Abstract
Aims/hypothesis
Prenatal glucocorticoid exposure causes lifelong hyperglycaemia in rat offspring, associated with permanently increased hepatic phosphoenolpyruvate carboxykinase 2 (PCK2), the rate-controlling enzyme of gluconeogenesis. To elucidate the mechanisms underlying the ‘programming’ of PCK2, this study examined the effect of prenatal dexamethasone treatment on expression of transcription factors that regulate Pck2.
Materials and Methods
Real-time RT-PCR and in situ hybridisation were used to measure and localise hepatic mRNA transcribed from the genes for PCK2, hepatocyte nuclear factor 4, alpha (HNF4A), transcription factor 1 (TCF1), CCAAT/enhancer binding protein, alpha (CEBPA), CEBPB, the glucocorticoid receptor (NR3C1) and peroxisome proliferative activated receptor, gamma, coactivator 1 alpha (PPARGC1A) in foetal and adult offspring of dams treated with dexamethasone or vehicle during the last week of gestation.
Results
Prenatal dexamethasone exposure significantly elevated Hnf4a mRNA expression in foetal and adult liver. This resulted from increased expression of isoforms derived from the ‘adult’ (P1) Hnf4a promoter. In contrast, isoforms from the ‘foetal’ (P2) promoter were markedly suppressed by dexamethasone. Like Pck2, the increase in hepatic Hnf4a mRNA occurred exclusively in the periportal zone. Foetal Tcf1 expression was also increased by dexamethasone treatment, but this did not persist into adulthood. Prenatal dexamethasone did not affect the amounts of foetal and/or adult Cebpa, Cebpb, Nr3c1 or Ppargc1a mRNA.
Conclusions/interpretation
Prenatal dexamethasone exposure caused a permanent increase in hepatic Hnf4a mRNA. This increase, which was associated with a premature switch from foetal to adult promoter predominance, was congruent with changes in Pck2 expression. These data suggest that HNF4A might mediate Pck2 overexpression and subsequent hyperglycaemia.
Similar content being viewed by others
Introduction
Compelling epidemiological evidence suggests that early-life events play an important role in determining the risk for common cardiovascular and metabolic disorders in adulthood. In particular, low birthweight is associated with a substantially greater incidence of adult hypertension, insulin resistance/type 2 diabetes mellitus and cardiovascular disease deaths [1, 2]. These observations have led to the concept of early-life ‘programming’, involving the action of a factor during a sensitive ‘window’ of development that alters the maturation, structure and function of specific tissues, producing effects that persist throughout life [2]. The mechanisms that might link low birthweight and adult disease remain unknown but are of clear importance.
We and others have previously shown that treating pregnant rats with glucocorticoids selectively during the last week of gestation reduces birthweight and causes permanent hyperglycaemia and hypertension in the adult offspring [3–5], suggesting that glucocorticoids might underlie the association between low birthweight and later disease. Indeed, inhibition of foeto-placental 11β-hydroxysteroid dehydrogenase type 2, the physiological barrier enzyme which protects the foetus from maternal glucocorticoids, has similar long-term programming effects [6]. Mechanistically, the hyperglycaemia was associated with permanent elevation of hepatic Pck2 expression. Phosphoenolpyruvate carboxykinase 2 (PCK2) is the rate-controlling enzyme of gluconeogenesis, the key process under fasting conditions that determines blood glucose levels and which is increased in patients with type 2 diabetes mellitus [7]. Indeed, hepatic Pck2 overexpression in transgenic mice produces fasting hyperglycaemia and glucose intolerance [8]. Increased liver PCK2 activity may therefore be of functional significance in the pathogenesis of hyperglycaemia in our rat model of prenatal exposure to glucocorticoids [3]. The molecular details of how transient exposure to glucocorticoids for a few days before birth might permanently alter the ‘set-point’ of hepatic Pck2 expression across the lifespan are not known. PCK2 first appears just before birth in preparation for extrauterine life and is the last gluconeogenic pathway enzyme to develop [9]. The induction of Pck2 at birth and its expression in mature hepatocytes is regulated by distinct hepatocyte-enriched nuclear transcription activators and associated co-activators that bind their cognate DNA motifs in the Pck2 promoter [10]. These transcription factors include members of the hepatocyte nuclear factor family (such as transcription factor 1 [TCF1] and hepatocyte nuclear factor 4, alpha [HNF4A]), members of the CCAAT/enhancer binding protein (C/EBP) family and the glucocorticoid receptor (NR3C1), as well as the key energy-regulating co-activator protein, peroxisome proliferative activated receptor, gamma, coactivator 1 alpha (PPARGC1A). Liver-enriched transcription factors are also expressed in, and regulate the function of a number of other metabolically active tissues including the pancreatic islets and adipose tissue. Increasing data in humans show that aberrant expression of the liver-enriched transcription factors results in metabolic disturbance. For example, mutations in the genes encoding TCF1 or HNF4A cause MODY, a subgroup of diabetes characterised by an autosomal dominant inheritance and early-onset non-insulin-dependent diabetes resulting from pancreatic beta-cell dysfunction [11, 12]. HNF4A is also suspected of playing a role in the pathogenesis of type 2 diabetes, so that inheriting particular HNF4A variants may alter insulin secretion and predispose to hyperglycaemia [13–15]. Patients with MODY may also have primary metabolic defects in the liver [16].
