II receptor antagonists in combination with thiazide and beta-blockers, respectively. The latter was also taking statins because of hypercholesterolaemia. One control subject was on warfarin because of a previous deep venous thrombosis and one was taking beta-blockers due to atrial fibrillation.
All subjects
To our knowledge the drugs taken by the volunteers do not significantly influence beta cell function, alpha cell function or incretin effect. At any rate, they are unlikely to differentially affect the responses to oral compared with i.v. glucose in the same subject.
All participants were negative with regard to islet cell autoantibodies except for one patient with type 2 diabetes, who produced weakly positive fluorescence. This particular patient had had type 2 diabetes for more than 10 years and was being treated with a combination of diet and sulfonylurea. He was negative with regard to GAD-65 autoantibodies and his metabolic control was acceptable (HbA1c: 6.5%; FPG after discontinuation of sulfonylurea treatment for 1 week: 8.6 mmol/l). All participants were negative with regard to GAD-65, except for one control subject, who had positive GAD-65 (27.3 U/l; normal: < 9.5). This particular subject had normal glucose tolerance (PG120 min: 4.3 mmol/l; FPG 5.3 mmol/l, HbA1c 5.3%) and normal islet cell autoantibodies. Otherwise, all the subjects had normal clinical and biochemical parameters. None had impaired renal function, i.e. all had normal plasma creatinine levels < 130 μmol/l and no albuminuria.
All subjects agreed to participate (orally and in writing) after receiving oral and written information. The study was approved by the Scientific-Ethical Committee of the County of Copenhagen, March 2004 (registration number KA 04034) and was conducted according to the principles of the Helsinki Declaration II.
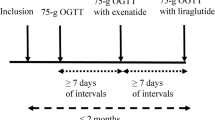
Experimental design
All subjects were studied on two separate occasions separated by at least 24 h. Before each occasion the patients with type 2 diabetes had not taken their glucose-lowering agents, if any, for a period of no less than 1 week. Other medication was not taken on the morning of the experiments (both groups). Otherwise the participants lived as usual. On both occasions the subjects were studied in a recumbent position after an overnight (10 h) fast.
On day 1, a cannula was inserted in the retrograde direction into a dorsal hand vein for collection of arterialised blood samples. The cannulated hand was placed in a heating box (42°C) throughout the experiment. For the 50-g OGTT the subjects ingested 50 g of water-free glucose dissolved in 400 ml water over the first 5 min of the experiment. Arterialised blood was drawn 15, 10 and 0 min before and 5, 10, 15, 20, 30, 40, 45, 50, 60, 70, 90, 120, 150, 180 and 240 min after ingestion of glucose. Blood was distributed into chilled tubes containing EDTA plus aprotinin (500 kIU/ml blood; Trasylol; Bayer, Leverkusen, Germany) and a specific dipeptidyl peptidase IV inhibitor (valine--pyrrolidide, final concentration 0.01 mmol/l; donated by R. D. Carr, Novo Nordisk, Bagsværd, Denmark) for analysis of glucagon, GLP-1 and GIP. For analysis of insulin and C-peptide, blood was distributed into chilled tubes containing heparin plus aprotinin (500 kIU/ml blood; Trasylol; Bayer). All tubes were immediately cooled on ice and then centrifuged for 20 min at 1,200 g and 4°C. Plasma for glucagon, GLP-1 and GIP analyses was stored at −20°C, and plasma for insulin and C-peptide analyses was stored at −80°C until analysis. For bedside measurement of PG, blood was distributed into fluoride tubes and centrifuged immediately for 2 min at 7,400 g at room temperature.
On day 2, a retrograde cannula was inserted in a dorsal hand vein for blood sampling (42°C) and a cannula was inserted in the contralateral cubital vein for glucose infusion. An isoglycaemic i.v. glucose infusion (20% w/v) was performed, aimed at copying the PG profile determined in the same individual on day 1 (50-g oral glucose load). Blood was sampled as on day 1, except for more frequent PG-sampling, every 5 min to adjust the glucose infusion rate in order to obtain isoglycaemia, and less frequent EDTA sampling.
Analysis
PG concentrations were measured during the experiments by the glucose oxidase method, using a glucose analyser (YSI 2300 STAT plus analyser; Yellow Springs Instruments, Yellow Springs, OH, USA).
