Abstract
Aims/hypothesis
The aim of this study was to investigate the effects of lifestyle intervention on the levels of plasminogen activator inhibitor (PAI-1) and fibrinogen in subjects participating in the Finnish Diabetes Prevention Study (DPS).
Methods
In five DPS centres, 321 subjects with impaired glucose tolerance (intervention group, n=163; control group, n=158) had their PAI-1 and fibrinogen levels measured at baseline and at the 1-year follow-up. Additional 3-year follow-up assessments were carried out in a sample of 97 subjects in one of the DPS centres (Turku). The intervention programme included an intensive lifestyle intervention aiming at weight reduction, healthy diet and increased physical activity.
Results
During the first intervention year, PAI-1 decreased by 31% in the intervention group but showed no change in the control group (p<0.0001). In the Turku subgroup, the decrease in PAI-1 persisted throughout the 3-year follow-up. Changes in PAI-1 were associated with the number of lifestyle changes made during the first year (p=0.008). Weight reduction was the most important factor explaining the decrease in PAI-1. Changes in fibrinogen levels did not differ between the groups.
Conclusions/interpretation
In addition to the previously reported reduction in the risk of type 2 diabetes in DPS participants with impaired glucose tolerance, the intensive dietary and exercise intervention had beneficial long-term effects on fibrinolysis as indicated by the reduced levels of PAI-1. These results suggest that elevated PAI-1 levels in obese subjects with impaired glucose tolerance are mostly reversible by lifestyle changes, especially those geared to weight reduction.
Similar content being viewed by others
Introduction
Subjects with type 2 diabetes have an increased risk of atherosclerotic and thrombotic complications, leading to increased morbidity and mortality from CHD or cerebrovascular and peripheral vascular diseases [1, 2]. Even subjects with milder disturbances in glucose metabolism, such as IGT, are at an increased risk of cardiovascular disease [3, 4].
Several studies have shown that high plasma fibrinogen levels represent an independent marker for cardiovascular morbidity in both non-diabetic [5] and diabetic [6] subjects. Diabetic subjects have higher fibrinogen levels than the general population [7], but the data on subjects with IGT are contradictory [8, 9]. Plasminogen activator inhibitor (PAI-1) is a fast-acting inhibitor of fibrinolysis. It has been proposed that decreased fibrinolytic activity and increased circulating PAI-1 play a role in thrombosis/fibrinolysis and contribute to the development of cardiovascular disease in the metabolic syndrome and type 2 diabetes [10]. Some, but not all, studies have reported raised PAI-1 levels in subjects with IGT [11, 12]. A high PAI-1 level may also be a predictor for the development of type 2 diabetes [13, 14].
The effects of physical activity on PAI-1 and fibrinogen levels in healthy subjects are contradictory [15, 16]. Weight reduction has been associated with reductions in both PAI-1 [17, 18] and fibrinogen [17] in obese subjects. A weight-reducing diet combined with exercise has had beneficial effects on fibrinolysis in subjects with or without glucose intolerance over a period of 1 year in some [19, 20] but not all [21] studies. However, there are no studies with long-term follow-up.
The Finnish Diabetes Prevention Study (DPS) showed that intensive lifestyle intervention reduced the risk of type 2 diabetes by 58% in IGT subjects [22]. This analysis aimed both to evaluate the effects of this intervention on changes in PAI-1 and fibrinogen during the first year of the intervention and to determine whether these changes persisted during the subsequent years.
Subjects and methods
Subjects and study design
The DPS was a randomised, controlled study carried out in five study centres in Finland from 1993 to 2000. The study design and methods have been described in detail elsewhere [22–24]. In brief, a total of 522 subjects with IGT were randomised into either a lifestyle intervention group or a control group receiving the usual care. The inclusion criteria were as follows: overweight (BMI>25 kg/m2), age 40–64 years at randomisation, and IGT according to the World Health Organization (WHO) 1985 criteria [25]. The subjects were randomly assigned to one of the two treatment modalities, the intensive lifestyle intervention group or a control group. The intervention aimed at weight reduction, increased physical activity and a low-saturated-fat, high-fibre diet. The study was approved by the ethics committee of the National Public Health Institute in Helsinki, Finland. All participants gave written informed consent.