The mechanisms that regulate the expression of liver-enriched transcription factors during development are not fully understood, but hormonal signals are thought to be important. For example, perinatal maturation of the liver (including the appearance of PCK2 at birth) coincides with a period of profound change in nutrient and hormonal status, including a rise in circulating glucocorticoids and catecholamines, and a fall in insulin levels [17]. Indeed, glucocorticoids and glucagon (acting via cAMP) are crucial for optimal differentiation of foetal hepatocytes in vitro, and administration of glucagon (or cAMP), glucocorticoids or streptozotocin, to reduce insulin levels, induces precocious appearance of hepatic PCK2 [17–20]. Alterations in the prenatal hormonal milieu might therefore influence the development of liver-enriched transcription factors, which in turn may affect maturation of the target organs. In order to begin to elucidate the fundamental molecular mechanisms that are involved in glucocorticoid programming of hepatic Pck2 expression, we have examined the effects of prenatal exposure to dexamethasone on hepatic expression of key liver-enriched transcription factors, both immediately with glucocorticoid exposure in the foetus and subsequently in adult offspring.
Research design and methods
Animals
All experiments were carried out under an appropriate UK Home Office licence. Female Wistar rats (200–250 g; Harlan UK, Bicester, UK) were maintained under conditions of controlled lighting (lights on 07.00–19.00 h) and temperature (22°C) and allowed free access to food (standard rat chow; 56.3% carbohydrate, 18.3% protein, NaCl 0.7%; BS & S Scotland, Edinburgh, UK) and tap water. Time-mated rats (five per group) were given either s.c. dexamethasone (100 μg kg−1 day−1, dissolved in 4% ethanol–0.9% saline, 200 μg/ml) or vehicle during the last week (day 15 to day 21) of pregnancy. At birth, the offspring were weighed and culled to six per litter. The pups were weaned at postnatal day 21. Adult (6-month-old) male offspring were killed by decapitation in a fed state and livers were removed and quickly frozen in liquid nitrogen and stored at −70°C for subsequent analyses. In a separate cohort of animals, livers from treatment and control groups were collected from foetuses at embryonic day (E)15, E19, E21 and postnatal day 7 neonates. Each group consisted of four dams, and livers from four foetuses or neonates, selected at random, were used per dam. Real-time RT-PCR was used to determine hepatic mRNA transcribed from the genes for PCK2, CEBPA, CEBPB, TCF1, HNF4A, NR3C1 and PPARGC1A. In situ hybridisation was used to localisation and quantify mRNA expression within the hepatic acinus.
In situ mRNA hybridisation
All restriction enzymes and RNA polymerases were obtained from Promega UK (Southampton, UK). Cebpa and Cebpb cDNAs were kind gifts from W. C. Yeh (University of Toronto, Toronto, ON, Canada) and S. L. McKnight (University of Texas Southwestern Medical Center, Dallas, TX, USA). Cebpa probes were made from a 300 bp fragment derived from the coding region of rat Cebpa cDNA subcloned into the pGEM3 vector. Antisense RNA probe was generated by T7 RNA polymerase following HindIII linearisation of vector and non-complementary sense strand was transcribed by SP6 RNA polymerase from EcoRI-linearised vector. Cebpb templates were made from a 390 bp NcoI fragment of Cebpb subcloned into pGEM3, and sense and antisense strands transcribed as above. Hnf4a templates were generated from a 1.2 kb PvuII fragment of rat Hnf4a cDNA cloned into Bluescript KS (gift from G. Kelsey, The Babraham Institute, Cambridge, UK). T7 RNA polymerase was used to make the antisense transcript (from EcoRI-linearised vector), while antisense template was made by T3 polymerisation from SacII-linearised vector. Tcf1 cDNA was a gift from M. Yaniv (Institut Pasteur, Paris, France). A 627 bp NcoI fragment of Tcf1 was subcloned into pGEM 5Z. The sense strand was transcribed by SP6 RNA polymerase from SphI-linearised vector while the antisense strand was obtained with T7 RNA polymerase following SacI linearisation. Radioactive probes were synthesised by incubating the appropriate RNA polymerase (15 U) with 0.5 μg linearised plasmid, 1×transcription buffer (Promega), 10 mmol/l dithiothreitol, 3 mmol/l ATP/GTP/CTP, 7.4 MBq [α-35S]UTP (Amersham International) and 4 