Abstract
Aims/hypothesis
Obesity is an independent risk factor for heart diseases but the underlying mechanism is not clear. This study examined cardiac contraction, oxidative stress, oxidative modification of sarco(endo)plasmic reticulum Ca2+-ATPase (SERCA) and the myosin heavy chain (MHC) isoform switch in obese mice.
Methods
Mechanical properties were evaluated in ventricular myocytes from C57BL/6J lean and Lep/Lep obese mice (formerly known as ob/ob mice), including peak shortening (PS), time to 50 or 90% PS, time to 50 or 90% relengthening (TR50, TR90), maximal velocity of shortening/relengthening (±dL/dt), intracellular Ca2+ and its decay (τ). Oxidative stress, lipid peroxidation, protein damage and SERCA activity were assessed by glutathione/glutathione disulfide, malondialdehyde, protein carbonyl and 45Ca2+ uptake, respectively. NADPH oxidase was determined by immunoblotting.
Results
Myocytes from Lep/Lep mice displayed depressed PS and ± dL/dt, prolonged TR50, TR90, elevated resting [Ca2+]i, prolonged τ, reduced contractile capacity at high stimulus frequencies and diminished responsiveness to extracellular Ca2+ compared with lean controls. Cardiac glutathione/glutathione disulfide was decreased whereas malondialdehyde, protein carbonyl, membrane p47phox and membrane gp91phox were increased in the Lep/Lep group. SERCA isoenzyme 2a was markedly modified by oxidation in Lep/Lep hearts and associated with decreased 45Ca2+ uptake. The MHC isozyme displayed a shift from the α to the β isoform in Lep/Lep hearts. Short-term incubation of angiotensin II with myocytes mimicked the mechanical defects, SERCA oxidation and 45Ca2+ uptake seen in Lep/Lep myocytes. Incubation of the NADPH oxidase inhibitor apocynin with Lep/Lep myocytes alleviated contractile defects without reversing SERCA oxidation or activity.
Conclusions/interpretation
These data indicate that obesity-related cardiac defects may be related to NADPH oxidase activation, oxidative damage to SERCA and the MHC isozyme switch.
Similar content being viewed by others
Introduction
An emerging theme in obesity is the presence of compromised ventricular function [1, 2]. Cardiovascular regulation of the obese gene product leptin has attracted much attention because its deficiency or resistance leads to obesity and cardiovascular problems [3–6]. Leptin receptors exist in cardiomyocytes and are coupled to the signalling pathways regulating myocardial contractility [6, 7] and cellular growth [5, 8]. Mice lacking leptin (Lep/Lep, formerly known as ob/ob) or its receptor (Lepr/Lepr, formerly known as db/db) develop cardiac hypertrophy and contractile dysfunction, consolidating a role for leptin in the maintenance of cardiac architecture and function [5, 9, 10].
Oxidative stress is a major risk factor for ventricular hypertrophy and endothelial dysfunction [3, 11, 12]. Although intracellular reactive oxygen species (ROS) are essential for optimal insulin sensitisation [13], excessive oxidative stress initiates an NADPH oxidase-mediated reduction in nitric oxide bioavailability and endothelial dysfunction in obesity [14, 15]. Defects in oxidative capacity alter cardiac function through decreased sarco(endo)plasmic reticulum Ca2+-ATPase (SERCA) isozyme 2a (SERCA2a) activity and the redistribution of myosin heavy chain (MHC) isozymes [16–18]. Alterations in MHC isozymes have been reported in obesity-related respiratory complications, which may be attenuated by leptin repletion [19, 20]. Although leptin is considered an essential player in obesity and diabetes [4, 11], the cellular mechanism(s) responsible for cardiac dysfunction in leptin-deficient obesity have not been elucidated. The aim of our study was to evaluate cardiomyocyte function, oxidative stress, lipid peroxidation, NADPH oxidase, oxidative modification of the key Ca2+ regulating protein SERCA and MHC isozyme distribution in leptin-deficient Lep/Lep obese mice.
Materials and methods
Experimental animals and intraperitoneal glucose tolerance test
All procedures described here were approved by our institutional animal care and use committee. Male homozygous B6.V-lep<Lep>/J Lep/Lep mice were purchased from the Jackson Laboratory (Bar Harbor, ME, USA) at 3 weeks of age and were housed within our animal facility until 9 weeks of age. Age-matched wild-type C57BL/6J mice were used as controls. Mice were allowed free access to water and lab chow. A glucose tolerance test was conducted in mice fasted for 12 h by intraperitoneal injection of glucose (2 g/kg body weight). Glucose levels were determined immediately before challenge and 15, 30, 60 and 120 min thereafter [21].
Cell isolation, short-term culture, cell shortening and intracellular Ca2+ measurement
Cardiomyocytes were isolated enzymatically as described [22]. Cohorts of cardiomyocytes from lean or Lep/Lep mice were incubated with angiotensin II (100 nmol/l), apocynin (100 μmol/l) or both for 4 h. Mechanical and intracellular Ca2+ properties were assessed using edge detection and fura-2 (0.5 μmol/l). Cell shortening and relengthening were assessed using the following indices: peak shortening (PS), times to 50 and 90% PS (TPS50 and TPS90), times to 50 and 90% relengthening (TR50 and TR90), and maximal velocity of shortening/relengthening (±dL/dt). Qualitative changes in intracellular Ca2+ were inferred from the ratio of fura-2 fluorescence intensities at two wavelengths (360 and 380 nm). Fluorescence decay time (τ) was measured to indicate the intracellular Ca2+ clearance rate [2, 22].