Plasma samples were assayed for total GLP-1 immunoreactivity using an RIA (antiserum no. 89390) that is specific for the C-terminal of the GLP-1 molecule and reacts equally with intact GLP-1 and the primary (N-terminally truncated) metabolite [20]. Intact GLP-1 was measured using an enzyme-linked immunosorbent assay. The assay is a two-site sandwich assay using two monoclonal antibodies; GLP-1F5 as catching antibody (C-terminally directed) and Mab26.1 as detecting antibody (N-terminally directed) [21].
Total GIP was measured using the C-terminally directed antiserum R65, which reacts fully with intact GIP and the N-terminally truncated metabolite [22, 23]. Intact, biologically active, GIP was measured using antiserum no. 98171 [24].
Plasma insulin and C-peptide concentrations were measured using a commercial time-resolved fluoroimmunoassay (AutoDELFIA; Wallac Oy, Turku, Finland), as previously described [25].
The glucagon assay is directed against the C-terminal of the glucagon molecule (antibody code no. 4305) and therefore measures glucagon of mainly pancreatic origin [26]. Neither glicentin nor oxyntomodulin cross-react, whereas proglucagon 1–61, which is formed in the pancreas in very small amounts, but may also be found in gut extracts and in the circulation, does react fully in this assay [27, 28].
Calculations and statistical analysis
All results are expressed as means±SEM. AUC values were calculated using the trapezoidal rule and are presented as the incremental values, unless otherwise stated. Incretin effects were calculated by relating the difference in integrated beta cell secretory responses (insulin and C-peptide responses) between stimulation with oral and isoglycaemic i.v. glucose to the response after oral glucose, which was taken as 100% using the following formula: 100%×(AUCOGTT – AUCi.v.)/AUCOGTT [13]. In addition, the incretin effect was calculated by relating the difference between the 50 g of glucose ingested and the total amount of glucose infused intravenously to the 50 g of glucose ingested using the following formula: 100% × (glucoseOGTT – glucosei.v.)/glucoseOGTT. The latter method not only includes insulinotropic substances released upon intestinal stimulation, but also takes into account differences of all factors affecting PG concentrations (e.g. glucagon responses) during the two administration forms. The homeostatic model assessment (HOMA) was used to obtain a quantitative assessment of insulin resistance (HOMAIR) [29]. Comparisons of experimental determinations in which the data were distributed normally were made with two-tailed t-test (paired within groups, unpaired between groups). For data that did not follow a normal distribution, the significance of differences between groups was tested using Mann--Whitney U test; for within-subject comparisons Wilcoxon’s test for paired differences was used. Within-group comparisons of post-stimulus to basal values were made using repeated-measures ANOVA. A p value of < 0.05 was considered to be statistically significant.
Results
Glucose
No difference in FPG between day 1 and 2 was observed for the patients with type 2 diabetes (8.5 ± 0.5 vs 8.6 ± 0.7 mmol/l; p = NS) or for the control subjects (5.2 ± 0.1 vs 5.2 ± 0.1 mmol/l; p = NS). Duplication of the PG profile (Fig. 1) following the 50-g oral load (day 1) was obtained by i.v. infusion of 44.3 ± 1.9 and 21.3 ± 0.8 g of glucose (p < 0.0001) on day 2 in the patients with type 2 diabetes and in the control subjects, respectively. No significant differences between the plasma glucose curves within each group were observed. Peak values for the patients with type 2 diabetes amounted to 15.9 ± 0.8 and 16.2 ±0.7 mmol/l on day 1 and 2, respectively (p = NS). In the control subjects, PG peaked earlier and amounted to 9.5 ± 0.5 and 10.1 ± 0.4 mmol/l on the 2 days (p = NS). The AUCs for glucose for day 1 and 2, respectively, were significantly higher among the patients with type 2 diabetes than among control subjects (Table 1).