U RNase inhibitor in a total volume of 10 μl for 1 h at 37°C (or 40°C for SP6 RNA polymerase). DNase I (0.1 U) was added to the mixture and incubated for a further 10 min. The probe was purified by passage through a Sephadex G-50 column (Pharmacia Biotech, St Albans, UK). In situ hybridisation was performed as described previously [21]. In brief, cryostat sections (10 μm) from frozen liver were mounted on poly-l-lysine-coated slides and fixed for 10 min in 4% paraformaldehyde solution in 0.1 mol/l phosphate buffer, pH 7.4 and washed three times in 2×SSC. Antisense or sense probes were diluted in hybridisation buffer to 5×106 cpm/μl. The hybridisation mixture contained 0.5 mol/l NaCl, 0.01 mol/l Tris–HCl (pH 7.5), 1 mmol/l EDTA, 10 mmol/l dithiothreitol, 10% dextran sulphate, 1×Denhardt’s solution, 2 μg/ml herring testis DNA, 0.125 mg/ml yeast tRNA and 50% (v/v) deionised formamide. Hybridisation was carried out overnight at 55°C in a chamber humidified with 50% deionised formamide/4×SSC. Following three washes at room temperature in 2×SSC, sections were treated with 30 μg/ml bovine pancreatic RNase A (Boehringer Mannheim UK, Lewes, UK) in buffer containing 0.5 mol/l NaCl, 0.01 mol/l Tris–HCl, pH 7.5 and 1 mmol/l EDTA, and incubated for 1 h at 37°C. Sections were then washed in 2×SSC at room temperature for 30 min and twice in 0.1×SSC at 60°C for 30 min. After dehydration in graded ethanol the slides were dipped in Kodak NTB 2 emulsion diluted 1:1 with distilled water. Autoradiography was performed at 4°C for 4 weeks. After development, sections were counterstained with haematoxylin and eosin. The hybridisation signal was quantified by counting silver grains in the periportal and perivenous regions (six sections per animal) under bright-field illumination using a computer-driven image analysis system (Seescan, Cambridge, UK). Specificity of hybridisation was demonstrated using labelled sense RNA probes hybridised under identical conditions.
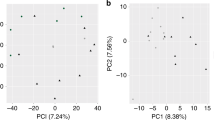
Real-time RT-PCR total RNA was extracted from liver using TRIzol as per manufacturer’s instructions (Gibco PRL, Paisley, UK), and quantified spectrophotometrically at OD260. RNA integrity was checked by agarose gel electrophoresis. Oligodeoxythymidine-primed cDNA was synthesised from 1 μg RNA samples using the First-Strand cDNA synthesis kit (Amersham Pharmacia Biotech, Bucks, UK). Quantification of Pck2, Nr3c1, Cebpa, Ppargc1a, Tcf1 and Hnf4a mRNA was performed with real-time PCR primer-probe sets using the ABI PRISM 7700 Sequence Detection System (PE Applied Biosystems, Cheshire, UK). We used TaqMan Gene Expression Assay (Applied Biosystems) primers for Cepba (Assay ID Rn00560963_s1), Nr3c1 (Assay ID Rn00561369_m1) and Ppargc1a (Assay ID Rn00580241_m1). Custom TaqMan Gene Expression Assay primers were used for Pck2 and Tcf1: Pck2, 5′-TGTCATCCGCAAGCTGAAGAA-3′ (forward), 5′-GCTTTCGATCCTGGCCACAT-3′ (reverse), and 5′-6-FAM-CCAGCCAACAGTTGTC-TAMRA-3′ (probe); Tcf1 5′-GAAGAGCGAGAGACCTTGGT-3′ (forward), 5′-GGTGACACCCCTCTCTGGAT-3′ (reverse), and 5′-6-FAM-CACTCCGCCCTATTGC-TAMRA-3′ (probe). Hnf4a potentially encodes nine distinct isoforms (Hnf4a1 to Hnf4a9) as a result of alternative promoter usage and differential splicing [22–25], and these isoforms are expressed in a tissue-specific manner. Embryonic/foetal liver predominantly expresses ‘foetal’ P2-promoter-initiated isoforms (Hnf4a7 and Hnf4a8), while Hnf4a1 and Hnf4a2 (driven by ‘adult’ P1 promoter) are first expressed later in gestation and predominate in the adult liver (Fig. 1a). Primers for detection of total Hnf4a mRNA were purchased from PE Applied Biosystems (TaqMan Gene Expression Assay, ID Rn00573309_m1). The forward primer for detection of Hnf4a1/2 mRNA was 5′-GACATGGACATGGCTGACTACG and that for Hnf4a7/8 was 5′-GTCATGCTCAGTGTGAACG. 5′-CAGAAGGGAGGCTTGACGA was used as reverse primer for both sets of transcripts (Fig. 1b). Cyclophilin (PE Applied Biosystems) primers/probes-5′-CCCACCGTGTTCTTCGACAT-3′ (forward), 5′-GAAAGTTTTCTGCTGTCTTTGGAACT-3′, (reverse) and 5′-FAM-6-CAAGGGCTCGCCATCAGCCGT-TAMRA-3′ (probe)-were used to normalise the mRNA levels of the gene of interest. A standard curve for each primer–probe set was generated by serial dilution of cDNA from all samples done in triplicate. Each sample was run in duplicate and the mean values of the duplicates were used to calculate transcript level.