Glutathione and glutathione disulfide assay
Glutathione levels were determined as an indicator of oxidative stress [22]. Samples were homogenised in four volumes (w/v) of 1% picric acid and centrifuged at 16,000 ×g (30 min). Supernatant fractions were assayed for total glutathione (GSH) and glutathione disulfide (GSSG) by the standard recycling method. GSH was determined using a standard curve and GSSG was measured with 4-vinyl pyridine. The GSSG (as GSH ×2) was then subtracted from the total GSH to determine the actual GSH level.
Measurement of lipid peroxidation
Hearts were homogenised in ice-cold phosphate-buffered saline (20 mmol/l) containing protease inhibitor cocktail. The homogenate was centrifuged (3,000 ×g, 10 min at 4°C) and the supernatant was used for assay according to a Bioxytech LPO-586 kit (Oxis, Portland, OR, USA) [23].
Quantification of protein carbonyl
Protein was precipitated by adding an equal volume of 20% trichloroacetic acid and centrifuged at 11,000 ×g for 1 min. The sample was resuspended in 10 mmol/l 2,4-dinitrophenylhydrazine (2,4-DNPH) solution for 15–30 min at room temperature before 20% trichloroacetic acid was added and samples were centrifuged (11,000 ×g) for 3 min. The precipitate was resuspended in 6 mol/l guanidine solution. The maximum absorbance (360–390 nm) was read against appropriate blanks (2 mol/l HCl) and carbonyl content was calculated using the formula: absorption at 360 nm×45.45 nmol/protein content (mg) [22].
MHC isoform analysis by gel electrophoresis
Briefly, homogenised heart tissue in sample buffer (1:30) was heated for 2 min at 95°C and chilled on ice for 5 min before being centrifuged. Three microlitres of 1:10 diluted supernatant was loaded for electrophoresis [24]. The methods for gels and the running conditions were identical to those described by Reiser and Kline [25]. After running, gels were fixed for a minimum of 2 h in 5% glutaraldehyde before being silver-stained and scanned with a calibrated densitometer (GS-800; Bio-Rad, Hercules, CA, USA) to determine the amounts of MHC-α and MHC-β.
Western blot analysis of NADPH oxidase subunit expression and distribution
Subcellular fractions of myocytes were prepared using the Cell Compartment Kit Fractionation Procedure (Qiagen, Valencia, CA, USA). Western blot analysis of NADPH oxidase subunits was performed on cytosolic and membrane protein fractions. Samples were separated on 10% SDS–polyacrylamide gels and transferred to nitrocellulose membranes. The membranes were blocked with 5% milk and were incubated with β-actin and antibodies to NADPH oxidase subunits gp91phox and p47phox. The film was scanned and the intensity of immunoblot bands was detected with a calibrated densitometer (Bio-Rad) [22].
SERCA isoenzyme 2a immunoprecipitation and protein carbonyl immunoprobing
Cardiomyocytes were sonicated and solubilised in a buffer containing 0.5% CHAPS (3-[(3-cholamidopropyl)dimethylammonio]-1-propanesulfonate; 1 mg CHAPS/100 μg protein), 10 mmol/l Tris–HCl (pH 7.4), 50 mmol/l dithiothreitol, 0.3 mol/l sucrose, with protease inhibitors at 4°C. After centrifugation (6,000 ×g, 10 min), antibody to sarco(endo)plasmic reticulum Ca2+-ATPase isozyme 2a (SERCA2a) (Affinity BioReagent, Denver, CO, USA) was added to the supernatant and incubated overnight at 4°C. An IgG–agarose slurry was added and rotary-mixed at 4°C for 2 h. Oxidised SERCA2a was probed immunochemically after derivatisation with dinitrophenylhydrazine [26]. Total SERCA2a expression after immunoprecipitation was quantified and was used to normalise protein loading.
SERCA activity measured by 45Ca2+ uptake
Cardiomyocytes were sonicated and solubilised in a Tris–sucrose homogenisation buffer consisting of 30 mmol/l Tris–HCl, 8% sucrose, 1 mmol/l phenylmethylsulfonylfluoride and 2 mmol/l dithiothreitol, pH 7.1. To determine SERCA-dependent Ca2+ uptake, samples were treated with and without 10 μmol/l of the SERCA inhibitor thapsigargin for 15 min. The difference between the two readings was deemed the thapsigargin-sensitive uptake through SERCA. Uptake was initiated by the addition of an aliquot of supernatant to a solution consisting of (mmol/l) 100 KCl, 5 NaN3, 6 MgCl2, 0.15 EGTA, 0.12 CaCl2, 30 Tris–HCl pH 7.0, 10 oxalate, 2 ATP and 1 μCi 45CaCl2 at 37°C. Aliquots of samples were injected onto glass filters on a suction manifold and washed three times. Filters were then removed from the manifold, placed in scintillation fluid and counted. SERCA activity was expressed as cpm/mg protein [27].
Statistical analysis
Data are expressed as mean ± SEM. Differences were assessed using ANOVA followed by the Newman–Keuls post hoc test. A p value less than 0.05 was considered statistically significant.
Results
General features of lean control and obese mice
The effects of obesity on body, organ weight, tibia length, glucose tolerance and blood pressure are shown in Table 1 and Fig. 1. Obesity increased the weights of the body and organs without affecting tibia length or systolic and diastolic blood pressures. The ratios of heart weight to tibia length and liver weight to tibia length were significantly higher in Lep/Lep mice. The ratio of kidney weight to tibia length was not different between lean and obese mice. Obesity moderately but significantly elevated the fasting blood glucose levels in conjunction with glucose intolerance.
