Abstract
Although there is abundant evidence that hyperglucagonaemia plays a key role in the development of hyperglycaemia in type 2 diabetes, efforts to understand and correct this abnormality have been overshadowed by the emphasis on insulin secretion and action. However, recognition that the incretin hormone glucagon-like peptide-1 (GLP-1) exerts opposing effects on glucagon and insulin secretion has revived interest in glucagon, the neglected partner of insulin, in the bihormonal hypothesis. In healthy subjects, glucagon secretion is regulated by a variety of nutrient, neural and hormonal factors, the most important of which is glucose. The defect in alpha cell function that occurs in type 2 diabetes reflects impaired glucose sensing. GLP-1 inhibits glucagon secretion in vitro and in vivo in experimental animals, and suppresses glucagon release in a glucose-dependent manner in healthy subjects. This effect is also evident in diabetic patients, but GLP-1 does not inhibit glucagon release in response to hypoglycaemia, and may even enhance it. Early clinical studies with agents acting through GLP-1 signalling mechanisms (e.g. exenatide, liraglutide and vildagliptin) suggest that GLP-1 can improve alpha cell glucose sensing in patients with type 2 diabetes. Therapeutic approaches based around GLP-1 have the potential to improve both alpha cell and beta cell function, and could be of benefit in patients with a broad range of metabolic disorders.
Similar content being viewed by others
Introduction
Thirty years ago, Unger and Orci proposed a ‘bihormonal hypothesis’ to explain the origin of hyperglycaemia in diabetes [1]. They cited convincing evidence that, in addition to relative or absolute hypoinsulinaemia, relative hyperglucagonaemia is essential in the pathogenesis of diabetes mellitus. Since that time, and despite further evidence implicating alpha cell dysfunction in the development of type 2 diabetes, beta cell function and insulin resistance remain central to most discussions concerning the pathogenesis and treatment of this disorder. However, it should be recognised that the increased ‘demand’ for insulin imposed by insulin resistance can be countered by reducing glucagon secretion, as well as by increasing the secretion of insulin.
We will review normal alpha cell function and its clinical measurement, and will examine the abnormalities of alpha cell function that occur in type 2 diabetes. The influence of the incretin hormone glucagon-like peptide-1 (GLP-1) on alpha cell function in vitro and in experimental animals, healthy humans and diabetic patients will then be discussed. We conclude with a survey of recent studies describing the acute and chronic actions of potential new therapeutic agents that use GLP-1 signalling mechanisms in the treatment of type 2 diabetes.
Normal alpha cell function
As with the beta cell, regulation of alpha cell function is complex, with a range of nutrient, neural and hormonal influences upon glucagon secretion. Glucose is perhaps the most important physiological regulator of alpha cell function, and profoundly suppresses glucagon secretion. In the perfused rat pancreas, threshold, half-maximal and maximal alpha cell responses to glucose occur at approximately 2.5, 5.0 and 10.0 mmol/l glucose [2]. Following an overnight fast, plasma glucagon rises in humans if glucose falls below a threshold of approximately 3.8 mmol/l [3] and decreases progressively as plasma glucose rises above the normal range [4].
Most amino acids stimulate glucagon release, but the relative potency of individual amino acids varies between species [5]. Arginine is the most effective amino acid in man, and is often employed in provocative tests of both alpha cell and beta cell function [6]. NEFA and ketones also influence glucagon secretion. Although a physiological role of lipids is not established, NEFA and ketones have been reported to suppress glucagon secretion in vitro [7] and administration of lipid has been shown to decrease plasma glucagon levels in man [8].
The autonomic nervous system can exert a profound influence on glucagon secretion, and activation of either branch stimulates glucagon release [9, 10]. As detailed in Table 1, numerous hormones (many of which are also neurotransmitters) also affect glucagon release. Insulin suppresses glucagon secretion via a local endocrine effect [11]; somatostatin, by a paracrine effect [12]. Thus, alpha cells are exposed to very high concentrations of insulin and somatostatin, and there is some evidence to suggest that insulin mediates glucose inhibition of glucagon secretion [13] and that withdrawal of this local insulin ‘tone’ mediates the effect of hypoglycaemia on glucagon release [14]. There are, however, other mechanisms that influence hypoglycaemic stimulation of glucagon release [15, 16]. Stress hormones such as adrenaline stimulate glucagon secretion, and activation of both branches of the autonomic nervous system contributes to the glucagon response, particularly when hypoglycaemia is profound [17].
Each of the factors listed above act in a coordinated fashion to regulate glucagon secretion. Accordingly, in healthy subjects, glucagon levels increase in response to a high-protein meal and decrease in response to a high-carbohydrate meal or oral glucose [18], thereby minimising fluctuations in plasma glucose levels. During stress (e.g. hypoxia [19] or hyperthermia [20]), where it is advantageous to mobilise fuels, glucagon levels increase and, particularly in the case of hypoglycaemic stress, there are several other mechanisms that elevate glucagon levels [15] and protect against severe and possibly life-threatening consequences.
Text box 1
Glucose and a variety of hormones and substrates act in a coordinated manner to regulate glucagon secretion. Normal alpha cell function serves to protect against hypoglycaemia and to minimise prandial glucose excursions. |
Clinical measures of alpha cell function
The development of the insulin RIA introduced an unprecedented degree of specificity and sensitivity for the measurement of insulin [21], and was soon followed by a glucagon RIA [22]. The existence of larger molecular weight species of glucagon-like immunoreactivity of extrapancreatic origin made quantification of pancreatic glucagon difficult until specific antisera such as 30 K allowed the development of sensitive and specific assays for the 3,500 molecular weight species [23]. Even today, pancreatic specific assays yield a rather wide range of ‘basal’ glucagon values, e.g. 30–60 ng/l (∼8.6–17.2 pmol/l) in healthy subjects. This highlights the importance of comparing values only within a single study and using a single assay system. Since many pancreatic-specific assays ‘read’ a large molecular weight interference factor as glucagon (this is unrelated to glucagon and remains constant [24]), changes from baseline provide a more reliable assessment of in vivo glucagon secretion than basal fasting glucagon levels.