Of the DPS participants, 321 subjects (intervention group, n=163; control group, n=158) had blood drawn and plasma stored for the analysis of PAI-1 and fibrinogen at baseline and at the 1-year follow-up. These subjects were from all five centres. However, because some of the centres recruiting study subjects did not initially include plasma sampling for PAI-1 and fibrinogen in their study protocol, the number of subjects with blood specimens is less than the total number of subjects in the entire DPS. In one study centre (Turku) the haemostatic variables were also analysed at the 3-year follow-up. Of the original 110 subjects in that study group (intervention, n=55; control, n=55), 15 subjects developed diabetes during the first or second year and did not attend the 3-year follow-up and four subjects dropped out; thus, 91 subjects (intervention, n=49, control, n=42) formed the study population at the 3-year follow-up.
Data collection
At baseline and at each annual visit, blood samples were drawn in the morning after a minimum of 10 h fasting. All subjects underwent a 2-h 75-g OGTT, their medical history and nutrient intake were recorded, and physical examinations were performed [23]. The nutrient intakes were calculated from 3-day food diaries using a program developed at the National Public Health Institute [26]. Leisure-time physical activity (LTPA) was assessed as described earlier [24, 27, 28]. The goals of lifestyle changes during the first year (weight reduction ≥5%, physical activity with moderate intensity ≥30 min/day, dietary fat <30% of total energy intake [E%], saturated fat <10 E%, and fibre ≥15 g/1000 kcal) were summed up as a success score, as reported earlier [22].
Biochemical assessments
Methods for the determination of glucose, HbA1c, insulin and serum lipids have been described previously [23]. Insulin resistance was estimated by the homeostatic model assessment (HOMA-IR) method as previously described [(fasting insulin in mU/l×fasting glucose in mmol/l)/22.5] [29]. Blood for haemostatic assessments was drawn after the other specimens with minimal stasis. The samples were centrifuged immediately. Plasma was collected and immediately frozen and stored at −70°C. Plasma fibrinogen was measured by liquid-phase immunoprecipitation assay with nephelometric end-point detection (Turbox Fibrinogen Assay, Orion Diagnostica, Espoo, Finland). Intra-assay variation was 2.0% and inter-assay variation was 4.9% at the 3.8 g/l level. PAI-1 activity was assessed by a chromogenic method based on two-stage, indirect enzymatic assay (Spectrolyse/pL PAI; Biopool International, Ventura, CA, USA). Intra-assay variations were 2.8% at the 17.5 U/ml level and 2.3% at the 28.7 U/ml level. The corresponding inter-assay variations were 4.8% and 8.6%. Fibrinogen and PAI-1 levels were analysed in the laboratory of the Research Department of the Social Insurance Institution.
Statistical analysis
Two-sided Student’s t-test or the non-parametric Wilcoxon’s signed-rank test was used to analyse the differences between the intervention and control groups. The changes in variables were analysed using a general linear mixed model with repeated measures. Logarithmic or square-root transformations were applied, if necessary. The validity of the models was evaluated with residual analysis. If the validity of the models was not fulfilled, Wilcoxon’s signed-rank test was applied. Untransformed data are presented in the tables. Group and centre were included in the model as the between-subjects factors and time as the within-subject factor. Mean changes in both groups were assessed by contrast with the 95% confidence intervals, regardless of whether or not the group×time interaction was significant. The association between PAI-1 and the other factors was tested with repeated ANOVA defining weight, HbA1c, 2-h glucose, HOMA-IR, dietary fat as E%, saturated fat as E%, intake of dietary fibre, and moderate to vigorous LTPA as time-dependent covariates, and group as a between-subjects factor. R 2 values for changes between PAI-1 and independent variables were calculated separately by regression analysis. The linear trend in success score and PAI-1 changes was tested by one-way ANOVA. All statistical analyses were conducted with SAS version 8.2 (SAS Institute, Cary, NC, USA). Statistical significance was taken as a p value of 0.05 or less.