Glucagon
In the control group, fasting levels of plasma glucagon were 7.5 ± 0.4 and 7.8 ± 0.5 pmol/l on day 1 and 2, respectively (p = NS), whereas the corresponding values in the patients with type 2 diabetes were significantly higher (10.1 ± 0.6, p < 0.001 and 10.3 ± 0.5 pmol/l, p = 0.002, respectively,) with no significant difference between day 1 and 2. In the control group equal suppression of plasma glucagon concentrations (Fig. 2) was observed on both experimental days (p = NS) with similar nadirs of 4.9 ± 0.4 and 5.0 ± 0.5 pmol/l following OGTT and isoglycaemic i.v. glucose infusion, respectively, (p = NS). In the patients with type 2 diabetes, complete lack of suppression of plasma glucagon was observed during the first 45 min after the glucose load (OGTT), with an increase to a maximum concentration of 10.6 ± 0.8 pmol/l occurring 15 min after initiation of the OGTT. Then the plasma concentrations dropped to fasting levels at 45 min and to a nadir of 6.5 ± 0.6 pmol/l at 150 min, subsequently increasing to near-basal levels towards the end of the experiment (8.0 ± 0.6 pmol/l). During day 2, immediately after initiation of the isoglycaemic i.v. glucose infusion, the plasma glucagon concentration was suppressed with a nadir of 6.4 ± 0.5 pmol/l occurring at 120 min (Fig. 2a). The significantly (p = 0.007) diverging curves in the patients with type 2 diabetes resulted in a significant difference between AUCs for plasma glucagon on the two days (−498 ± 134 vs −771 ± 155 mmol/l × 4 h; p = 0.02); moreover, an even more pronounced difference was observed during the initial 45 min of days 1 and 2 (10 ± 16 vs −63 ± 21 mmol/l × 45 min; p = 0.002) (Fig. 2b). A significantly larger integrated glucagon response among patients with type 2 diabetes than among the control subjects was evident during day 1 (p = 0.03), but no significant differences between the two groups was observed during day 2.
a Plasma glucagon concentrations during OGTT (filled symbols) and isoglycaemic i.v. glucose infusion (open symbols), respectively, in patients with type 2 diabetes (dark green curves, diamonds) and in healthy control subjects (light green curves, circles). b Incremental values for plasma glucagon during the initial 45 min of OGTT (coloured bars) and isoglycaemic i.v. glucose infusion (open bars) in healthy control subjects and in patients with type 2 diabetes. * p < 0.05
Insulin, C-peptide, incretin effect and HOMA
There were no statistically significant differences between fasting values on day 1 and day 2 for plasma insulin or C-peptide for the two groups (Fig. 1). Maximum concentrations of both hormones were attained earlier in the control subjects than in the patients with type 2 diabetes. In both groups AUCs differed significantly between day 1 and 2 for insulin and C-peptide (Table 1). A significant difference between the positive incremental AUC for insulin was observed between the groups during day 1 (p = 0.03), but during day 2 no difference could be shown (p = NS). However, AUCs for insulin and C-peptide during the initial 45 min were significantly (p < 0.05) higher in the control subjects than in the patients with type 2 diabetes, both after oral and after i.v. glucose, respectively (data not shown).
Based on plasma insulin concentrations, the incretin effect amounted to 43 ± 16% in the patients with type 2 diabetes and 83 ± 6% in the control subjects (p = 0.03). The corresponding values calculated from plasma C-peptide concentrations were 36 ± 9 and 64 ± 7% (p = 0.02). Incretin effects based on glucose ingested during the OGTT and glucose infused during the isoglycaemic i.v. clamp amounted to 11 ± 4 and 57 ± 2% (p < 0.00001) in the two groups, respectively.
HOMAIR differed with borderline significance between the two groups (1.3 ± 0.2 for patients with type 2 diabetes vs 2.3 ± 0.5 for control subjects; p = 0.07).
GLP-1
Time courses for both total and intact GLP-1 are shown in Fig. 3. No significant differences in basal and stimulated values between the two groups were observed. In both groups total and intact GLP-1 responses were evident on day 1 (p < 0.05), whereas no significant responses (flat lines) of total or intact GLP-1 were observed during the isoglycaemic i.v. glucose administration in the two groups. In both groups AUCs for total and intact GLP-1 were significantly greater on day 1 than on day 2 (Table 1), but no differences between the two groups were found (p = NS).