The most commonly used provocative test of alpha cell function involves administration of arginine, usually as an intravenous bolus of 5 g, which results in a maximum stimulation [6, 25]. The acute glucagon response to arginine (AGRarg) is a convenient measure of alpha cell responsiveness and is usually expressed as either the incremental AUC for 10 min or the mean increment above the prestimulus baseline from 2–5 min following arginine administration. Although other non-glucose secretagogues, such as isoproterenol, are also used in provocative tests of beta cell function [26], bolus administration of isoproterenol is less effective than arginine in stimulation of acute glucagon release in humans [27]. Acute insulin-induced hypoglycaemia has also been used to assess alpha cell function in humans [28], although arginine stimulation tests clearly pose less risk and are more routinely employed.
Just as glucose modifies the beta cell response to non-glucose stimuli, it also strongly influences the alpha cell response to other provocative stimuli. Hyperglycaemic clamps using variable-rate glucose infusions can therefore be combined with arginine stimulation tests to characterise alpha cell function more fully. Figure 1 shows results from a study in which the AGRarg was measured at basal glucose and at two levels of hyperglycaemia [25]; the glucagon response to arginine falls as glucose levels are increased.
Plasma levels of glucagon (a) and glucose (b) and the acute glucagon response to intravenous arginine bolus (AGRarg=10 min AUC) (c) during stepped hyperglycaemic clamps in healthy volunteers. The data in the upper two panels are from a single representative subject, while the data in the bottom panel are presented as means±SEM, n=16. Adapted from [25], Copyright 1982 American Diabetes Association. From Diabetes, Vol. 31, 1982; 489–495. Reprinted with permission from the American Diabetes Association
Assessment of the AGRarg at several glucose levels allows more rigorous definition of the influence of glucose on arginine-stimulated glucagon release, and quantification of alpha cell function can be derived from the data obtained. The minimum AGRarg (seen at plasma glucose levels above ∼25 mmol/l in healthy subjects [29]) and the slope of the linear portion of the curve provide information on the responsiveness of the alpha cell to glucose-induced suppression, and the PG50, the glucose level at which half-maximal suppression occurs, is a measure of alpha cell sensitivity to glucose. It should be noted that the PG50 may be underestimated if a minimum AGRarg is not achieved at the highest glucose level tested.

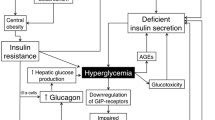
Abnormalities of alpha cell function in diabetes
As with beta cell dysfunction in type 2 diabetes, most—and perhaps even all—of the abnormalities of alpha cell function seen in this disorder may be considered to reflect an impairment of glucose sensing. Absolute fasting plasma levels of glucagon may or may not be higher in patients with type 2 diabetes than in non-diabetic subjects, but fasting hyperglucagonaemia is clearly present in the context of ambient glucose levels, and this contributes to the increased rate of hepatic glucose output seen in patients with type 2 diabetes [30–32]. Another manifestation of impaired glucose sensing by the alpha cell is the loss of hyperglycaemia-induced suppression of glucagon release. The magnitude of the reduction in plasma glucagon levels in response to glucose infusion [33], an oral glucose load [34] or a high carbohydrate meal [18] is considerably less in patients with type 2 diabetes than in those with NGT. In fact, as illustrated in Fig. 2, glucose may elicit a paradoxical stimulation of glucagon secretion in diabetic patients, particularly in those with more advanced disease [34]. It has also been suggested that the alpha cell is resistant to insulin [35]; however, it is difficult to distinguish between impaired glucose sensing and alpha cell insulin resistance.
Plasma glucagon levels during 50 g OGTTs in subjects with NGT (closed circles, n=6) and patients with type 2 diabetes classified as mild (fasting blood glucose <6.7 mmol/l, open triangles, n=11), moderate (6.7–11.1 mmol/l, closed triangles, n=8) or severe (>11.1 mmol/l, open circles, n=14). The data are presented as means±SEM. Adapted from [34]
The glucagon response to the stimulatory effect of arginine is higher in patients with type 2 diabetes than in non-diabetic subjects [36]. However, in view of the concurrent hyperglycaemia, it is difficult to distinguish hyper-responsiveness to arginine from faulty glucose sensing. Indeed, as illustrated in Fig. 3, the plasma glucose level required for half-maximal suppression of the AGRarg is substantially higher in diabetic subjects than in normal, glucose-tolerant subjects, suggesting that the sensitivity of the alpha cell to the suppressive effects of glucose is decreased [29].
Acute glucagon response to intravenous arginine bolus (AGRarg=mean level from 2–5 min) during stepped hyperglycaemic clamps in subjects with NGT (closed circles) and in patients with type 2 diabetes (open triangles). The data are presented as means±SEM, n=8 in each group. Adapted with permission and republished from [29]
One of the most clinically important aspects of alpha cell dysfunction in diabetes is a failure to respond appropriately to hypoglycaemia. A marked impairment is well documented in patients with type 1 diabetes [37] and those with long-standing type 2 diabetes [38], although the degree of impairment in patients with ‘mild’ type 2 diabetes is controversial [39], as are the relative contributions of altered pancreatic glucose sensing and autonomic failure [40]. Nonetheless, impaired alpha cell glucose sensing can result in inadequate glucagon secretion in response to decreases in plasma glucose, and thereby increased risk of severe hypoglycaemia, and in excessive glucagon secretion in the fasting [41] and postprandial states [42], which contribute to the development and progression of hyperglycaemia in type 2 diabetes.
Many of the manifestations of alpha cell dysfunction described above have been reported in subjects with IGT [6, 43, 44]. Furthermore, a prospective study of postmenopausal women found that the AGRarg at a clamped plasma glucose of 14 mmol/l was an independent predictor of glucose intolerance [45]. Such findings strongly support the bihormonal hypothesis [1] and attest to the importance of pancreatic glucagon. Accordingly, when GLP-1 was reported to augment insulin secretion and suppress glucagon in man [46], this newly discovered peptide became the focus of intense and continued research, holding promise for the treatment of type 2 diabetes.