Results
The 321 subjects with haemostatic measurements did not differ from the rest of the study population (n=201), except for fasting glucose (6.26±0.71 mmol/l vs 5.94±0.77 mmol/l, p<0.0001). The differences in baseline characteristics between the subjects in the intervention group and the control group were not significant, except for the dietary fat and saturated fat intakes, which were higher in the control group (Table 1).
During the first year, the weight reduction was 4.7 kg (5%) in the intervention group, compared with 1.1 kg (1%) in the control group (p<0.0001) (Table 2). The intake of dietary and saturated fat as E% decreased in both groups, but the intake of saturated fat decreased by a significantly greater degree in the intervention group (19% vs 9%, p=0.01). Subjects in the intervention group increased their intake of dietary fibre by a significantly greater amount than control subjects (p<0.0001). Moderate to vigorous LTPA increased markedly in the intervention group (25%, p<0.0005), but only slightly in the control group (4%, p=0.02). HbA1c and fasting glucose decreased in the intervention group (1% and 5%, respectively) while in the control group HbA1c increased by 3% and fasting glucose did not change. The decreases in 2-h glucose, fasting insulin and 2-h insulin were also larger in the intervention group.
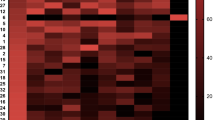
PAI-1 activity decreased significantly after the 1-year intervention (31%), but no change was observed in the control group. Fibrinogen did not change during the 1-year period in either group. PAI-1 changes were associated with the success score at 1-year follow-up: the higher the score the larger the decrease in PAI-1 (p=0.008) (Fig. 1). During the first follow-up year, PAI-1 decreased more in subjects who did not develop diabetes (n=251) than in those (n=70) who did during the DPS follow-up of 3.2 years (6.2±17.3 U/ml vs 0.5±22.1 U/ml, p=0.02).
Changes in PAI-1 during the first year according to the Success Score. The Score describes the number of the predefined lifestyle goals achieved. The linear trend in the success score and PAI-1 changes was significant, p=0.008. The description of the score is given in the Subjects and Methods section. The numbers below the bars indicate the number of subjects in each category
The most important factor explaining the change in PAI-1 was the change in weight (R 2 10.7%, p<0.0001). Other explanatory factors were the following: insulin resistance (HOMA-IR) (R 2 6.3%, p<0.0001), fat intake (R 2 5.6%, p<0.0001), fibre intake (R 2 4.4%, p=0.0002), saturated fat intake (R 2 3.7%, p=0.0005), 2-h glucose (R 2 2.7%, p=0.003) and LTPA (R 2 2.1%, p=0.01). In the final model, including weight, fat intake, and moderate to vigorous LTPA as covariates, the change in PAI-1 in the intervention group was reduced from the unadjusted value of −9.4 U/ml (95% CI −12.2 to −6.7) to −5.2 U/ml (95% CI −8.1 to −2.3) (Table 3).
In the Turku subgroup, levels of PAI-1 at the 1- and 3-year follow-ups compared with the baseline values remained the same in the intervention group (−35% vs −37%) while the decrease in the control group was greater at the 3-year follow-up than at 1-year (−23% vs −9%). PAI-1 changes with group×time interaction were still significant (p=0.009). The changes in fibrinogen at 1 and 3 years were −1% vs −10% in the intervention group and −1% vs −5% in the control group (p=0.38).