Total glucose-dependent insulinotropic polypeptide (GIP) (a), intact GIP (c), total glucagon-like peptide 1 (GLP-1) (b) and intact GLP-1 (d) plasma concentrations during OGTT (filled symbols) and isoglycaemic i.v. glucose infusion (open symbols), respectively, in patients with type 2 diabetes (dark green curves, diamonds) and in healthy control subjects (light green curves, circles)
GIP
Time courses for total and intact plasma concentrations of GIP are shown in Fig. 3. No significant differences in basal values between the two groups were observed. Brisk increases of both total and intact GIP concentrations were observed in both groups following glucose ingestion (day 1). No significant responses (flat lines) of total or intact GIP were observed during isoglycaemic i.v. glucose administration in either group. In both groups the AUC for total GIP was significantly greater on day 1 than on day 2, as were the AUCs for intact GIP (Table 1). A significantly reduced incremental AUC for total GIP was observed among the patients compared with the healthy control subjects (p = 0.048; Table 1) but the absolute AUCs were not different (9.4 ± 0.9 vs 10.3 ± 1.0 nmol/l×4 h; p = NS).
Discussion
In the present study we report that inappropriate glucagon suppression in patients with type 2 diabetes occurs following oral ingestion of glucose, but not following isoglycaemic i.v. administration.
It is well established that both fasting hyperglucagonaemia and reduced postprandial glucagon suppression result in increased hepatic glucose production contributing to the hyperglycaemia characterising patients with type 2 diabetes [5–8]. Glucagon secretion has previously been observed to paradoxically increase after oral glucose or to exhibit exaggerated increases after meal ingestion in these patients [1–4]. This pathophysiological trait has been considered to represent an alpha-cell-specific islet defect [9] involving loss of alpha cell responsiveness to glucose and/or lack of insulin-induced suppression within the pancreatic islets. Studies on glucagon responses during intravenous glucose tolerance tests in patients with diabetes are scarce [30]; moreover, due to varying glucose concentrations during the experiments, the results are difficult to interpret. To our knowledge, reports on glucagon secretion during isoglycaemic clamp experiments have not been published previously, either for healthy subjects or for patients with type 2 diabetes.
How can the loss of initial inhibition during OGTT as opposed to normal suppression during isoglycaemic i.v. infusion be explained? We can rule out differences in PG concentrations under the two conditions since the PG curve during the OGTT was copied successfully during the second experimental day. According to the intra-islet insulin hypothesis, glucagon secretion is suppressed as a consequence of glucose-induced insulin release from the beta-cell-enriched core of the islets of Langerhans [31–35]. Nevertheless, the inappropriate suppression of glucagon observed in the patients with type 2 diabetes occurred during OGTT when insulin secretion was significantly higher (although reduced compared with control subjects) than during isoglycaemic i.v. glucose infusion (Fig. 1). Therefore, differences in beta cell secretion during the two experimental days do not seem to explain the delayed suppression of glucagon secretion in patients with type 2 diabetes. GLP-1 has been shown to be glucagonostatic [11], whereas the other incretin hormone, GIP, has been shown to enhance glucagon secretion particularly during the initial phase of GIP administration in patients with type 2 diabetes [10, 12, 17, 36]. In the present study, robust responses of both incretin hormones occurred during the OGTT in both groups (p = NS) and in neither of the groups were significant responses evident during the isoglycaemic i.v. glucose infusion. Thus, differences in total or intact GLP-1 and GIP responses, respectively, do not explain the findings. The glucagon-suppressive effect of GLP-1 has been found to be preserved in patients with type 2 diabetes [37], but in that study supraphysiological doses of GLP-1 were used, and it is possible that a decreased alpha cell sensitivity to GLP-1, similar to the decreased beta cell sensitivity to GLP-1 in type 2 diabetes, contributes to the lack of glucagon suppression. The other L-cell hormone, GLP-2, which is secreted in parallel with GLP-1, has been shown to cause increased alpha cell secretion without affecting insulin secretion [38–40]. We did not measure GLP-2 in these studies, but given that GLP-2 is co-secreted from the L-cell in equimolar amounts with GLP-1 [41, 42], and in these experiments with no apparent difference between the control subjects and the patients, it is unlikely that an increased secretion of GLP-2 could be responsible for reduced glucagon suppression during OGTT in patients with type 2 diabetes. However, abnormal alpha cell sensitivity to GLP-2 might theoretically be involved.