Expression of Hnf4a in the liver. a Systematic representation of Hnf4a. Exons are shown as boxes. The arrows represent the two alternative promoters and the lines linking exons indicate splicing events. Splicing of exon 1A to exon 2 yields isoform a1, whereas splicing of 1D to exon 2 yields isoform a7. Use of a second donor site at the 3′ end of exon 9 (clear area) yields a 30-bp insert in isoforms a2 and a8. b Representation of Hnf4a isoforms a1/a2 and a7/a8. Positions of primers used in PCR are indicated. Primers ‘a’ and ‘b’ were used to detect Hnf4a transcripts containing exon 1A, whereas transcripts initiated at exon 1D were detected using primers ‘d’ and ‘b’
Statistics
All data are expressed as means±SEM. Data were compared using unpaired Student’s t tests or one-way ANOVA followed by Newman–Keuls post-hoc multiple comparisons test, where appropriate. Values were considered significant at p<0.05.
Results
Pck2 expression
Hepatic Pck2 mRNA increased towards term, so that there was a sevenfold rise between E15 and E21 in control foetuses (Fig. 2a). Foetuses that were exposed to dexamethasone had significantly higher hepatic Pck2 mRNA levels at E19 and E21 compared with controls (Fig. 2a). As we have shown previously [3], the elevation in Pck2 mRNA persisted in the adult liver (Fig. 2b), and this increase was located predominantly in the periportal zone (Fig. 3).
Effect of prenatal dexamethasone on hepatic Pck2 expression. Hepatic Pck2 mRNA was measured in foetuses (a) or in adult offspring (b) of dams that received vehicle (open bars) or dexamethasone (closed bars) during the last week of gestation. In foetuses (a), percentage mRNA is shown relative to that in E15 control livers. In adult livers (b), results are expressed as percentage mRNA in adult control animals. E embryonic age. Means±SEM of n=6–10 per group. *p<0.05 vs control
Hnf4a expression
Hepatic total Hnf4a mRNA level increased progressively between E15 and E21 (Fig. 4a). Foetuses of dams that received dexamethasone had significantly higher amounts of total Hnf4a mRNA at E19 and E21, but not earlier in gestation (E15), compared with controls (Fig. 4a). Like Pck2, Hnf4a expression was more prominent in the periportal region than the perivenous zone (Fig. 3). The adult offspring of dams given dexamethasone during pregnancy had significantly elevated levels of total Hnf4a mRNA, selectively in the periportal zone, compared with controls (Fig. 4b). Hnf4a expression within the perivenous region of the hepatic acinus was not significantly different between dexamethasone-exposed animals and controls (data not shown). There was a strong correlation (r=0.75, p=0.02) between hepatic total Hnf4a and Pck2 mRNA. Prenatal dexamethasone treatment caused marked suppression of Hnf4a transcripts that are initiated at the P2 promoter (Hnf4a7/8) (Fig. 4c), suggesting that the increase in total Hnf4a mRNA resulted from increased activity of the P1 promoter. When Hnf4a7/8 and Hnf4a1/2 mRNA levels were compared in E21 and postnatal day 7 livers, the ratio of Hnf4a7/8 to Hnf4a1/2 mRNA was 1:4 in controls, whilst in the prenatal dexamethasone-exposed group it was 1:9.
Effect of prenatal dexamethasone on hepatic Hnf4a expression. Hepatic total Hnf4a mRNA was measured in foetuses (a) or in adult offspring (b) of dams that received vehicle (open bars) or dexamethasone (closed bars) during the last week of gestation. c Amounts of the P2-promoter-initiated isoforms (Hnf4a7/8). In a and c, percentage mRNA is shown relative to that in E15 control livers. In adult livers (b), results are expressed as percentage mRNA in adult control animals. E embryonic age; P postnatal age in days. Means±SEM of n=6–10 per group. *p<0.05 vs control
Tcf1 expression
Foetal hepatic Tcf1 mRNA increased with gestational age. Livers from dexamethasone-exposed foetuses had higher levels of Tcf1 mRNA at E19 and E21 compared with controls (Fig. 5a). In the adult liver, Tcf1 mRNA did not show zonation in its distribution, with equal levels in periportal and perivenous regions (Fig. 3). In sharp contrast to the effect in the foetal liver (where Tcf1 mRNA was induced and correlated positively with Pck2 mRNA; r=0.59, p=0.04), adult offspring of dams that received dexamethasone prenatally had reduced hepatic Tcf1 mRNA compared with controls (Fig. 5b).