Discussion
The Finnish DPS showed that intensive dietary and exercise intervention had long-term beneficial effects on fibrinolysis as measured by the plasma PAI-1 level. The decrease in PAI-1 was associated with weight reduction. During the first year, the subjects in the intervention group lost an average of 4.7 kg and their PAI-1 activity decreased by 31%. The decrease in PAI-1 persisted in our intervention group, and so did the decrease of weight, up to the 3-year follow-up. To our knowledge, no other report has covered such a long follow-up period. Our 1-year results are in accordance with those previously obtained in a Swedish study [20]. In connection with the weight decline, our subjects’ insulin sensitivity improved, which may partly explain the reduction in PAI-1 [30]. Surprisingly, there is one lifestyle intervention study in which marked weight loss and a decrease in insulin resistance were not accompanied by any decrease in PAI-1 [21]. The decline of PAI-1 has been shown to be more closely related to changes in adipose tissue than to changes in insulin levels [31]. Several studies have shown decreased PAI-1 levels after weight loss [17, 18, 30–32], and the decrease seems to depend on the magnitude of the weight loss [17]. Furthermore, the PAI-1 level has been shown to increase when weight is regained [31].
Besides weight loss, changes in energy intake from fat, saturated fat and dietary fibre were associated with the PAI-1 decrease. Fibre intake, however, had no independent explanatory power, as has been shown previously [33, 34]. All changes in the dietary components were connected with changes in weight. It seems probable that neither modification of dietary fat composition alone nor a reduction of dietary fat intake will alter the PAI-1 levels without the occurrence of a significant weight loss [35, 36].
In our study, exercise training had a smaller impact on the PAI-1 levels than the decrease in weight. The participants were at first advised to change their diet, and the exercise programmes did not start until after the first 6 months of the DPS. The intervention group was advised and supervised to carry out individually tailored progressive exercise programmes including resistance training throughout the study period. Consequently, the changes in fibrinogen were greater after the third year than after the first year. The effects of exercise may be partly mediated by visceral fat loss [37], which can determine PAI-1 levels [31, 38, 39]. The type and intensity of exercise may be important because in some studies exercise has caused no additional effect after dieting [40]. High-intensity exercise may be needed to induce significant changes in PAI-1 levels [41, 42]. We have previously shown that the increase in moderate to vigorous physical activity decreased the risk of type 2 diabetes in subjects with IGT [28]. However, all life-style changes are important, and in our study they all explained the PAI-1 decrease; the better the intervention goals were achieved, the greater was the decrease in PAI-1.
The results of the intervention persisted for 3 years, but the difference between the intervention and control groups diminished, because PAI-1 decreased in the control group, too. One explanation may be that subjects developing diabetes during the first and second years did not take part in the 3-year follow-up and all but two of these belonged to the control group. Since those developing diabetes had no decrease in PAI-1 at year 1, if tested, they would probably also have no decline at 3 years. Thus, their absence from the 3-year data results in a greater decrease in PAI-1 at 3 years compared with 1 year among subjects in the control group.
The changes in fibrinogen levels were small during the first year, which is in line with many dietary and exercise intervention studies on subjects with or without glucose intolerance [17, 18, 32, 34–36, 40, 43]. The reason may be that the change in weight was relatively small. One study that found an average weight loss of 13.6 kg showed a marked decline in fibrinogen [18]. In one lifestyle intervention study the beneficial effect of intervention on fibrinogen was actually the result of the increase in fibrinogen in the control group, while the decrease in the intervention group was not significant [20]. Diabetic patients with higher physical activity and higher aerobic power had lower fibrinogen concentrations in plasma [44], but in exercise intervention studies comprising normal or diabetic subjects the changes in fibrinogen have been conflicting [42, 45–47]. In the DPP study, after the first year the change in fibrinogen was −2% in the lifestyle group [48], which is slightly more than in our study. At the 3-year follow-up we found a decrease of 10% in the fibrinogen level in the intervention group. This may be the result of the moderate to vigorous exercise, which was reported to increase markedly [28]. Thus, intensive exercise may be necessary to achieve a significant decrease in fibrinogen [42].