Text box 2
There are clear defects in alpha cell function in patients with type 2 diabetes, including relative glucagon hypersecretion at normal and elevated glucose levels, and often an impaired response to hypoglycaemia. Thus, alpha cell dysfunction in diabetes may be described as inadequate glucose sensing. |
GLP-1
GLP-1 is a 30-amino acid peptide produced by L cells in the lower intestine by alternative processing of the gene encoding proglucagon [47]. The structure of GLP-1 was originally deduced from cDNA cloning of the gene encoding preproglucagon (GLP-1 [1–37]). However, GLP-1 [1–37] is inactive, requiring N-terminal truncation of amino acids 1–6 for activation. The biologically active forms of GLP-1 are GLP-1 [7–37] and GLP-1 [7–36] amide, previously known as insulinotropin [48], glucagon-like insulinotropic peptide (GLIP) [49] and truncated GLP-1 [50]. This latter designation is unhelpful, since inactivation of GLP-1 [7–37] and GLP-1 [7–36] amide occurs through further N-terminal truncation by the enzyme dipeptidyl peptidase IV (DPP-4), yielding GLP-1 [9–37] and GLP-1 [9–36] amide, which have also been referred to as truncated GLP-1. For the purposes of this paper, and consistent with recommendations arising from the first international symposium on GLP-1, the term GLP-1 will be used to designate either of the biologically active peptides, GLP-1 [7–37] and GLP-1 [7–36] amide.
GLP-1 is released from the gut in response to food intake and its most well-known physiological function is as an incretin [46], i.e. promoting assimilation of ingested nutrients via glucose-dependent stimulation of insulin release. The clinical potential of GLP-1-based therapies has received much attention and is the topic of several recent reviews, which have primarily focused on the beta cell [51–53]. However, GLP-1 also suppresses glucagon release [54], and this action may be as important as its insulinotropic effect in terms of its therapeutic properties.
Effects of GLP-1 on alpha cells in vitro
Although somewhat controversial [55], displaceable binding of GLP-1 to pancreatic cells that test positive for glucagon immunoreactivity has been reported [56], suggesting the existence of GLP-1 receptors on pancreatic alpha cells, and thus a direct effect of GLP-1 on glucagon secretion. Although GLP-1 augments Ca2+-dependent exocytosis in rat pancreatic alpha cells [57], GLP-1 has been shown to inhibit glucagon release from the perfused rat pancreas [58–61], isolated rat islets in static incubations [62], the perfused canine pancreas [60, 63], the perfused porcine pancreas, the perfused porcine nonantral stomach [64] and cultured human islets [65]. The glucagonostatic effect of GLP-1 does not appear to be mediated by a local endocrine effect of insulin, since glucagon release is inhibited even when insulin is unstimulated [61, 64]. This is supported by the observation that GLP-1 also inhibits glucagon release from a glucagon-secreting cell line [66].
The influence of ambient glucose on the effects of GLP-1 on glucagon secretion in vitro is not altogether clear. Many studies use a relatively low glucose level (∼3 mmol/l) in the perfusate or culture media, often with arginine or a mixture of amino acids to establish a high baseline secretory rate and thus a broad dynamic range. Under these conditions it has been shown that GLP-1 exerts an inhibitory effect on glucagon release [65, 67]. The effect of GLP-1 on alpha cell glucose sensing in vitro has not been assessed. One study with the GLP-1 agonist exenatide (previously known as exendin-4; a naturally occurring peptide isolated from salivary secretions of Heloderma suspectum) did examine glucagon release from the perfused rat pancreas in response to a square wave decrease in glucose level from 11 to 3.2 mmol/l, with or without GLP-1 infusion, and found a small suppressive effect of GLP-1 [68]. However, the alpha cell response to the glucose decrement alone was very modest. It would be of interest to assess the effect of either a glucose decrement on a background of GLP-1 with a perfusion system, or a full glucose dose response with or without co-incubation with GLP-1 in a static system.
Text box 3
In vitro studies show that GLP-1 or agonists can exert powerful inhibitory effects on glucagon secretion. The effects that have been described would generally be of benefit in the treatment of diabetes. More rigorous examination of the influence of GLP-1 on alpha cell glucose sensing will be needed to determine if therapies based on GLP-1 signalling mechanisms will actually improve alpha cell function vis-à-vis suppressing glucagon secretion under all circumstances. |
Effects of exogenous and endogenous GLP-1 on alpha cell function in experimental animals
The following sections will discuss the effects of exogenously administered GLP-1 or agonists such as exenatide and liraglutide (previously known as NN2211; a long-acting derivative of GLP-1 that is resistant to the actions of DPP-4) and will examine the effects of DPP-4 inhibitors such as vildagliptin (previously known as LAF237) and valine pyrrolidide, which act by increasing plasma levels of endogenously released GLP-1 and possibly other substrates such as glucose-dependent insulinotropic polypeptide (GIP). These sections will consider information regarding GLP-1 antagonists and neutralising antibodies that may provide information on the physiological role of endogenous GLP-1.
In normal mice fed an unrestricted diet, intravenous administration of GLP-1 had no influence on basal plasma glucagon levels but suppressed the acute stimulatory effect of co-injection of cholecystokinin (CCK) or the cholinergic agonist carbachol [69]. In normal rats, intravenous infusion of GLP-1 in the fed state reduced plasma glucagon, while glucose decreased from 7.3 to 5.6 mmol/l and insulin levels increased markedly but transiently. In contrast, in rats fasted for 48 h, the same rate of GLP-1 infusion increased plasma glucagon, and glucose fell from 5.0 to 4.4 mmol/l following transient stimulation of insulin. Thus, GLP-1 suppressed glucagon during modest hyperglycaemia, but did not inhibit the increase of glucagon in response to incipient hypoglycaemia [70].