Mechanical properties of cardiomyocytes
Cardiomyocytes from obese mice exhibited significantly enlarged cross-sectional area and reduced contractile capacity, indicated by decreased PS and ±dL/dt compared with lean controls. Durations of relengthening (TR50 and TR90) were significantly prolonged and associated with normal duration of shortening (TPS50 and TPS90) in Lep/Lep myocytes (Fig. 2). Obesity led to elevated resting and peak [Ca2+]i, slowed intracellular Ca2+ decay (prolonged τ) and increased area underneath the fluorescence curve, an indication of compromised Ca2+ clearing. The electrically stimulated rise in [Ca2+]i was similar between the two groups (Fig. 3).
Contractile properties of ventricular myocytes from lean and Lep/Lep obese mouse hearts. a Representative cell shortening traces in lean control and Lep/Lep mouse myocytes. b Cross-sectional area. c Peak shortening normalised to resting cell length. d Maximal velocity of shortening/relengthening (±dL/dt). e Times to 50 and 90% peak shortening (TPS50 and TPS90, open and shaded bars, respectively). f Times to 50 and 90% relengthening (TR50 and TR90, open and shaded bars, respectively). Cardiomyocytes were electrically stimulated to contract at a frequency of 0.5 Hz with an extracellular Ca2+ level of 1.0 mmol/l. Mean±SEM, n=146 cells evenly distributed from six mice, *p<0.05 vs lean control
Intracellular Ca2+ transient properties of ventricular myocytes from lean and Lep/Lep obese mouse hearts. a Representative intracellular Ca2+ transients in lean and Lep/Lep mouse myocytes. b Resting intracellular Ca2+ levels. c Peak intracellular Ca2+ levels. d Electrically stimulated rise in intracellular Ca2+. e Intracellular Ca2+ decay rate (τ). f Area integration underneath Ca2+ fluorescence curve. Cardiomyocytes were electrically stimulated to contract at a frequency of 0.5 Hz with an extracellular Ca2+ level of 1.0 mmol/l. Mean±SEM, n=56 cells evenly distributed from four mice, *p<0.05 vs lean control
Effect of extracellular Ca2+ and stimulus frequency on myocyte shortening
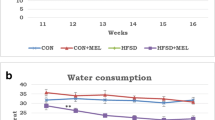
To examine the influence of extracellular Ca2+ levels on PS, myocytes were placed in a contractile buffer with 0.5 mmol/l CaCl2 before increasing extracellular Ca2+ levels to 1.0, 2.0 and 3.0 mmol/l, with a 5-min interval in between. Figure 4a shows that PS was not significantly different between lean and obese myocytes under 0.5 mmol/l Ca2+. Stepwise increases in extracellular Ca2+ resulted in increased PS in lean control myocytes. However, such a rise in PS was significantly dampened in Lep/Lep myocytes. The maximal PS (at 3 mmol/l Ca2+) was significantly less in Lep/Lep myocytes than in those of lean controls. These results suggest reduced myocyte responsiveness to extracellular Ca2+ and/or a diminished sarcoplasmic reticulum Ca2+ load under obesity. To evaluate the impact of obesity on cardiac function at higher pacing rates, cells were initially stimulated to contract at 0.5 Hz for 5 min to ensure a steady state before commencing the frequency response study. All recordings were normalised to PS at 0.1 Hz of the same myocyte. Figure 4b shows a steeper decline of PS in Lep/Lep myocytes with increasing stimulus frequency compared with lean control myocytes (with the exception of 3.0 Hz). These data indicate that Lep/Lep myocytes displayed reduced intracellular Ca2+ cycling or stress tolerance.
Effect of increased extracellular Ca2+ concentration (a) and field electrical stimulus frequency (b) on peak shortening (PS) amplitude in myocytes from lean (open symbols) and Lep/Lep obese (filled symbols) mouse hearts. For frequency response, PS is shown as percentage change from respective PS value obtained at 0.1 Hz. Mean±SEM, n=25–29 cells from four mice per group, *p<0.05 vs lean control
Effect of obesity on cardiac oxidative stress, lipid peroxidation level, protein carbonyl content and expression of MHC isozymes
Obesity is often associated with enhanced oxidative stress, leading to irreversible damage of proteins or lipids [14]. Figure 5a demonstrates that the GSH/GSSG ratio was significantly decreased, by ∼40%, in Lep/Lep heart. Similarly, lipid peroxidation and protein carbonyl formation were both significantly elevated in Lep/Lep hearts (Fig. 5b,c). It has been reported that expression of MHC isozymes is associated with cardiac function, especially in myocardial remodelling and cardiomyopathies [17, 28–31]. We examined the pattern of MHC isozyme distribution in Lep/Lep heart. The result shown in Fig. 6 revealed an MHC isozyme switch from α to β in Lep/Lep hearts. While MHC-α was the predominant isoform in lean hearts, the MHC-β content was significantly elevated in Lep/Lep hearts compared with the lean group (Fig. 6).