Effect of prenatal dexamethasone on hepatic Tcf1 expression. Hepatic Tcf1 mRNA was measured in foetuses (a) or in adult offspring (b) of dams that received vehicle (open bars) or dexamethasone (closed bars) during the last week of gestation. In foetuses (a), percentage mRNA is shown relative to that in E15 control livers. In adult livers (b), results are expressed as percentage mRNA in adult control animals. E embryonic age. Means±SEM of n=6–12 per group. *p<0.05 compared with control
Expression of Cebp genes
There was an ontogenic rise in hepatic Cebpa mRNA between E15 and E21 (Fig. 6a). Dexamethasone treatment did not alter foetal Cebpa mRNA levels at any time point. In the adult liver, Cebpa was expressed evenly in the periportal and perivenous zones (Fig. 3), consistent with previous data [26], and was unaffected by in utero exposure to dexamethasone (Fig. 6b). Cebpb mRNA was assessed in adult livers only. It also had an even pattern of expression across the hepatic acinus (data not shown), and prenatal dexamethasone treatment had no effect on the level of Cebpb mRNA (Fig. 6c).
Effect of prenatal dexamethasone on hepatic Cebpa and Cebpb expression. Hepatic Cebpa mRNA was measured in foetuses (a) or in adult offspring (b) of dams that received vehicle (open bars) or dexamethasone (closed bars) during the last week of gestation. c Cebpb mRNA expression in the adult livers. In foetuses (a), percentage mRNA is shown relative to that in E15 control livers. In adult livers (b and c), results are expressed as percentage of mRNA in adult control animals. Means±SEM of n=6–10 per group. E embryonic age
Nr3c1 and Ppargc1a expression
Previous data showed that hepatic Nr3c1 mRNA is increased in the adult offspring following prenatal exposure to dexamethasone [3]. In the present study we examined the amount of Nr3c1 mRNA in foetal liver, and we found similar level of mRNA in foetuses of dexamethasone-treated dams and those from dams that received vehicle injections (Fig. 7a). Likewise, dexamethasone treatment did not alter the level of Ppargc1a mRNA in foetal liver (Fig. 7b).
Effect of prenatal dexamethasone on hepatic Nr3c1 and Ppargc1a expression. Hepatic Nr3c1 (a) and Ppargc1a (b) mRNA expression was measured in foetuses of dams that received vehicle (open bars) or dexamethasone (closed bars) during the last week of gestation. Results are expressed as percentage mRNA relative to that in E15 control (vehicle) livers. Means±SEM of n=8 per group. E embryonic age
Discussion
In a previous study we showed that a brief prenatal exposure to supraphysiological levels of glucocorticoids in late gestation causes lifelong hyperglycaemia, associated with a permanent elevation in hepatic Pck2 expression in the rat offspring [3]. Our current data demonstrate that such prenatal glucocorticoid treatment results in significant changes in hepatic expression of key transcriptional factors that regulate Pck2. In particular, dexamethasone exposure induced a prompt rise in foetal hepatic Hnf4a mRNA. The increase in Hnf4a was predominantly in the periportal region of the hepatic acinus and persisted into adulthood, congruent with the change in Pck2 mRNA. Although prenatal dexamethasone treatment was also associated with increased foetal hepatic Tcf1 mRNA, this increase did not persist into adulthood. Several studies have shown cross-regulation between TCF1 and HNF4A and the increase in foetal levels may well reflect this interaction [27–29], but the reasons for the discrepancy in the adult liver are unclear. Nevertheless, TCF1 does not appear to be instrumental in driving adult hepatic Pck2 overexpression in this model. Nr3c1 mRNA level was found to be higher in the adult liver following prenatal glucocorticoid exposure, a change also confined to the periportal zone [3]. Increased hepatic NR3C1 may be important in the phenotype, as prenatal dexamethasone-exposed adult rats are supersensitive to the hyperglycaemic actions of glucocorticoids [3]. However, NR3C1 is part of a macromolecular assembly that regulates the proximal Pck2 promoter in association with other transcription factors such as HNF4A, TCF1 and CEBPs [30]. Moreover, the level of Nr3c1 mRNA was not affected by prenatal dexamethasone in foetal liver, suggesting that the change in Nr3c1 expression is mediated secondarily through a mechanism that develops postnatally. In foetal liver, expression of Ppargc1a, a key transcriptional coactivator that regulates energy homeostasis and interacts with HNF4A and NR3C1 in stimulating Pck2 expression [31, 32], was also unaffected by maternal dexamethasone treatment. This suggests that the change in hepatic Hnf4a and Pck2 mRNA, at least in foetal liver, is unlikely to be due to NR3C1 or PPARGC1A. Likewise, the levels of Cebpa and Cebpb mRNA were not significantly affected by maternal dexamethasone treatment. Therefore, although these genes may be acutely regulated by glucocorticoids [33], they are unlikely to be critical determinants in the long-term programming of Pck2 by glucocorticoids.