In minipigs rendered glucose-intolerant with either nicotinamide or streptozotocin, intravenous injection of the GLP-1 derivative liraglutide was found to exaggerate plasma glucagon suppression induced by the hyperglycaemic clamp; however, glucagon increased promptly during the rapid decrease in glucose levels that followed termination of the clamp. Liraglutide therefore suppressed glucagon secretion during hyperglycaemia in these minipigs with IGT, but did not impair the response to falling glucose [71]. A physiological role of endogenous GLP-1 in the regulation of alpha cell function may be inferred from a study in healthy baboons using a peptide antagonist (exendin-[9–39]) [72]. In animals fasted overnight, plasma glucagon and glucose levels were higher during infusion with the antagonist than during a control saline infusion. Plasma insulin did not differ significantly between studies, suggesting that endogenous GLP-1 tonically restrains glucagon release.
Many recent studies have explored the effects of DPP-4 inhibition in experimental animals; plasma glucagon was measured in two of these studies. In the first study, 12 weeks of daily treatment with the DPP-4 inhibitor P32/98 did not affect fasting glucagon levels in the Vancouver diabetic fatty rat [73]. In the second study, acute administration of the DPP-4 inhibitor NVP-DPP728 suppressed the glucagon AUC(0–90 min) by ∼70% following a mixed meal in normal dogs. The difference between active and placebo treatment did not reach statistical significance, probably because of low sample size and substantial variability in response [74].
Text box 4
There are surprisingly few reports on the effects of GLP-1 agonists or antagonists on glucagon levels in experimental animals. Although some studies found no effect of GLP-1 on glucagon, most of the limited evidence available is consistent with the concept that GLP-1 improves alpha cell glucose sensing. |
Effects of exogenous and endogenous GLP-1 on alpha cell function in healthy humans
From the time of its discovery [75] and the first reports that it could stimulate insulin secretion [48], GLP-1 was considered a candidate incretin hormone. Kreymann et al. studied the potential contributions of GLP-1 and GIP to the incretin effect in healthy volunteers; GLP-1 raised insulin and suppressed basal glucagon when infused to mimic postprandial levels, whereas GIP increased glucagon [46]. Many subsequent studies have measured plasma glucagon, but few have focused on alpha cell function.
Subcutaneous injection of GLP-1 produced dose-related and parallel decreases in fasting plasma glucose and glucagon in healthy individuals [54]. GLP-1 infusion suppressed glucagon levels by ∼28% during glucose infusion to maintain steady-state euglycaemia. Insulin infusion in the same volunteers during steady-state euglycaemia had a less suppressive effect, suggesting that the effects of GLP-1 on plasma glucagon levels are not mediated exclusively by insulin; however, it is not clear whether local insulin levels were similar during the two protocols [76]. In studies examining the effects of GLP-1 infusion during a standardised mixed meal, GLP-1 markedly [77] or completely [78–80] suppressed the meal-induced increase in glucagon and essentially abolished prandial glucose excursions. In another study, however, GLP-1 had no effect on the degree of suppression of glucagon induced by intravenous glucose, although GLP-1 did significantly reduce basal glucagon [81].
The effects of GLP-1 or exenatide on glucagon levels during stepped hyperglycaemic and hypoglycaemic clamps provided the first information about GLP-1 receptor activation and alpha cell glucose sensing in human subjects. As illustrated in Fig. 4a, GLP-1 infusion during stepped hyperglycaemic clamps suppressed plasma glucagon during euglycaemia and had a progressively larger effect as glucose increased [82]. As illustrated in Fig. 4b, exenatide infusion suppressed plasma glucagon during euglycaemia, did not affect glucagon during moderate hypoglycaemia, and significantly increased plasma glucagon during more severe hypoglycaemia [83]. In a similar study of stepped hypoglycaemic clamps during GLP-1 infusion, GLP-1 suppressed glucagon levels during euglycaemia but had no detectable effect on plasma glucagon during hypoglycaemia [84]. Taken together, these findings demonstrate that GLP-1 suppresses glucagon secretion at normal and elevated glucose levels but does not inhibit, and may even modestly augment, glucagon secretion induced by hypoglycaemia.
(a) Plasma glucagon levels during stepped hyperglycaemic clamps in healthy volunteers during intravenous infusion of placebo (open bars) or GLP-1 (closed bars). The data are presented as means±SEM, n=8. Reprinted from [82] with permission from Elsevier. (b) Plasma glucagon levels during stepped hypoglycaemic clamps in healthy volunteers during intravenous infusion of placebo (open bars) or exendin-4 (closed bars). The data are presented as means±SEM, n=11. *p<0.05 vs placebo. Adapted from [83], Copyright 2004 American Diabetes Association. From Diabetes, Vol. 53, 2004; 2397–2403. Reprinted with permission from the American Diabetes Association
As in non-human primates, infusion of the GLP-1 antagonist exendin-[9–39] amide in healthy volunteers fasted overnight both blocked the glucagonostatic (and the insulinotropic) effects of exogenous GLP-1 and raised plasma glucagon in the absence of exogenous GLP-1 [85]. Plasma glucose increased, but insulin remained unchanged. This suggests that endogenous GLP-1 tonically restrains glucagon secretion in humans, and may indicate that GLP-1-based therapies could influence fasting, as well as postprandial, glucose.
Text box 5
GLP-1 and its agonists suppress glucagon secretion at euglycaemic and hyperglycaemic levels in healthy volunteers, but do not do so at hypoglycaemic levels. Thus, unlike other known modulators of glucagon release, GLP-1 appears to enhance alpha cell glucose sensing. |
Acute effects of exogenous and endogenous GLP-1 on alpha cell function in diabetes
Gutniak and colleagues demonstrated the glucagonostatic effect of GLP-1, both in patients with type 2 and type 1 diabetes [49] (Fig. 5) This study showed that the ‘diabetic’ alpha cell is responsive to GLP-1 despite its inability to respond appropriately to glucose, and that the effects of GLP-1 are not mediated by endogenous insulin, since they were evident in patients with type 1 diabetes. Several studies have confirmed that GLP-1 given as a subcutaneous injection [86, 87], a buccal tablet [88] or an intravenous infusion [89–91] before a mixed meal effectively prevents inappropriate meal-induced glucagon release and greatly reduces prandial glucose excursions in patients with type 2 diabetes. A dose-related reduction in meal-stimulated glucagon release by subcutaneous injection of GLP-1 was also demonstrated in patients with type 1 diabetes [92]. Since GLP-1 can slow gastric emptying, particularly at supraphysiological concentrations [90], these studies do not rule out the possibility that inhibition of gastric emptying (and, accordingly, a reduction of the stimulus for glucagon secretion) contributes to the observed effects. Further study will be needed to establish the relative contributions of delayed gastric emptying and effects on the alpha cell to the reduction in postmeal glucagon levels that occurs in response to agents that act through GLP-1 signalling mechanisms.