Role of NADPH oxidase in obesity-associated cardiac mechanical dysfunction
NADPH oxidase is a predominant source of ROS [32, 33]. Our earlier study revealed that angiotensin receptor-mediated activation of NADPH oxidase plays a role in hyperglycaemia-induced cardiac dysfunction [34]. To test whether the angiotensin II-NADPH oxidase cascade plays a role in obesity-induced cardiac dysfunction, lean and Lep/Lep myocytes were incubated with angiotensin II (100 nmol/l) or apocynin (100 μmol/l) for 4 h before the cell mechanics were evaluated. Data shown in Fig. 7 indicate that neither angiotensin II nor apocynin affected cell cross-sectional area in lean and Lep/Lep myocytes. Interestingly, apocynin blunted the obesity-induced reduction in PS, ±dL/dt and prolongation of TR90 in Lep/Lep myocytes without affecting cell mechanics in lean cells. On the contrary, angiotensin II mimicked the cardiomyocyte contractile phenotype of Lep/Lep myocytes to a great extent, an effect which was abolished by apocynin. TPS90 was not affected by either angiotensin II or apocynin. Surprisingly, co-incubation with both agents significantly shortened TPS90 in lean control myocytes, although the mechanism remains unknown. Apocynin and angiotensin II exhibited effects on TPS50 and TR50 similar to those of TPS90 and TR90 in lean and Lep/Lep myocytes (data not shown). These data suggest that angiotensin II and NADPH oxidase activation play important roles in the cardiac dysfunction observed in Lep/Lep obesity. To further elucidate the role of NADPH oxidase in obesity-associated cardiac dysfunction, levels of two major subunits of NADPH oxidase, gp91phox and p47phox, were examined in lean and Lep/Lep cardiomyocytes. Redistribution of NADPH oxidase subunits from cytosol onto membrane is considered a hallmark of NADPH oxidase activation [32]. Consistent with oxidative stress in Lep/Lep mouse hearts, the levels of p47phox and gp91phox were elevated in the membrane but not the cytosolic fraction of Lep/Lep myocytes or lean cells treated with angiotensin II. Apocynin attenuated elevated pg91phox distribution but not p47phox in Lep/Lep myocytes. Similarly, apocynin effectively antagonised angiotensin II-induced upregulation of NADPH oxidase subunits. Cytosolic NADPH oxidase was not affected by obesity, angiotensin II or apocynin (Fig. 8).
Contractile properties of lean and Lep/Lep obese cardiomyocytes incubated for 4 h with angiotensin II (AngII, 100 nmol/l), the NADPH oxidase inhibitor apocynin (Apo, 100 μmol/l) or both. a Cross-sectional area. b Peak shortening (PS) normalised to resting cell length. c Maximal velocity of shortening (+dL/dt). d Maximal velocity of relengthening (−dL/dt). e Time to 90% peak shortening (TPS90). f Time to 90% relengthening (TR90). Mean±SEM, n=84–88 cells from three mice per group, *p<0.05 vs lean control, #p<0.05 vs respective apocynin-free group
NADPH oxidase expression and distribution in cytosolic and membrane fractions of lean and Lep/Lep obese mouse myocytes with or without treatment with angiotensin II (AngII, 100 nmol/l) or apocynin (Apo, 100 μmol/l). a, b The p47phox subunit of NADPH oxidase in cytosolic and membrane fractions. c, d The gp91phox subunit of NADPH oxidase in cytosolic and membrane fractions. Insets: representative immunoblots using specific antibodies against p47phox and gp91phox subunits. Mean±SEM, n=6, *p<0.05 vs lean control, #p<0.05 vs angiotensin II treatment group
Effect of obesity on SERCA2a oxidation and SERCA activity
Persistent oxidative stress leads to oxidative damage to proteins such as SERCA [27, 35, 36]. Given that protein carbonyl formation, a fundamental measure of oxidative damage in cardiac proteins [22, 37], is elevated in Lep/Lep heart, we evaluated oxidative damage to SERCA2a by quantitative immunoprecipitation of SERCA2a from cell lysates using specific SERCA2a antibody followed by immunoprobe of the protein carbonyl content. The total expression of immunoprecipitated SERCA2a proteins did not differ among lean myocytes, Lep/Lep myocytes and cells treated with apocynin or angiotensin. Interestingly, the levels of oxidised SERCA2a (both absolute abundance and the level normalised to total SERCA2a) were significantly increased in Lep/Lep myocytes and lean control myocytes treated with angiotensin II. Apocynin did not affect the oxidative modification SERCA2a in either the lean or the Lep/Lep group. Interestingly, the angiotensin II-elicited increase in SERCA2a oxidative modification was significantly attenuated by apocynin (Fig. 9). Consistent with enhanced SERCA2a oxidative modification in Lep/Lep myocytes, SERCA activity was significantly reduced in myocytes from Lep/Lep mice. Angiotensin II treatment suppressed SERCA activity in lean control myocytes to a similar extent. Somewhat surprisingly, apocynin did not exhibit any affect on the reduced SERCA activity in Lep/Lep myocytes whereas it significantly attenuated angiotensin II-induced reduction in SERCA activity (Fig. 10).
Oxidative modification of SERCA2a protein in lean and Lep/Lep obese mouse myocytes with or without treatment with angiotensin II (AngII, 100 nmol/l) or apocynin (Apo, 100 μmol/l). a Total SERCA2a expression. b Oxidative modification of SERCA2a detected by immunoprecipitation followed by protein carbonyl immunoprobing. c Oxidised SERCA2a normalised to total SERCA2a abundance. Mean±SEM, n=6, *p<0.05 vs lean control, #p<0.05 vs angiotensin II treatment
Discussion
This study demonstrated that Lep/Lep obesity is associated with cardiomyocyte dysfunction and intracellular Ca2+ mishandling, manifested as reduced contractile capacity and maximal velocity of contraction/relaxation, prolonged relaxation, elevated resting intracellular Ca2+ levels, slowed intracellular Ca2+ extrusion, impaired responsiveness to extracellular Ca2+ and diminished contractile capacity at higher stimulus frequencies. In addition, elevated oxidative stress, lipid peroxidation and protein carbonyl formation were observed in Lep/Lep hearts in conjunction with activation of NADPH oxidase. Our further evidence indicated overt oxidative modification to SERCA2a, diminished SERCA activity and MHC isozyme switch in Lep/Lep obesity. The fact that apocynin abolished the cardiac contractile defect and pg91phox subunit membrane distribution in Lep/Lep myocytes supports a role of NAPDH oxidase in obesity-associated cardiac dysfunction. However, the observation that apocynin fails to reverse obesity-induced oxidative modification of SERCA2a and reduced 45Ca2+ uptake indicates that SERCA modification may not be reversed with short-term apocynin treatment. It is also possible that SERCA may not be a permissive player downstream of NADPH oxidase activation en route to cardiac mechanical defects in Lep/Lep obesity.