In healthy subjects we suggest that the normal glucagon response to an OGTT consists of a glucose-induced inhibition of alpha cell secretion, which is modulated by the release and stimulatory actions of GIP and GLP-2, thus counteracting the glucagonostatic effects of GLP-1 and the inhibitory effects of increased intra-islet insulin, but still resulting in an equal suppression compared to the less insulinotropic i.v. stimulus. In type 2 diabetes the lost glucagon response during OGTT might be explained by an imbalance between the glucagonotropic effects of GIP and GLP-2 on the one hand, and the glucagonostatic effects of GLP-1 and increased intra-islet insulin on the other. In type 2 diabetes, the beta cell is resistant to GIP and insensitive to GLP-1 [17, 43] and therefore less insulin is secreted. Furthermore, the alpha cells seem to respond more readily to the stimulatory actions at least of GIP. Indeed, in hyperglycaemic clamp experiments in patients with type 2 diabetes, glucagon secretion was inadequately suppressed by glucose and paradoxically increased above basal by GIP [17, 36]. Clearly, further studies are needed to confirm the possible role of GIP and perhaps GLP-2 as mediators of the paradoxical glucagon responses during OGTT in patients with type 2 diabetes.
When we gauged the incretin effect by comparing the amount of intravenous glucose required to copy the PGOGTT curve, the incretin effect was almost completely lost in the patients, whereas a comparison of insulin responses indicates that the incretin effect was reduced from 83 to 43%. We propose that the abnormal glucagon suppression during the OGTT is responsible for this difference. Thus, the dampened glucagon suppression during OGTT compared with isoglycaemic i.v. glucose infusion would be expected to result in inadequate suppression of hepatic glucose production pulling the PG curve upwards. This, in turn, means that an increased amount of glucose is required to obtain isoglycaemic glucose excursions during i.v. infusion, eventually approaching the amount of glucose given orally.
Thus, the diabetic intolerance to oral glucose appears to include not only an inadequate amplification of insulin secretion by the incretin hormones GIP and GLP-1, but also a lack of suppression or a frank elevation of glucagon secretion, possibly induced by GIP (and possibly GLP-2), which is not observed in healthy subjects.
In summary, the present study confirms the observation made by Nauck and colleagues in 1986 that the incretin effect is reduced in patients with type 2 diabetes [13], and it seems that the explanation for this deficiency is not to be found in the response of the incretin hormones to oral or isoglycaemic i.v. glucose. In addition, we report the novel finding that in patients with type 2 diabetes glucagon is suppressed in a normal fashion during isoglycaemic i.v. glucose infusion, whereas the suppression is dampened during oral ingestion of glucose. The mechanism of this phenomenon is currently unclear, but there is little doubt that this inappropriate glucagon suppression contributes to the glucose intolerance and the reduced incretin effect in patients with type 2 diabetes, when estimated by comparing the amounts of glucose given orally and intravenously during isoglycaemic glucose challenges.
Abbreviations
- FPG:
-
fasting plasma glucose
- GIP:
-
glucose-dependent insulinotropic polypeptide
- GLP-1:
-
glucagon-like peptide-1
- HOMA:
-
homeostatic model assessment
- HOMAIR :
-
assessment of insulin resistance by homeostatic model assessment
- PG:
-
plasma glucose
- PG120 min :
-
plasma glucose concentration at 120 min after 75-g OGTT
References
Muller WA, Faloona GR, Aguilar-Parada E, Unger RH (1970) Abnormal alpha-cell function in diabetes. Response to carbohydrate and protein ingestion. N Engl J Med 283:109–115
Reaven GM, Chen YD, Golay A, Swislocki AL, Jaspan JB (1987) Documentation of hyperglucagonemia throughout the day in nonobese and obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 64:106–110