The plasma glucagon AUC(0–210 min) during a mixed meal in subjects with NGT (n=8), type 2 diabetes (T2DM, n=8) or type 1 diabetes (T1DM, n=8) during intravenous infusion of saline (closed bars) or GLP-1 (open bars). The data are presented as means±SEM. *p< 0.005 vs saline. Adapted from [49]
Studies of GLP-1 infusions in the fasting state have established that GLP-1 can directly inhibit glucagon release in patients with diabetes, irrespective of any effect on gastric emptying (Fig. 6) [93]. It should also be noted that glucagon levels rapidly increased as glucose levels approached the normal range, despite ongoing GLP-1 infusion, suggesting that GLP-1 may improve abnormal alpha cell glucose sensing in type 2 diabetes. The direct suppressive effect of GLP-1 infusion on fasting glucagon levels has further been demonstrated in patients with type 1 diabetes [94] and in patients with advanced type 2 diabetes after ‘sulphonylurea failure’ [95].
Plasma levels of glucose (a) and glucagon (b) in overnight-fasted patients with type 2 diabetes during intravenous infusion of placebo (closed circles) or GLP-1 (open triangles). The data are presented as means±SEM, n=10. *p<0.05 vs placebo. Reprinted from [93] with kind permission of Springer Science and Business Media
GLP-1 not only influences alpha cell function in individuals with diabetes, but is arguably more effective in patients with type 2 diabetes than in healthy subjects. Nauck and colleagues compared the influence of GLP-1 in patients with type 2 diabetes and in non-diabetic subjects [96]. As expected in healthy subjects, oral glucose or hyperglycaemic clamp suppressed plasma glucagon levels, whereas patients with type 2 diabetes showed a transient paradoxical increase in glucagon following oral glucose and failed to suppress during the hyperglycaemic clamp, thus illustrating the failure of alpha cell glucose sensing in diabetic subjects. Infusion of GLP-1 during the hyperglycaemic clamp had a much larger suppressive effect on plasma glucagon in patients than in healthy volunteers. Similar findings were reported by Vilsbøll et al. [97]. In both of these hyperglycaemic clamp/GLP-1 infusion studies, the absolute glucagon levels observed in patients with type 2 diabetes were either equal to or lower than those observed in healthy individuals, once again suggesting that GLP-1 can improve glucose sensing by the alpha cell, or that GLP-1 ‘allows’ glucose to suppress glucagon release in diabetic patients.
Perhaps the clearest demonstration of the influence of GLP-1 on alpha cell function in diabetic patients was provided by a study in which arginine-stimulated glucagon responses were examined at basal glucose levels and during hyperglycaemic clamps at 14 and 28 mmol/l glucose. GLP-1 infusion significantly enhanced glucose-induced suppression of both prestimulus and arginine-stimulated glucagon levels at each glucose concentration (Fig. 7). As discussed above, an index of alpha cell sensitivity to glucose can be obtained from the glucose level at which half-maximal suppression (PG50) of glucagon levels (Fig. 7a) or response (Fig. 7b) occurs. The PG50 for prestimulus glucagon averaged 15.5±1.0 mmol/l when saline was infused and 11.0±0.8 mmol/l during GLP-1 infusion (p<0.001). Similarly, the PG50 for AGRarg was 15.5±0.7 mmol/l during saline and 12.1±0.8 mmol/l during GLP-1 (p<0.001). Such findings suggest that GLP-1 infusion shifts the glucose dose–response curve to the left, i.e. sensitizes the alpha cell to the suppressive effects of glucose [98]. It may be noted that the magnitude of the decrease in the PG50 for the AGRarg in response to GLP-1 to is very similar to the increase in this parameter estimated from mean data comparing patients with type 2 diabetes with healthy volunteers (cf. Fig. 3). Accordingly, it may be speculated that a GLP-1-based therapy may be capable of correcting the defect in alpha cell glucose sensing that is characteristic of type 2 diabetes.
Prestimulus plasma glucagon levels (a) and the acute glucagon response to intravenous arginine (AGRarg=mean level from 2–5 min) (b) during stepped hyperglycaemic clamps in patients with type 2 diabetes during infusion of saline (closed circles) or GLP-1 (open triangles). The data are presented as means±SEM, n=6. Adapted with permission from [98]
At present, only limited data are available with respect to the acute effects of GLP-1 agonists other than the native peptide on alpha cell function in diabetic patients. A recent study demonstrated that subcutaneous injection of exenatide decreased fasting plasma glucagon in patients with type 2 diabetes in a dose-related manner and eliminated meal-stimulated glucagon release [99]. In contrast, subcutaneous injection of the acylated derivative of GLP-1, liraglutide, did not affect fasting glucagon or glucagon during graded glucose infusions in patients with type 2 diabetes [4]. However, in another study, bedtime injection of liraglutide modestly decreased postmeal glucagon [100].