Leptin deficiency in Lep/Lep mice is associated with obesity, insulin resistance and mild to moderate diabetes [38, 39]. The 9-week-old Lep/Lep mice used in our study exhibited impaired glucose tolerance, indicative of prediabetic insulin resistance. Tibia length was similar between the lean and Lep/Lep mice, excluding potential contribution from developmental factor. Cardiac hypertrophy has been shown in Lep/Lep hearts from 8- and 12-week-old mice [40, 41], in agreement with our observation of increased absolute heart weight, ratio of heart weight to tibia length and enlarged cross-sectional area of myocytes. Myocardial remodelling is a critical factor in the transition of the heart from a compensated to a decompensated state and may contribute to compromised cardiac function and the MHC isozyme switch [42]. Reduced contractile capacity and prolonged duration of relaxation have been indicated in obesity and type 2 diabetes [2, 16]. Our present study demonstrated a larger cross-sectional area of the cells, reduced PS, lessened ±dL/dt and prolonged TR50/TR90 in association with normal TPS50/TPS90, compared with lean control myocytes. Consistently, myocytes from Lep/Lep mice showed elevated resting and peak [Ca2+]i, prolonged τ, increased area integration underneath the intracellular Ca2+ fluorescence curve, reduced contractile capacity at higher field stimulus frequency, and reduced responsiveness to extracellular [Ca2+]. Several mechanisms may be postulated for obesity-associated defects in Lep/Lep cardiac contractility and intracellular Ca2+ handling. It has been reported that prolonged duration of relaxation may simply be a consequence of impaired SERCA and Na+/Ca2+ exchanger function [43]. This is supported by enhanced SERCA oxidative modification, reduced 45Ca2+ uptake and slowed intracellular Ca2+ clearing rate (τ) in Lep/Lep mouse cardiomyocytes. The prolongation of both TR50 and TR90 seen in Lep/Lep myocytes indicates defects in both the rapid phase (usually controlled by SERCA) and the slow phase (controlled by Na+/Ca2+ exchanger, sarcolemmal and mitochondrial Ca2+ pumps) of diastole. Our study revealed depressed myocyte shortening ability associated with a normal increase in intracellular Ca2+ in response to electrical stimuli in Lep/Lep myocytes. This discrepancy may be attributed to reduced myofilament Ca2+ sensitivity and MHC isozyme switch in the Lep/Lep group. Our data indicate that the contractile response of myocytes to increased extracellular Ca2+ was reduced in Lep/Lep mouse myocytes, indicative of poor myofilament Ca2+ responsiveness, and that the low sarcoplasmic reticulum Ca2+ load resulted from defective SERCA function. In addition, the Lep/Lep mice displayed interrupted leptin signalling and reduced leptin receptor LEPR [41], representing a unique model of obesity. Most obese or overweight individuals display enhanced rather than reduced plasma levels of leptin, contrary to the leptin-deficient status in Lep/Lep obesity [4]. In a recent study, Belke and colleagues found decreased rates of contraction, relaxation and pressure development in hyperleptinaemic Lepr/Lepr diabetic mouse hearts [44]. While cardiac mechanical findings and the slowed intracellular Ca2+ decay in Lepr/Lepr mice are consistent with our present observation in Lep/Lep mice, Lepr/Lepr diabetic myocytes displayed significantly reduced resting and peak Ca2+ levels [44], contrary to our finding in Lep/Lep myocytes. Decreased, increased and unchanged resting intracellular Ca2+ levels have been seen in diabetes, insulin resistance and obesity [2, 45]. The resting intracellular Ca2+ levels appear to be model- and age-dependent.
Increased oxidative stress plays an important role in obesity-related cardiac complications [4, 14], in which NADPH oxidase may serve as the predominant source of ROS [14]. Our results showed that the cardiac GSH/GSSG ratio was decreased in the Lep/Lep group, associated with elevated lipid peroxidation and protein carbonyl content. More importantly, p47phox and gp91phox were significantly elevated in membrane fractions of Lep/Lep mouse myocytes. Activation of NADPH oxidase and subsequent accumulation of ROS are key to oxidative injury in cardiovascular diseases [32, 33, 46]. Oxidative stress has been shown to result in oxidative damage to functional proteins [35]. SERCA2a has been shown to be a vulnerable target for oxidative insult [27, 36]. In this study we demonstrated a marked oxidative modification of SERCA2a in Lep/Lep mouse myocytes, which may contribute to reduced SERCA activity and subsequent cardiac contractile dysfunction in Lep/Lep mouse myocytes. Excessive and irreversible SERCA oxidation may account for heart dysfunction in heart failure, atherosclerosis, ageing and other cardiovascular diseases [27]. Our observation that apocynin abolished angiotensin II and Lep/Lep obesity-induced cardiac mechanical defects and NADPH oxidase subunit membrane distribution (with the exception of p47phox in Lep/Lep myocytes) further consolidated the important role of NAPDH oxidase in cardiac contractile dysfunction in Lep/Lep obesity. Although the discrepancy between apocynin-elicited effects on p47phox and pg91phox is not fully clear at this point, routes of NADPH oxidase activation and the inhibition of this by apocynin may contribute to the disparity in NADPH oxidase subunit response in Lep/Lep myocytes. First, apocynin interrupts the activation of NADPH oxidase through inhibition of the NADPH subunit assembly, its post-translational modification and translocation to the membrane (especially the cytosolic subunit p47phox) [32, 47]. It is possible that apocynin exerts a predominant inhibitory effect on protein assembly of the cytosolic subunit p47phox and the membrane-bound gp91phox, whereas it has little effect on p47phox translocation to the membrane in Lep/Lep myocytes. As a result, apocynin failed to significantly suppress the increase in the membrane distribution of p47phox in Lep/Lep myocytes seen in our present study. Secondly, an association between gp91phox and p47phox was deemed an essential step for NADPH oxidase activation [33]. Therefore, inhibition of apocynin on membrane-bound gp91phox (but not p47phox) in Lep/Lep myocytes may be sufficient to disrupt the association between these two subunits and the subsequent activation of NADPH oxidase in Lep/Lep myocytes. It is also possible that the enhanced membrane distribution of p47phox due to prolonged obesity may not be readily reversed by short-term apocynin treatment. In addition, activation of NADPH oxidase is known to stimulate protein synthesis and cardiac hypertrophy [32], although our 4 h incubation of angiotensin II was too short for the enlargement of cardiomyocytes.