Thus, it is the changes in Hnf4a mRNA levels that best correlated with the alterations in Pck2 expression. HNF4A is produced from an early stage in hepatocyte differentiation and plays a key role in regulation of liver development and metabolic function; nearly half of the transcribed genes in the liver, including Pck2, are thought to be controlled by HNF4A [34–36]. Overexpression of Hnf4a in cell culture results in stimulation of Pck2 transcription [37]. Conversely, Hnf4a liver-specific knockout mice fail to induce PCK2 during fasting [35]. Furthermore, maternal vitamin A deficiency reduces Hnf4a mRNA in foetal liver and this is associated with impaired foetal and neonatal development of PCK2 [38]. The increase in hepatic Hnf4a expression following prenatal dexamethasone treatment may therefore represent a primary event that drives Pck2 overexpression and subsequent hyperglycaemia. However, Pck2 is regulated through complex mechanisms that involve other transcription factors, such as chicken ovalbumin upstream transcription factor, peroxisome proliferator activated receptor gamma 2, retinoic acid receptor, retinoid X receptor, and members of the Forkhead family of transcription factors, FOXO1 and Foxa2 [39], which may be important but were not examined in this study.
Hnf4a potentially encodes at least nine distinct isoforms as a result of alternative promoter usage and differential splicing [22–25]. The developmental and physiological relevance of the various Hnf4a isoforms has not been fully explored, mainly because most previous studies relied on probes that failed to differentiate among the isoforms. However, recent data suggest that these isoforms are expressed in a tissue-specific fashion, and that within a particular tissue the pattern of expression may depend on developmental stage. For example, Hnf4a7/8 mRNA is predominant in embryonic/foetal liver, while Hnf4a1/2 isoforms increase dramatically in late gestation and predominate in adult life [23]. In our experimental model, we found an increase in hepatic total Hnf4a mRNA following prenatal dexamethasone treatment. However, the levels of P2-promoter-initiated transcripts (Hnf4a7/8) were significantly lower at all stages in animals exposed to dexamethasone, suggesting that the increased total Hnf4a mRNA is due to a rise in P1-promoter-initiated transcripts, which are likely to be disproportionately elevated (high P1:P2 ratio) in the treated animals. In vitro studies have shown that a change in the Hnf4a profile (from Hnf4a7/8 to Hnf4a1/2 predominance) is associated with differentiation of the hepatoma cells from foetal into adult hepatic phenotype [40]. Taken together, these data suggest that glucocorticoids influence hepatic maturation through differential regulation of the Hnf4a promoters. Whether this effect exists at physiological concentrations of glucocorticoids remains unknown. However, the interaction of glucocorticoids and Hnf4a is further supported by the recent identification in mouse Hnf4a of an enhancer element containing a glucocorticoid response sequence [41]. These data are consistent with a mechanism in which prenatal glucocorticoid exposure alters hepatic Hnf4a isoforms with the ratio of P1-promoter-driven transcripts (Hnf4a1/2) ‘fixed’ at a permanently high level, which would lead to permanent overactivity of the target genes such as Pck2, and contribute to hyperglycaemia. It is noteworthy, however, that liver-enriched transcription factors are part of a complex transcriptional network that is established by a number of autoregulatory and cross-regulatory pathways [26–28], and it remains to be established whether the change in Hnf4a expression is the primary effect of prenatal dexamethasone treatment or is secondary to alterations in the expression and/or function of other genes involved in the glucose metabolism/insulin signalling system. However, given the central role of HNF4A in regulating development and metabolism, its abnormal expression may have widespread pathophysiological consequences.