Text box 6
GLP-1 directly suppresses glucagon secretion in patients with type 2 diabetes, independently of any effects on insulin or gastric emptying. The glucagonostatic effect of GLP-1 is at least as pronounced in diabetes as in health, but the alpha cell response to incipient hypoglycaemia is not suppressed by GLP-1. GLP-1 appears to improve alpha cell function, although further studies are needed to establish if this peptide can normalise the defects in alpha cell glucose sensing that are characteristic of type 2 diabetes. |
Chronic effects of exogenous and endogenous GLP-1 in patients with type 2 diabetes
Zander and colleagues reported the first longer-term study of GLP-1 based therapy in patients with type 2 diabetes [101]. They found that a 6-week continuous subcutaneous infusion of GLP-1 did not affect fasting or 8-h mean plasma glucagon, as compared with saline infusion, but there was a tendency for glucagon to be lower after 1 and 6 weeks of treatment, and fasting and postmeal glucose were substantially reduced. The authors concluded from this that GLP-1 improved alpha cell sensitivity to prevailing glucose levels. In contrast, in a 3-month study in elderly patients switched from oral therapy to continuous GLP-1 infusion, as compared with those remaining on their previous oral therapy, found no effect of GLP-1 on glucagon, and the authors interpreted this as a loss of effect on glucagon with chronic treatment [102].
Another study explored the effects of 1 week of treatment with liraglutide on measures of alpha cell function in patients with type 2 diabetes. Liraglutide did not affect fasting glucagon, but decreased the 24-h glucagon AUC, which included three standardised meals, and the decrease following a protein-rich dinner was particularly large. Treatment with liraglutide reduced glucagon levels relative to placebo (by ∼17%) during a hyperglycaemic (15 mmol/l) clamp, and the glucagon AUC during an arginine stimulation test performed during the hyperglycaemic clamp was also reduced (by ∼16%) [103]. This outcome contrasts with some earlier negative results with acute administration of liraglutide (see above) and suggests that this GLP-1 derivative can affect alpha cell function during chronic treatment. Similarly, an 8-week study of once-daily injection of liraglutide in patients with type 2 diabetes reported that glucagon levels were reduced during meals, although no data were shown [104]. However, in a 12-week dose-ranging study of once-daily injection of liraglutide in patients with type 2 diabetes, no dose had a statistically significant effect on glucagon levels [105]. Taken together, the available information on liraglutide cannot as yet support firm conclusions regarding this compound and glucagon secretion, although it seems likely that, like GLP-1 and exenatide, liraglutide exerts glucagonostatic effects.
No glucagon data were reported in recent reports of a 4-week study of exenatide added to metformin or sulphonylurea treatment [106] or of a 30-week study of exenatide added to sulphonylurea treatment [107]. Earlier studies of a 48-h infusion of GLP-1 in patients during ongoing pioglitazone [108] or metformin [109] treatment did indicate a glucagon-lowering effect of the native peptide in combination with oral agents. Hence, it may be expected that GLP-1-based therapies will maintain their effectiveness when combined with existing oral agents.
As mentioned above, an alternative approach to enhancing the therapeutic effects of GLP-1 is to block the rapid degradation of endogenous GLP-1 by DPP-4 and thereby increase circulating levels of biologically active GLP-1. As with other small molecule DPP-4 inhibitors, vildagliptin has good oral availability; therefore, unlike the native peptide and peptide agonists, it does not require parenteral administration. Treatment with vildagliptin over 4 weeks in drug-naïve patients with type 2 diabetes increased circulating levels of intact GLP-1, and decreased plasma glucagon and glucose during a standardised meal challenge [110]. A similar effect of vildagliptin was recently reported in patients with type 1 diabetes [111], suggesting that the effect on the alpha cell did not require endogenous insulin.
Text box 7
The ability of GLP-1 agonists to suppress glucagon secretion in patients with type 2 diabetes appears to be maintained with chronic (up to 8 weeks) treatment. Treatment with a DPP-4 inhibitor over a 4-week period also reduced meal-stimulated glucagon levels. |
Future directions and therapeutic implications
Although much remains to be learned about GLP-1 and alpha cell function, current evidence suggests that GLP-1-based therapies will be effective at improving glycaemic control in patients with a broad range of metabolic disease, at least in part due to their ability to improve, perhaps even normalise, alpha cell function. The terminology in this area is evolving, and we suggest that the term ‘incretin mimetic’ is appropriately applied to GLP-1 agonists and derivatives such as exenatide and liraglutide, while the term ‘incretin enhancer’ may be useful to distinguish the mechanism of action of DPP-4 inhibitors such as vildagliptin from agents that act directly on target tissues.
Abbreviations
- AGRarg :
-
acute glucagon response to intravenous arginine bolus
- CCK:
-
cholecystokinin
- DPP-4:
-
dipeptidyl peptidase IV
- GIP:
-
glucose-dependent insulinotropic polypeptide
- GLP-1:
-
glucagon-like peptide-1
- PG50 :
-
plasma glucose level at which 50% of the maximal suppression of the AGRarg is observed
References
Unger RH, Orci L (1975) The essential role of glucagon in the pathogenesis of diabetes mellitus. Lancet 1:14–16
Gerich JE, Charles MA, Grodsky GM (1974) Characterization of the effects of arginine and glucose on glucagon and insulin release from the perfused rat pancreas. J Clin Invest 54:833–841