In conclusion, intensive lifestyle intervention, which reduced the risk of type 2 diabetes in IGT subjects, was accompanied by a marked decrease in PAI-1 levels. The decrease of PAI-1 was mainly explained by weight reduction. Thus, these favourable changes in the fibrinolytic system and metabolic factors in IGT subjects can improve the cardiovascular profile in these high-risk individuals.
Abbreviations
- DPS:
-
Diabetes Prevention Study
- E%:
-
per cent of total energy intake
- HOMA-IR:
-
homeostasis model assessment for insulin resistance
- LTPA:
-
leisure-time physical activity
- PAI-1:
-
plasminogen activator inhibitor-1
- WHO:
-
World Health Organization
References
Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M (1998) Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 339:229–234
Kannel WB, McGee DL (1979) Diabetes and glucose tolerance as risk factors for cardiovascular disease: the Framingham study. Diabetes Care 2:120–126
Qiao Q, Jousilahti P, Eriksson J, Tuomilehto J (2003) Predictive properties of impaired glucose tolerance for cardiovascular risk are not explained by the development of overt diabetes during follow-up. Diabetes Care 26:2910–2914
Kuller LH, Velentgas P, Barzilay J, Beauchamp NJ, O’Leary DH, Savage PJ (2000) Diabetes mellitus: subclinical cardiovascular disease and risk of incident cardiovascular disease and all-cause mortality. Arterioscler Thromb Vasc Biol 20:823–829
Ernst E, Resch KL (1993) Fibrinogen as a cardiovascular risk factor: a meta-analysis and review of the literature. Ann Intern Med 118:956–963
Ceriello A (1997) Fibrinogen and diabetes mellitus: is it time for intervention trials? Diabetologia 40:731–734
Kannel WB, D’Agostino RB, Wilson PW, Belanger AJ, Gagnon DR (1990) Diabetes, fibrinogen, and risk of cardiovascular disease: the Framingham experience. Am Heart J 120:672–676
Haffner SM, D’Agostino R Jr, Festa A et al (2003) Low insulin sensitivity (S(i)=0) in diabetic and nondiabetic subjects in the insulin resistance atherosclerosis study: is it associated with components of the metabolic syndrome and nontraditional risk factors? Diabetes Care 26:2796–2803
Lam TH, Liu LJ, Janus ED, Lam KS, Hedley AJ (2000) Fibrinogen, other cardiovascular risk factors and diabetes mellitus in Hong Kong: a community with high prevalence of Type 2 diabetes mellitus and impaired glucose tolerance. Diabet Med 17:798–806
Juhan-Vague I, Alessi MC, Vague P (1996) Thrombogenic and fibrinolytic factors and cardiovascular risk in non-insulin-dependent diabetes mellitus. Ann Med 28:371–380
Meigs JB, Mittleman MA, Nathan DM et al (2000) Hyperinsulinemia, hyperglycemia, and impaired hemostasis: the Framingham Offspring Study. JAMA 283:221–228
Nagi DK, Mohamed Ali V, Jain SK, Walji S, Yudkin JS (1996) Plasminogen activator inhibitor (PAI-1) activity is elevated in Asian and Caucasian subjects with non-insulin-dependent (type 2) diabetes but not in those with impaired glucose tolerance (IGT) or non-diabetic Asians. Diabet Med 13:59–64
Eliasson MC, Jansson JH, Lindahl B, Stegmayr B (2003) High levels of tPA antigen precede the development of type 2 diabetes in a longitudinal population study. The Northern Sweden MONICA Study. Cardiovasc Diabetol 2:19
Haffner SM (2003) Insulin resistance, inflammation, and the prediabetic state. Am J Cardiol 92:18J–26J
Lee KW, Lip GY (2003) Effects of lifestyle on hemostasis, fibrinolysis, and platelet reactivity: a systematic review. Arch Intern Med 163:2368–2392