Abbreviations
- CEBPA:
-
CCAAT/enhancer binding protein, alpha
- CEBPB:
-
CCAAT/enhancer binding protein, beta
- NR3C1:
-
nuclear receptor subfamily 3, group C, member 1 (glucocorticoid receptor)
- HNF4A:
-
hepatocyte nuclear factor 4, alpha
- P1:
-
promoter 1 (adult)
- P2:
-
promoter 2 (foetal)
- PCK2:
-
phosphoenolpyruvate carboxykinase 2
- PPARGC1A:
-
peroxisome proliferative activated receptor, gamma, coactivator 1 alpha
- TCF1:
-
transcription factor 1
References
Barker DJP (1998) In utero programming of chronic disease. Clin Sci 95:115–128
Bateson P, Barker D, Clutton-Brock T et al (2004) Developmental plasticity and human health. Nature 430:419–421
Nyirenda MJ, Lindsay RS, Kenyon CJ, Burchell A, Seckl JR (1998) Glucocorticoid exposure in late gestation permanently programs rat hepatic phosphoenolpyruvate carboxykinase and glucocorticoid receptor expression and causes glucose intolerance in adult offspring. J Clin Invest 101:2174–2181
Nyirenda MJ, Welberg LA, Seckl JR (2001) Programming hyperglycaemia in the rat through prenatal exposure to glucocorticoids—fetal effect or maternal influence? J Endocrinol 170:653–660
Levitt N, Lindsay RS, Holmes MC, Seckl JR (1996) Dexamethasone in the last week of pregnancy attenuates hippocampal glucocorticoid receptor gene expression and elevates blood pressure in the adult offspring in the rat. Neuroendocrinology 64:412–418
Lindsay RS, Lindsay RM, Waddell BJ, Seckl JR (1996) Prenatal glucocorticoid exposure leads to offspring hyperglycaemia in the rat: studies with 11β-hydroxysteroid dehydrogenase inhibitor carbenoxolone. Diabetologia 39:1299–1305
Consoli A, Nurjhan N (1990) Contribution of gluconeogenesis to overall glucose output in diabetic and nondiabetic men. Ann Med 22:191–195
Valera A, Pujol A, Pelegrin M, Bosch F (1994) Transgenic mice overexpressing phosphoenolpyruvate carboxykinase develop non-insulin-dependent diabetes. Proc Natl Acad Sci USA 91:9151–9154
Ballard FJ, Hanson RW (1967) Phosphoenolpyruvate carboxykinase and pyruvate carboxylase in the developing rat liver. Biochem J 104:871–886
Xanthopoulos KG, Mirkovitch J (1993) Gene regulation in rodent hepatocyte during development, differentiation and disease. Eur J Biochem 216:353–360
Yamagata F, Furuta H, Oda N et al (1996) Mutation in hepatic nuclear factor-4a gene in maturity-onset diabetes of the young (MODY 1). Nature 384:458–460
Yamagata K, Oda N, Kaisaki PJ et al (1996) Mutations in the hepatic nuclear factor 1-alpha gene in maturity-onset diabetes of the young (MODY 3). Nature 384:455–458
Zhu Q, Yamagata K, Miura A et al (2003) T130I mutation in HNF-4alpha gene is a loss-of-function mutation in hepatocytes and is associated with late-onset type 2 diabetes mellitus in Japanese subjects. Diabetologia 46:567–573
Silander K, Mohlke KL, Scott LJ et al (2004) Genetic variation near the hepatocyte nuclear factor-4 alpha gene predicts susceptibility to type 2 diabetes. Diabetes 53:1141–1149
Love-Gregory LD, Wasson J, Ma J et al (2004) A common polymorphism in the upstream promoter region of the hepatocyte nuclear factor-4 alpha gene on chromosome 20q is associated with type 2 diabetes and appears to contribute to the evidence for linkage in an Ashkenazi Jewish population. Diabetes 53:1134–1140
Shih DQ, Dansky HM, Fleisher M, Assmann G, Fajans SS, Stoffel M (2000) Genotype/phenotype relationships in HNF-4alpha/MODY1: haploinsufficiency is associated with reduced apolipoprotein (AII), apolipoprotein (CIII), lipoprotein(a), and triglyceride levels. Diabetes 49:832–837
Girard JR, Cuender GS, Marliss EB, Kervran A, Rieutort M, Assan R (1973) Fuels, hormones, and liver metabolism at term and during early postnatal period in the rat. J Clin Invest 52:3190–3200
Chou JY (1988) Regulation of foetal liver differentiation in vitro. Arch Biochem Biophys 263:378–386
Hanson RW, Reshef L, Ballard J (1975) Hormonal regulation of hepatic p-enolpyruvate carboxykinase (GTP) during development. Fed Proc 34:166–171
Philippidis H, Ballard FJ (1970) The development of gluconeogenesis in rat liver. Effects of glucagon and ether. Biochem J 120:385–392
Seckl JR, Dickson KL, Fink G (1990) Central 5,7-dihydroxytryptamine lesions decrease hippocampal glucocorticoid and mineralocorticoid receptor messenger ribonucleic acid expression. J Neuroendocrinol 2:911–916