Mitrakou A, Ryan C, Veneman T et al (1991) Hierarchy of glycemic thresholds for counterregulatory hormone secretion, symptoms, and cerebral dysfunction. Am J Physiol 260:E67–E74
Chang AM, Jakobsen G, Sturis J et al (2003) The GLP-1 derivative NN2211 restores β-cell sensitivity to glucose in type 2 diabetic patients after a single dose. Diabetes 52:1786–1791
Rocha DM, Faloona GR, Unger RH (1972) Glucagon-stimulating activity of 20 amino acids in dogs. J Clin Invest 51:2346–2351
Larsson H, Ahrén B (2000) Islet dysfunction in insulin resistance involves impaired insulin secretion and increased glucagon secretion in postmenopausal women with impaired glucose tolerance. Diabetes Care 23:650–657
Ikeda T, Yoshida T, Ito Y et al (1987) Effect of β-hydroxybutyrate and acetoacetate on insulin and glucagon secretion from perfused rat pancreas. Arch Biochem Biophys 257:140–143
Gerich JE, Langlois M, Noacco C et al (1976) Comparison of the suppressive effects of elevated plasma glucose and free fatty acid levels on glucagon secretion in normal and insulin-dependent diabetic subjects. Evidence for selective alpha-cell insensitivity to glucose in diabetes mellitus. J Clin Invest 58:320–325
Ahrén B, Veith RC, Taborsky GJ Jr (1987) Sympathetic nerve stimulation versus pancreatic norepinephrine infusion in the dog: (1). Effects on basal release of insulin and glucagon. Endocrinology 121:323–331
Ahrén B, Taborsky GJ Jr (1986) The mechanism of vagal nerve stimulation of glucagon and insulin secretion in the dog. Endocrinology 118:1551–1557
Stagner JI, Samols E (1992) The vascular order of islet cellular perfusion in the human pancreas. Diabetes 41:93–97
Taborsky GJ Jr (1983) Evidence of a paracrine role for pancreatic somatostatin in vivo. Am J Physiol 245:E598–E603
Greenbaum CJ, Havel PJ, Taborsky GJ Jr, Klaff LJ (1991) Intra-islet insulin permits glucose to directly suppress pancreatic A cell function. J Clin Invest 88:767–773
McCulloch DK, Raghu PK, Koerker DJ, Palmer JP, Klaff LJ (1989) Responses of the pancreatic A cell during hypoglycemia and hyperglycemia are dependent on the B cell. Metabolism 38:702–707
Havel PJ, Ahrén, B (1997) Activation of autonomic nerves and the adrenal medulla contributes to increased glucagon secretion during moderate insulin-induced hypoglycemia in women. Diabetes 46:801–807
Taborsky GJ, Ahrén B, Havel PJ (1998) Autonomic mediation of glucagon secretion during hypoglycemia: implications for impaired a-cell responses in type 1 diabetes. Diabetes 47:995–1005
Havel PJ, Parry SJ, Stern JS et al (1994) Redundant parasympathetic and sympathoadrenal mediation of increased glucagon secretion during insulin-induced hypoglycemia in conscious rats. Metabolism 43:860–866
Müller WA, Faloona GR, Aguilar-Parada E, Unger RH (1970) Abnormal alpha-cell function in diabetes. Response to carbohydrate and protein ingestion. N Engl J Med 283:109– 115
Baum D, Porte D Jr, Ensinck J (1979) Hyperglucagonemia and alpha-adrenergic receptor in acute hypoxia. Am J Physiol 237:E404–E408
Moller N, Beckwith R, Butler PC et al (1989) Metabolic and hormonal responses to exogenous hyperthermia in man. Clin Endocrinol (Oxf) 30:651–660
Yalow RS, Berson SA (1960) Immunoassay of endogenous plasma insulin in man. J Clin Invest 39:1157–1175
Unger RH, Eisentraut AM, McCall MS, Madison LL (1961) Glucagon antibodies and an immunoassay for glucagon. J Clin Invest 40:1280–1289
Faloona GR, Unger RH, (1974) Glucagon. In: Jaffe BM, Behrman HR (eds) Methods of hormone radioimmunoassay, pp 317–330 Academic, New York
Ahrén B, Lundquist I (1982) Glucagon immunoreactivity in plasma from normal and dystrophic mice. Diabetologia 22:258–263
Hollander PM, Asplin CM, Palmer JP (1982) Glucose modulation of insulin and glucagon secretion in nondiabetic and diabetic man. Diabetes 31:489–495
Beard JC, Ward WK, Halter JB, Wallum BJ, Porte D Jr (1987) Relationship of islet function to insulin action in human obesity. J Clin Endocrinol Metab 65:59–64
Palmer JP, Halter J, Werner PL (1979) Differential effect of isoproterenol on acute glucagon and insulin release in man. Metabolism 28:237–240
Chideckel EW, Palmer J, Koerker DJ et al (1975) Somatostatin blockade of acute and chronic stimuli of the endocrine pancreas and the consequences of this blockade on glucose homeostasis. J Clin Invest 55:754–762
Ward WK, Bolgiano DC, McKnight B, Halter JB, Porte D Jr (1984) Diminished B cell secretory capacity in patients with noninsulin-dependent diabetes mellitus. J Clin Invest 74:1318–1328
Gerich JE, Tsalikian E, Lorenzi M et al (1975) Normalization of fasting hyperglucagonemia and excessive glucagon responses to intravenous arginine in human diabetes mellitus by prolonged infusion of insulin. J Clin Endocrinol Metab 41:1178–1180
Baron AD, Schaeffer L, Shragg P, Kolterman OG (1987) Role of hyperglucagonemia in maintenance of increased rates of hepatic glucose output in type II diabetics. Diabetes 36:274–283
Gastaldelli A, Baldi S, Pettiti M et al (2000) Influence of obesity and type 2 diabetes on gluconeogenesis and glucose output in humans: a quantitative study. Diabetes 49:1367–1373
Aronoff SL, Bennett PH, Unger RH (1977) Immunoreactive glucagon (IRG) responses to intravenous glucose in prediabetes and diabetes among Pima Indians and normal Caucasians. J Clin Endocrinol Metab 44:968–972
Ohneda A, Watanabe K, Horigome K et al (1978) Abnormal response of pancreatic glucagon to glycemic changes in diabetes mellitus. J Clin Endocrinol Metab 46:504–510
Hamaguchi T, Fukushima H, Uehara M et al (1991) Abnormal glucagon response to arginine and its normalization in obese hyperinsulinaemic patients with glucose intolerance: importance of insulin action on pancreatic alpha cells. Diabetologia 34:801–806