El-Sayed MS, Sale C, Jones PG, Chester M (2000) Blood hemostasis in exercise and training. Med Sci Sports Exerc 32:918–925
Rissanen P, Vahtera E, Krusius T, Uusitupa M, Rissanen A (2001) Weight change and blood coagulability and fibrinolysis in healthy obese women. Int J Obes Relat Metab Disord 25:212–218
Marckmann P, Toubro S, Astrup A (1998) Sustained improvement in blood lipids, coagulation, and fibrinolysis after major weight loss in obese subjects. Eur J Clin Nutr 52:329–333
Hamdy O, Ledbury S, Mullooly C et al (2003) Lifestyle modification improves endothelial function in obese subjects with the insulin resistance syndrome. Diabetes Care 26:2119–2125
Lindahl B, Nilsson TK, Jansson JH, Asplund K, Hallmans G (1999) Improved fibrinolysis by intense lifestyle intervention. A randomized trial in subjects with impaired glucose tolerance. J Intern Med 246:105–112
Torjesen PA, Birkeland KI, Anderssen SA, Hjermann I, Holme I, Urdal P (1997) Lifestyle changes may reverse development of the insulin resistance syndrome. The Oslo Diet and Exercise Study: a randomized trial. Diabetes Care 20:26–31
Tuomilehto J, Lindström J, Eriksson JG et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350
Eriksson J, Lindström J, Valle T et al (1999) Prevention of Type II diabetes in subjects with impaired glucose tolerance: the Diabetes Prevention Study (DPS) in Finland. Study design and 1-year interim report on the feasibility of the lifestyle intervention programme. Diabetologia 42:793–801
Lindström J, Louheranta A, Mannelin M et al (2003) The Finnish Diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 26:3230–3236
World Health Organization Expert Committee (1985) Diabetes mellitus. WHO, Geneva
Ovaskainen M-L, Valsta L, Lauronen J (1996) The compilation of food analysis values as a database for dietary values: the Finnish experience. Food Chem 57:133–136
Lakka TA, Salonen JT (1992) Intra-person variability of various physical activity assessments in the Kuopio Ischaemic Heart Disease Risk Factor Study. Int J Epidemiol 21:467–472
Laaksonen DE, Lindström J, Lakka TA et al (2005) Physical activity in the prevention of type 2 diabetes: the Finnish Diabetes Prevention Study. Diabetes 54:158–165
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Mavri A, Alessi MC, Bastelica D et al (2001) Subcutaneous abdominal, but not femoral fat expression of plasminogen activator inhibitor-1 (PAI-1) is related to plasma PAI-1 levels and insulin resistance and decreases after weight loss. Diabetologia 44:2025–2031
Mavri A, Stegnar M, Krebs M, Sentocnik JT, Geiger M, Binder BR (1999) Impact of adipose tissue on plasma plasminogen activator inhibitor-1 in dieting obese women. Arterioscler Thromb Vasc Biol 19:1582–1587
Folsom AR, Qamhieh HT, Wing RR et al (1993) Impact of weight loss on plasminogen activator inhibitor (PAI-1), factor VII, and other hemostatic factors in moderately overweight adults. Arterioscler Thromb 13:162–169
Turpeinen AM, Juntunen K, Mutanen M, Mykkänen H (2000) Similar responses in hemostatic factors after consumption of wholemeal rye bread and low-fiber wheat bread. Eur J Clin Nutr 54:418–423
Marckmann P, Sandström B, Jespersen J (1993) Favorable long-term effect of a low-fat/high-fiber diet on human blood coagulation and fibrinolysis. Arterioscler Thromb 13:505–511
Marckmann P, Sandström B, Jespersen J (1992) Fasting blood coagulation and fibrinolysis of young adults unchanged by reduction in dietary fat content. Arterioscler Thromb 12:201–205