Unger RH, Orci L (1981) Glucagon and the A cell: physiology and pathophysiology (first of two parts). N Engl J Med 304:1518–1524
Unger RH, Orci L (1981) Glucagon and the A cell: physiology and pathophysiology (second of two parts). N Engl J Med 304:1575–1580
Baron AD, Schaeffer L, Shragg P, Kolterman OG (1987) Role of hyperglucagonemia in maintenance of increased rates of hepatic glucose output in type-II diabetics. Diabetes 36:274–283
Dinneen S, Alzaid A, Turk D, Rizza R (1995) Failure of glucagon suppression contributes to postprandial hyperglycaemia in IDDM. Diabetologia 38:337–343
Mitrakou A, Kelley D, Veneman T et al (1990) Contribution of abnormal muscle and liver glucose metabolism to postprandial hyperglycemia in NIDDM. Diabetes 39:1381–1390
Shah P, Vella A, Basu A, Basu R, Schwenk WF, Rizza RA (2000) Lack of suppression of glucagon contributes to postprandial hyperglycemia in subjects with type 2 diabetes mellitus. J Clin Endocrinol Metab 85:4053–4059
Ipp E (2000) Impaired glucose tolerance: the irrepressible alpha-cell? Diabetes Care 23:569–570
Holst JJ (2004) On the physiology of GIP and GLP-1. Horm Metab Res 36:747–754
Nauck MA, Kleine N, Orskov C, Holst JJ, Willms B, Creutzfeldt W (1993) Normalization of fasting hyperglycaemia by exogenous glucagon-like peptide 1 (7–36 amide) in type 2 (non-insulin-dependent) diabetic patients. Diabetologia 36:741–744
Meier JJ, Gallwitz B, Siepmann N et al (2003) Gastric inhibitory polypeptide (GIP) dose-dependently stimulates glucagon secretion in healthy human subjects at euglycaemia. Diabetologia 46:798–801
Nauck M, Stockmann F, Ebert R, Creutzfeldt W (1986) Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 29:46–52
Toft-Nielsen MB, Damholt MB, Madsbad S et al (2001) Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab 86:3717–3723
Vilsboll T, Krarup T, Deacon CF, Madsbad S, Holst JJ (2001) Reduced postprandial concentrations of intact biologically active glucagon-like peptide 1 in type 2 diabetic patients. Diabetes 50:609–613
Kjems LL, Holst JJ, Volund A, Madsbad S (2003) The influence of GLP-1 on glucose-stimulated insulin secretion -- effects on beta-cell sensitivity in type 2 and nondiabetic subjects. Diabetes 52:380–386
Vilsboll T, Krarup T, Madsbad S, Holst JJ (2002) Defective amplification of the late phase insulin response to glucose by GIP in obese type II diabetic patients. Diabetologia 45:1111–1119
No authors listed (2002) Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 25(Suppl 1):S5–S20
Alberti KGMM, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications part 1: Diagnosis and classification of diabetes mellitus -- Provisional report of a WHO consultation. Diabet Med 15:539–553
Orskov C, Rabenhoj L, Wettergren A, Kofod H, Holst JJ (1994) Tissue and plasma concentrations of amidated and glycine-extended glucagon-like peptide-1 in humans. Diabetes 43:535–539
Vilsboll T, Krarup T, Sonne J et al (2003) Incretin secretion in relation to meal size and body weight in healthy subjects and people with type 1 and type 2 diabetes mellitus. J Clin Endocrinol Metab 88:2706–2713
Krarup T, Holst JJ (1984) The heterogeneity of gastric inhibitory polypeptide in porcine and human gastrointestinal mucosa evaluated with five different antisera. Regul Pept 9:35–46
Krarup T, Madsbad S, Moody AJ et al (1983) Diminished immunoreactive gastric inhibitory polypeptide response to a meal in newly diagnosed type I (insulin-dependent) diabetics. J Clin Endocrinol Metab 56:1306–1312
Deacon CF, Nauck MA, Meier J, Hucking K, Holst JJ (2000) Degradation of endogenous and exogenous gastric inhibitory polypeptide in healthy and in type 2 diabetic subjects as revealed using a new assay for the intact peptide. J Clin Endocrinol Metab 85:3575–3581
Kjems LL, Christiansen E, Volund A, Bergman RN, Madsbad S (2000) Validation of methods for measurement of insulin secretion in humans in vivo. Diabetes 49:580–588
Orskov C, Jeppesen J, Madsbad S, Holst JJ (1991) Proglucagon products in plasma of noninsulin-dependent diabetics and nondiabetic controls in the fasting state and after oral glucose and intravenous arginine. J Clin Invest 87:415–423