Perhaps the most puzzling result of our study is that apocynin fails to restore the Lep/Lep obesity-induced oxidative modification of SERCA2a and reduced SERCA activity. This observation tends to indicate that the SERCA pump may not be a permissive player downstream of NADPH oxidase activation en route to cardiac mechanical defects in Lep/Lep obesity. However, it may be argued that enhanced oxidative modification of SERCA and impaired SERCA function as a result of the 9-week insulin resistance and mild hyperglycaemia in Lep/Lep obesity cannot be readily reversed by our short-term in vitro apocynin treatment. Nonetheless, a contribution from other SERCA-independent machineries cannot be ruled out at this time. For example, apocynin may counteract certain signalling pathways downstream of angiotensin II. This is supported by our finding that apocynin abolished angiotensin II-elicited mechanical defects and SERCA oxidative modification and reduced 45Ca2+ uptake in lean control myocytes, all of which are reminiscent of the effects seen in Lep/Lep myocytes. Last but not least, it is plausible to speculate that insulin resistance and oxidative stress in Lep/Lep mice may both contribute to cardiac dysfunction. It is likely that ROS precedes Ca2+ overload since the former is known to induce Ca2+ overload in cardiomyocytes [48].
An altered distribution of MHC isoforms has been shown in myocardial remodelling, cardiac hypertrophy and cardiomyopathy [17, 28–31], indicating that the regulation of cardiac contractile function is directly related to the relative amounts of MHC-α and MHC-β isozymes [25]. Even a small shift in the relative expression of these isoforms may significantly alter cardiomyocyte power output [30, 31]. Although the predominant MHC isoform in healthy human hearts is β rather than α, overexpression of MHC-β in transgenic mice suggests that such an MHC-α to MHC-β switch is a maladaptive response to preserve energy [30]. The MHC isozyme switch from the fast type α isoform to the slow type β isoform (lower ratio of MHC-α to MHC-β) is believed to play a significant role in cardiac dysfunction in diabetes, cardiac hypertrophy and senescence [28, 29, 49, 50]. This is supported by the fact that an increase in MHC-α and a decrease in MHC-β mRNA expression (increased ratio of MHC-α to MHC-β) is deemed beneficial in the improvement of left ventricular function in patients with idiopathic dilated cardiomyopathy [31]. Similarly, our results reveal a significant isozyme switch from MHC-α to MHC-β in Lep/Lep mice, which may contribute to contractile dysfunction. This is supported by our observation of impaired SERCA function in Lep/Lep cardiomyocytes. So far, little information is available regarding the ratio between MHC-α and MHC-β in human obesity. To the best of our knowledge, this is the first report to correlate cardiac contractile dysfunction with cardiac MHC isozyme switch in a Lep/Lep model of obesity. However, it should be mentioned that factors such as cardiac hypertrophy, which exists in the Lep/Lep mouse model of obesity, may independently trigger the MHC isozyme switch.
In summary, our findings revealed reduced cardiac contractile capacity, a prolonged duration of relaxation, an elevated resting intracellular Ca2+ level, reduced intracellular Ca2+ extrusion, diminished stress tolerance and depressed Ca2+ responsiveness in Lep/Lep obese mouse myocytes. Our data showing that the NADPH oxidase inhibitor apocynin rescues cardiac contractile dysfunction in Lep/Lep myocytes suggest a causal relationship between oxidative stress and cardiac mechanical dysfunction. Moreover, our data demonstrated increased oxidative modification of SERCA2a, reduced SERCA activity and overt MHC isozyme switch in Lep/Lep mouse myocytes, indicating that both decreased SERCA function and the MHC isozyme switch may participate in cardiac mechanical dysfunction in the Lep/Lep model of obesity. Our short-term in vitro treatment of apocynin failed to reverse SERCA2a oxidative modification and the SERCA defect in Lep/Lep myocytes, making long-term apocynin treatment necessary if we are to understand the roles of NADPH oxidase and SERCA in cardiac contractile dysfunction in Lep/Lep obesity. To validate the role of NADPH oxidase activation in the increased oxidative modification of SERCA2a and reduced SERCA activity in obesity, in vivo treatment with an NADPH oxidase inhibitor using Lep/Lep mice or another genetic or diet-induced model of obesity is needed for future studies. Given what we know about obesity-associated ventricular dysfunction obesity and the high prevalence of juvenile obesity, the use of antioxidants to antagonise obesity-associated cardiac dysfunction should have a promising future.