Niskanen L, Schwab US, Sarkkinen ES, Krusius T, Vahtera E, Uusitupa MI (1997) Effects of dietary fat modification on fibrinogen, factor VII, and plasminogen activator inhibitor-1 activity in subjects with impaired glucose tolerance. Metabolism 46:666–672
Giannopoulou I, Ploutz-Snyder LL, Carhart R et al (2005) Exercise is required for visceral fat loss in postmenopausal women with type 2 diabetes. J Clin Endocrinol Metab 90:1511–1518
Cigolini M, Targher G, Bergamo Andreis IA, Tonoli M, Agostino G, De Sandre G (1996) Visceral fat accumulation and its relation to plasma hemostatic factors in healthy men. Arterioscler Thromb Vasc Biol 16:368–374
Janand-Delenne B, Chagnaud C, Raccah D, Alessi MC, Juhan-Vague I, Vague P (1998) Visceral fat as a main determinant of plasminogen activator inhibitor 1 level in women. Int J Obes Relat Metab Disord 22:312–317
Svendsen OL, Hassager C, Christiansen C, Nielsen JD, Winther K (1996) Plasminogen activator inhibitor-1, tissue-type plasminogen activator, and fibrinogen: effect of dieting with or without exercise in overweight postmenopausal women. Arterioscler Thromb Vasc Biol 16:381–385
El-Sayed MS (1996) Effects of high and low intensity aerobic conditioning programs on blood fibrinolysis and lipid profile. Blood Coagul Fibrinolysis 7:484–490
Stratton JR, Chandler WL, Schwartz RS et al (1991) Effects of physical conditioning on fibrinolytic variables and fibrinogen in young and old healthy adults. Circulation 83:1692–1697
Rauramaa R, Väisänen SB (1999) Physical activity in the prevention and treatment of a thrombogenic profile in the obese: current evidence and research issues. Med Sci Sports Exerc 31:S631–S634
Vanninen E, Laitinen J, Uusitupa M (1994) Physical activity and fibrinogen concentration in newly diagnosed NIDDM. Diabetes Care 17:1031–1038
Ponjee GA, Janssen GM, van Wersch JW (1993) Prolonged endurance exercise and blood coagulation: a 9 month prospective study. Blood Coagul Fibrinolysis 4:21–25
Zanettini R, Bettega D, Agostoni O et al (1997) Exercise training in mild hypertension: effects on blood pressure, left ventricular mass and coagulation factor VII and fibrinogen. Cardiology 88:468–473
Schuit AJ, Schouten EG, Kluft C, de Maat M, Menheere PP, Kok FJ (1997) Effect of strenuous exercise on fibrinogen and fibrinolysis in healthy elderly men and women. Thromb Haemost 78:845–851
Haffner S, Temprosa M, Crandall J et al (2005) Intensive lifestyle intervention or metformin on inflammation and coagulation in participants with impaired glucose tolerance. Diabetes 54:1566–1572
Acknowledgements
We are deeply indebted to all DPS research team members for their contribution to the study. The DPS was supported by grants from the Finnish Academy, the Ministry of Education, the Novo Nordisk Foundation, the Yrjö Jahnsson Foundation, the Juho Vainio Foundation and the Finnish Diabetes Research Foundation. The authors wish to thank A. Kylliäinen for her skilful technical and statistical assistance, and AL. Leino for taking care of the laboratory analysis of haemostatic indices.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Hämäläinen, H., Rönnemaa, T., Virtanen, A. et al. Improved fibrinolysis by an intensive lifestyle intervention in subjects with impaired glucose tolerance. The Finnish Diabetes Prevention Study. Diabetologia 48, 2248–2253 (2005). https://doi.org/10.1007/s00125-005-1938-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1938-5