Baldissera FGA, Holst JJ (1984) Glucagon-related peptides in the human gastrointestinal mucosa. Diabetologia 26:223–228
Holst JJ, Pedersen JH, Baldissera F, Stadil F (1983) Circulating glucagon after total pancreatectomy in man. Diabetologia 25:396–399
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Aronoff SL, Bennett PH, Unger RH (1977) Immunoreactive glucagon (Irg) responses to intravenous glucose in prediabetes and diabetes among pima Indians and normal Caucasians. J Clin Endocrinol Metab 44:968–972
Banarer S, McGregor VP, Cryer PE (2002) Intraislet hyperinsulinemia prevents the glucagon response to hypoglycemia despite an intact autonomic response. Diabetes 51:958–965
Gerich JE, Langlois M, Noacco C, Karam JH, Forsham PH (1973) Lack of glucagon response to hypoglycemia in diabetes -- evidence for an intrinsic pancreatic alpha cell defect. Science 182:171–173
Meier JJ, Kjems LL, Veldhuis JD, Lefebvre P, Butler PC (2006) Postprandial suppression of glucagon secretion depends on intact pulsatile insulin secretion -- further evidence for the intraislet insulin hypothesis. Diabetes 55:1051–1056
Samols E, Stagner JI, Ewart RBL, Marks V (1988) The order of islet microvascular cellular perfusion is β–α–δ in the perfused rat pancreas. J Clin Invest 82:350–353
Zhou HR, Tran POT, Yang SL et al (2004) Regulation of alpha-cell function by the beta-cell during hypoglycemia in Wistar rats: the “switch-off” hypothesis. Diabetes 53:1482–1487
Nauck MA, Heimesaat MM, Orskov C, Holst JJ, Ebert R, Creutzfeldt W (1993) Preserved incretin activity of glucagon-like peptide 1 [7–36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest 91:301–307
Nauck MA, Kleine N, Orskov C, Holst JJ, Willms B, Creutzfeldt W (1993) Normalization of fasting hyperglycemia by exogenous glucagon-like peptide-1 (7–36 amide) in type-2 (non-insulin-dependent) diabetic-patients. Diabetologia 36:741–744
Meier JJ, Nauck MA, Pott A et al (2006) Glucagon-like peptide 2 stimulates glucagon secretion, enhances lipid absorption, and inhibits gastric acid secretion in humans. Gastroenterology 130:44–54
Schmidt WE, Siegel EG, Creutzfeldt W (1985) Glucagon-like peptide-1 but not glucagon-like peptide-2 stimulates insulin release from isolated rat pancreatic-islets. Diabetologia 28:704–707
Sorensen LB, Flint A, Raben A, Hartmann B, Holst JJ, Astrup A (2003) No effect of physiological concentrations of glucagon-like peptide-2 on appetite and energy intake in normal weight subjects. Int J Obes 27:450–456
Bell GI, Santerre RF, Mullenbach GT (1983) Hamster preproglucagon contains the sequence of glucagon and 2 related peptides. Nature 302:716–718
Orskov C, Holst JJ, Khuhtsen S, Baldissera FGA, Poulsen SS, Nielsen OV (1986) Glucagon-like peptides Glp-1 and Glp-2, predicted products of the glucagon gene, are secreted separately from pig small-intestine but not pancreas. Endocrinology 119:1467–1475
Vilsboll T, Knop FK, Krarup T et al (2003) The pathophysiology of diabetes involves a defective amplification of the late-phase insulin response to glucose by glucose-dependent insulinotropic polypeptide -- regardless of etiology and phenotype. J Clin Endocrinol Metab 88:4897–4903
Acknowledgements
We are grateful to our volunteers, whose availability made this work possible, and to L. Bagger, B. Bischoff, N. Kjeldsen, J. Purtoft and S. Reimer for technical assistance. This study was supported by unrestricted grants from the Danish Medical Research Council and Else and Svend Madsen’s Foundation.
Duality of interest
None of the authors have any financial interests that might conflict with this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Knop, F.K., Vilsbøll, T., Madsbad, S. et al. Inappropriate suppression of glucagon during OGTT but not during isoglycaemic i.v. glucose infusion contributes to the reduced incretin effect in type 2 diabetes mellitus. Diabetologia 50, 797–805 (2007). https://doi.org/10.1007/s00125-006-0566-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0566-z