Abbreviations
- ±dL/dt:
-
maximal velocity of shortening/relengthening
- GSH:
-
glutathione
- GSSG:
-
glutathione disulfide
- MHC:
-
myosin heavy chain
- PS:
-
peak shortening
- ROS:
-
reactive oxygen species
- SERCA:
-
sarco(endo)plasmic reticulum Ca2+-ATPase
- SERCA2a:
-
sarco(endo)plasmic reticulum Ca2+-ATPase isozyme 2a
- TPS50 :
-
time to 50% peak shortening
- TPS50 :
-
time to 90% peak shortening
- TR50 :
-
time to 50% relengthening
- TR90 :
-
time to 90% relengthening
- τ:
-
intracellular Ca2+ decay rate
References
Eckel RH, Barouch WW, Ershow AG (2002) Report of the National Heart, Lung, and Blood Institute-National Institute of Diabetes and Digestive and Kidney Diseases Working Group on the pathophysiology of obesity-associated cardiovascular disease. Circulation 105:2923–2928
Ren J, Sowers JR, Walsh MF, Brown RA (2000) Reduced contractile response to insulin and IGF-I in ventricular myocytes from genetically obese Zucker rats. Am J Physiol Heart Circ Physiol 279:H1708–1714
Montague CT, Farooqi IS, Whitehead JP, et al (1997) Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature 387:903–908
Ren J (2004) Leptin and hyperleptinemia—from friend to foe for cardiovascular function. J Endocrinol 181:1–10
Barouch LA, Cappola TP, Harrison RW, et al (2003) Combined loss of neuronal and endothelial nitric oxide synthase causes premature mortality and age-related hypertrophic cardiac remodeling in mice. J Mol Cell Cardiol 35:637–644
Nickola MW, Wold LE, Colligan PB, Wang GJ, Samson WK, Ren J (2000) Leptin attenuates cardiac contraction in rat ventricular myocytes. Role of NO. Hypertension 36:501–505
Wold LE, Relling DP, Duan J, Norby FL, Ren J (2002) Abrogated leptin-induced cardiac contractile response in ventricular myocytes under spontaneous hypertension: role of Jak/STAT pathway. Hypertension 39:69–74
Xu FP, Chen MS, Wang YZ, et al (2004) Leptin induces hypertrophy via endothelin-1-reactive oxygen species pathway in cultured neonatal rat cardiomyocytes. Circulation 110:1269–1275
Minhas KM, Khan SA, Raju SVY, et al (2005) Leptin repletion restores depressed {beta}-adrenergic contractility in ob/ob mice independently of cardiac hypertrophy. J Physiol 565:463–474
Ren J (2005) Lessons from the leptin paradox in cardiac regulation—too much versus too little. J Physiol 565:347
Correia ML, Haynes WG (2004) Leptin, obesity and cardiovascular disease. Curr Opin Nephrol Hypertens 13:215–223
Uzun H, Zengin K, Taskin M, Aydin S, Simsek G, Dariyerli N (2004) Changes in leptin, plasminogen activator factor and oxidative stress in morbidly obese patients following open and laparoscopic Swedish adjustable gastric banding. Obes Surg 14:659–665
McClung JP, Roneker CA, Mu W, et al (2004) Development of insulin resistance and obesity in mice overexpressing cellular glutathione peroxidase. Proc Natl Acad Sci USA 101:8852–8857
Furukawa S, Fujita T, Shimabukuro M, et al (2004) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114:1752–1761
Katakam PV, Tulbert CD, Snipes JA, Erdos B, Miller AW, Busija DW (2005) Impaired insulin-induced vasodilation in small coronary arteries of Zucker obese rats is mediated by reactive oxygen species. Am J Physiol Heart Circ Physiol 288:H854–860
Boudina S, Sena S, O’Neill BT, Tathireddy P, Young ME, Abel ED (2005) Reduced mitochondrial oxidative capacity and increased mitochondrial uncoupling impair myocardial energetics in obesity. Circulation 112:2686–2695
Razeghi P, Young ME, Cockrill TC, Frazier OH, Taegtmeyer H (2002) Downregulation of myocardial myocyte enhancer factor 2C and myocyte enhancer factor 2C-regulated gene expression in diabetic patients with nonischemic heart failure. Circulation 106:407–411
Russell LK, Finck BN, Kelly DP (2005) Mouse models of mitochondrial dysfunction and heart failure. J Mol Cell Cardiol 38:81–91
Tankersley CG, O’Donnell C, Daood MJ, et al (1998) Leptin attenuates respiratory complications associated with the obese phenotype. J Appl Physiol 85:2261–2269
O’Donnell CP, Tankersley CG, Polotsky VP, Schwartz AR, Smith PL (2000) Leptin, obesity, and respiratory function. Respir Physiol 119:63–70
Yang X, Palanichamy K, Ontko AC, et al (2005) Newly synthetic chromium complex—chromium (phenylalanine)3 improves insulin responsiveness and reduces whole body glucose tolerance. FEBS Lett 579:1458–1464
Li SY, Du M, Dolence EK, et al (2005) Aging induces cardiac diastolic dysfunction, oxidative stress, accumulation of advanced glycation endproducts and protein modification. Aging Cell 4:57–64
Husain K (2004) Physical conditioning modulates rat cardiac vascular endothelial growth factor gene expression in nitric oxide-deficient hypertension. Biochem Biophys Res Commun 320:1169–1174
Blough ER, Rennie ER, Zhang F, Reiser PJ (1996) Enhanced electrophoretic separation and resolution of myosin heavy chain in mammalian and avian skeletal muscles. Anal Biochem 233:31–35
Reiser PJ, Kline WO (1998) Electrophoretic separation and quantitation of cardiac myosin heavy chain isoforms in eight mammalian species. Am J Physiol Heart Circ Physiol 274:H1048–H1053