Sladek FM, Seidel SD (2001) Hepatocyte nuclear factor 4a. In: McCabe ERB (ed) Nuclear receptors and genetic disease. Academic, London, pp 309–361
Torres-Padilla ME, Fougere-Deschatrette C, Weiss MC (2001) Expression of HNF4alpha isoforms in mouse liver development is regulated by sequential promoter usage and constitutive 3′ end splicing. Mech Dev 109:183–193
Zhong W, Mirkovitch J, Darnell JE Jr (1994) Tissue-specific regulation of mouse hepatocyte nuclear factor 4 expression. Mol Cell Biol 14:7276–7284
Drewes T, Senkel S, Holewa B, Ryffel GU (1996) Human hepatocyte nuclear factor 4 isoforms are encoded by distinct and differentially expressed genes. Mol Cell Biol 16:925–931
Lindros KO, Oinonen T, Issakainen J, Nagy P, Thorgeirsson SS (1997) Zonal distribution of transcripts of four hepatic transcription factors in the mature rat liver. Cell Biol Toxicol 13:257–262
Kuo CJ, Conley PB, Chen L, Sladek FM, Darnell JE Jr, Crabtree GR (1992) A transcriptional hierarchy involved in mammalian cell-type specification. Nature 355:457–461
Duncan SA, Navas MA, Dufort D, Rossant J, Stoffel M (1998) Regulation of a transcription factor network required for differentiation and metabolism. Science 281:692–695
Tian JM, Schibler U (1991) Tissue-specific expression of the gene encoding hepatic nuclear factor 1 may involve nuclear factor 4. Genes Dev 5:2225–2234
Stafford JM, Waltner-Law M, Granner DK (2001) Role of accessory factors and steroid receptor coactivator 1 in the regulation of phosphoenolpyruvate carboxykinase gene transcription by glucocorticoids. J Biol Chem 276:3811–3819
Yoon JC, Puigserver P, Chen G et al (2001) Control of hepatic gluconeogenesis through the transcriptional coactivator PGC-1. Nature 413:131–138
Rhee J, Inoue Y, Yoon JC et al (2003) Regulation of hepatic fasting response by PPARgamma coactivator-1alpha (PGC-1): requirement for hepatocyte nuclear factor 4alpha in gluconeogenesis. Proc Natl Acad Sci USA 100:4012–4017
Crosson SM, Davies GF, Roesler WJ (1997) Hepatic expression of CCAAT/enhancer binding protein α: hormonal and metabolic regulation in rats. Diabetologia 40:1117–1124
Hayhurst GP, Lee YH, Lambert G, Ward JM, Gonzalez FJ (2001) Hepatocyte nuclear factor 4alpha (nuclear receptor 2A1) is essential for maintenance of hepatic gene expression and lipid homeostasis. Mol Cell Biol 21:1393–1403
Yoon JC, Puigserver P, Chen G et al (2001) Control of hepatic gluconeogenesis through the transcriptional coactivator PGC-1. Nature 413:131–138
Odom DT, Zizlsperger N, Gordon DB et al (2004) Control of pancreas and liver gene expression by HNF transcription factors. Science 303:1378–1381
Naiki T, Nagaki M, Shidoji Y et al (2002) Analysis of gene expression profile induced by hepatocyte nuclear factor 4alpha in hepatoma cells using an oligonucleotide microarray. J Biol Chem 277:14011–14019
Ghoshal S, Pasham S, Odom DP, Furr HC, McGrane MM (2003) Vitamin A depletion is associated with low phosphoenolpyruvate carboxykinase mRNA levels during late foetal development and at birth in mice. J Nutr 133:2131–2136
Cassuto H, Kochan K, Chakravarty K et al (2005) Glucocorticoids regulate transcription of the gene for phosphoenolpyruvate carboxykinase in the liver via an extended glucocorticoid regulatory unit. J Biol Chem 280:33873–33884
Nakhei H, Lingott A, Lemm I, Ryffel GU (1998) An alternative splice variant of the tissue specific transcription factor HNF4alpha predominates in undifferentiated murine cell types. Nucleic Acids Res 26:497–504
Bailly A, Torres-Padilla ME, Tinel AP, Weiss MC (2001) An enhancer element 6 kb upstream of the mouse HNF4alpha1 promoter is activated by glucocorticoids and liver-enriched transcription factors. Nucleic Acids Res 29:3495–3505
Acknowledgements
This study was supported by the Wellcome Trust (J. R. Sekl, K. E. Chapman), Scottish Hospital Endowments Research Trust (SHERT; M. J. Nyirenda, J. R. Sekl) and the Beit Memorial Fund (M. J. Nyirenda). We thank members of the Endocrine Unit, particularly M. Lai and J. Nixon, for helpful advice and many useful discussions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nyirenda, M.J., Dean, S., Lyons, V. et al. Prenatal programming of hepatocyte nuclear factor 4α in the rat: a key mechanism in the ‘foetal origins of hyperglycaemia’?. Diabetologia 49, 1412–1420 (2006). https://doi.org/10.1007/s00125-006-0188-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0188-5