Yan LJ, Orr WC, Sohal RS (1998) Identification of oxidized proteins based on sodium dodecyl sulfate-polyacrylamide gel electrophoresis, immunochemical detection, isoelectric focusing, and microsequencing. Anal Biochem 263:67–71
Adachi T, Weisbrod RM, Pimentel DR, et al (2004) S-Glutathiolation by peroxynitrite activates SERCA during arterial relaxation by nitric oxide. Nat Med 10:1200–1207
Rundell VL, Manaves V, Martin AF, de Tombe PP (2005) Impact of beta-myosin heavy chain isoform expression on cross-bridge cycling kinetics. Am J Physiol Heart Circ Physiol 287:H408–H413
Olsson MC, Palmer BM, Stauffer BL, Leinwand LA, Moore RL (2004) Morphological and functional alterations in ventricular myocytes from male transgenic mice with hypertrophic cardiomyopathy. Circ Res 94:201–207
Krenz M, Robbins J (2004) Impact of beta-myosin heavy chain expression on cardiac function during stress. J Am Coll Cardiol 44:2390–2397
Lowes BD, Gilbert EM, Abraham WT, et al (2002) Myocardial gene expression in dilated cardiomyopathy treated with beta-blocking agents. N Engl J Med 346:1357–1365
Cai H, Griendling KK, Harrison DG (2003) The vascular NAD(P)H oxidases as therapeutic targets in cardiovascular diseases. Trends Pharmacol Sci 24:471–478
Touyz RM, Chen X, Tabet F, et al (2002) Expression of a functionally active gp91phox-containing neutrophil-type NAD(P)H oxidase in smooth muscle cells from human resistance arteries: regulation by angiotensin II. Circ Res 90:1205–1213
Privratsky JR, Wold LE, Sowers JR, Quinn MT, Ren J (2003) AT1 blockade prevents glucose-induced cardiac dysfunction in ventricular myocytes: role of the AT1 receptor and NADPH oxidase. Hypertension 42:206–212
Dalle-Donne I, Scaloni A, Giustarini D, et al (2005) Proteins as biomarkers of oxidative/nitrosative stress in diseases: the contribution of redox proteomics. Mass Spectrom Rev 24:55–99
Squier TC (2001) Oxidative stress and protein aggregation during biological aging. Exp Gerontol 36:1539–1550
Pantke U, Volk T, Schmutzler M, Kox WJ, Sitte N, Grune T (1999) Oxidized proteins as a marker of oxidative stress during coronary heart surgery. Free Radic Biol Med 27:1080–1086
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM (1994) Positional cloning of the mouse obese gene and its human homologue. Nature 372:425–432
Schwartz MW, Porte D Jr (2005) Diabetes, obesity, and the brain. Science 307:375–379
Mazumder PK, O’Neill BT, Roberts MW, et al (2004) Impaired cardiac efficiency and increased fatty acid oxidation in insulin-resistant ob/ob mouse hearts. Diabetes 53:2366–2374
Dong F, Zhang X, Yang X, et al (2006) Impaired cardiac contractile function in ventricular myocytes from leptin deficient ob/ob obese mice. J Endocrinol 188:25–36
Sabbah HN (2004) Effects of cardiac support device on reverse remodeling: molecular, biochemical, and structural mechanisms. J Card Fail 10:S207–S214
Kass DA, Bronzwaer JG, Paulus WJ (2004) What mechanisms underlie diastolic dysfunction in heart failure? Circ Res 94:1533–1542
Belke DD, Swanson EA, Dillmann WH (2004) Decreased sarcoplasmic reticulum activity and contractility in diabetic db/db mouse heart. Diabetes 53:3201–3208
Pierce GN, Russell JC (1997) Regulation of intracellular Ca2+ in the heart during diabetes. Cardiovasc Res 34:41–47
Li JM, Shah AM (2002) Intracellular localization and preassembly of the NADPH oxidase complex in cultured endothelial cells. J Biol Chem 277:19952–19960
Stolk J, Hiltermann TJ, Dijkman JH, Verhoeven AJ (1994) Characteristics of the inhibition of NADPH oxidase activation in neutrophils by apocynin, a methoxy-substituted catechol. Am J Respir Cell Mol Biol 11:95–102
Goldhaber JI, Qayyum MS (2000) Oxygen free radicals and excitation-contraction coupling. Antioxid Redox Signal 2:55–64
Zhong Y, Reiser PJ, Matlib MA (2003) Gender differences in myosin heavy chain-beta and phosphorylated phospholamban in diabetic rat hearts. Am J Physiol Heart Circ Physiol 285:H2688–H2693
Carnes CA, Geisbuhler TP, Reiser PJ (2004) Age-dependent changes in contraction and regional myocardial myosin heavy chain isoform expression in rats. J Appl Physiol 97:446–453
Acknowledgements
We are grateful to P. J. Reiser from Ohio State University for his helpful advice on electrophoretic separation of α- and β-MHC. We would like to thank M. T. Quinn from Montana State University for providing antibodies for NADPH oxidase subunits gp91phox and p47phox. The authors also wish to acknowledge M. Trucillo and R. Cohen from Boston University for guidance on SERCA activity assay. Technical assistance from T. A. Doser, J. M. Nunn, S. A. Babcock, P. Xu and B. H. Ren was also greatly appreciated. This work was supported in part by grants from the American Diabetes Association (7-00-RA-21), American Heart Association Pacific Mountain Affiliate (no. 0355521Z) and NIH/NIA 1 R03 AG21324-01 to J. Ren.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, SY., Yang, X., Ceylan-Isik, A.F. et al. Cardiac contractile dysfunction in Lep/Lep obesity is accompanied by NADPH oxidase activation, oxidative modification of sarco(endo)plasmic reticulum Ca2+-ATPase and myosin heavy chain isozyme switch. Diabetologia 49, 1434–1446 (2006). https://doi.org/10.1007/s00125-006-0229-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0229-0