Unger RH, Aguilar-Parada E, Müller WA, Eisentraut AM (1970) Studies of pancreatic alpha cell function in normal and diabetic subjects. J Clin Invest 49:837–848
Gerich JE, Langlois M, Noacco C, Karam JH, Forsham PH (1973) Lack of glucagon response to hypoglycemia in diabetes: evidence for an intrinsic pancreatic alpha cell defect. Science 182:171–173
Cryer PE, Davis SN, Shamoon H (2003) Hypoglycemia in diabetes. Diabetes Care 26:1902–1912
Heller SR, Macdonald IA, Tattersall RB (1987) Counterregulation in type 2 (non-insulin-dependent) diabetes mellitus. Normal endocrine and glycaemic responses, up to ten years after diagnosis. Diabetologia 30:924–929
Bolli GB, Tsalikian E, Haymond MW, Cryer PE, Gerich JE (1984) Defective glucose counterregulation after subcutaneous insulin in noninsulin-dependent diabetes mellitus: paradoxical suppression of glucose utilization and lack of compensatory increase in glucose production, roles of insulin resistance, abnormal neuroendocrine responses, and islet paracrine interactions. J Clin Invest 73:1532–1541
Gerich JE, Lorenzi M, Bier DM et al (1975) Prevention of human diabetic ketoacidosis by somatostatin. Evidence for an essential role of glucagon. N Engl J Med 292:985–989
Dinneen SF (2000) The postprandial state: mechanisms of glucose intolerance. Diabet Med 14 (Suppl 3):S19–S24
Mitrakou A, Kelley D, Mokan M et al (1992) Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance. N Engl J Med 326:22–29
Ahrén B, Larsson H (2001) Impaired glucose tolerance (IGT) is associated with reduced insulin-induced suppression of glucagon concentrations. Diabetologia 44:1998–2003
Larsson H, Ahrén B (2000) Glucose intolerance is predicted by low insulin secretion and high glucagon secretion: outcome of a prospective study in postmenopausal Caucasian women. Diabetologia 43:194–202
Kreymann B, Williams G, Ghatei MA, Bloom SR (1987) Glucagon-like peptide-1 7–36: a physiological incretin in man. Lancet 2:1300–1304
Kieffer TJ, Habener JF (1999) The glucagon-like peptides. Endocr Rev 20:876–913
Mojsov S, Weir GC, Habener JF (1987) Insulinotropin: glucagon-like peptide I (7–37) co-encoded in the glucagon gene is a potent stimulator of insulin release in the perfused rat pancreas. J Clin Invest 79:616–619
Gutniak M, Ørskov C, Holst JJ, Ahrén B, Efendic S (1992) Antidiabetogenic effect of glucagon-like peptide-1 (7–36)amide in normal subjects and patients with diabetes mellitus. N Engl J Med 326:1316–1322
Wettergren A, Schjoldager B, Mortensen PE et al (1993) Truncated GLP-1 (proglucagon 78–107-amide) inhibits gastric and pancreatic functions in man. Dig Dis Sci 38:665–673
Vilsbøll T, Holst JJ (2004) Incretins, insulin secretion and Type 2 diabetes mellitus. Diabetologia 47:357–366
Ahrén B, Schmitz O (2004) GLP-1 receptor agonists and DPP-4 inhibitors in the treatment of type 2 diabetes. Horm Metab Res 36:867–876
Deacon CF (2004) Therapeutic strategies based on glucagon-like Peptide 1. Diabetes 53:2181–2189
Ritzel R, Ørskov C, Holst JJ, Nauck MA (1995) Pharmacokinetic, insulinotropic, and glucagonostatic properties of GLP-1 [7–36 amide] after subcutaneous injection in healthy volunteers. Dose–response-relationships. Diabetologia 38:720–725
Moens K, Heimberg H, Flamez D et al (1996) Expression and functional activity of glucagon, glucagon-like peptide I, and glucose-dependent insulinotropic peptide receptors in rat pancreatic islet cells. Diabetes 45:257–261
Heller RS, Aponte GW (1995) Intra-islet regulation of hormone secretion by glucagon-like peptide-1-(7–36) amide. Am J Physiol 269:G852–G860
Ding WG, Renstrom E, Rorsman P, Buschard K, Gromada J (1997) Glucagon-like peptide I and glucose-dependent insulinotropic polypeptide stimulate Ca2+-induced secretion in rat alpha-cells by a protein kinase A-mediated mechanism. Diabetes 46:792–800
Komatsu R, Matsuyama T, Namba M et al (1989) Glucagonostatic and insulinotropic action of glucagonlike peptide I-(7–36)-amide. Diabetes 38:902–905
Suzuki S, Kawai K, Ohashi S, Mukai H, Yamashita K (1989) Comparison of the effects of various C-terminal and N-terminal fragment peptides of glucagon-like peptide-1 on insulin and glucagon release from the isolated perfused rat pancreas. Endocrinology 125:3109–3114
Kawai K, Suzuki S, Ohashi S et al (1989) Comparison of the effects of glucagon-like peptide-1-(1–37) and -(7–37) and glucagon on islet hormone release from isolated perfused canine and rat pancreases. Endocrinology 124:1768–1773
Guenifi A, Ahrén B, Abdel-Halim SM (2001) Differential effects of glucagon-like peptide-1 (7–36)amide versus cholecystokinin on arginine-induced islet hormone release in vivo and in vitro. Pancreas 22:58–64
Yamato E, Noma Y, Tahara Y et al (1990) Suppression of synthesis and release of glucagon by glucagon-like peptide-1 (7–36 amide) without affect on mRNA level in isolated rat islets. Biochem Biophys Res Commun 167:431–437
Ohneda A, Ohneda K, Ohneda M et al (1991) The structure–function relationship of GLP-1 related peptides in the endocrine function of the canine pancreas. Tohoku J Exp Med 165:209–221
Ørskov C, Holst JJ, Nielsen OV (1988) Effect of truncated glucagon-like peptide-1 [proglucagon-(78–107) amide] on endocrine secretion from pig pancreas, antrum, and nonantral stomach. Endocrinology 123:2009–2013
Fehmann HC, Hering BJ, Wolf MJ et al (1995) The effects of glucagon-like peptide-I (GLP-I) on hormone secretion from isolated human pancreatic islets. Pancreas 11:196–200
Matsumura T, Itoh H, Watanabe N et al (1992) Glucagonlike peptide-1(7–36)amide suppresses glucagon secretion and decreases cyclic AMP concentration in cultured In-R1-G9 cells. Biochem Biophys Res Commun 186:503–508
Matsuyama T, Komatsu R, Namba M et al (1988) Glucagon-like peptide-1 (7–36 amide): a potent glucagonostatic and insulinotropic hormone. Diabetes Res Clin Pract 5:281–284
Silvestre RA, Rodriguez-Gallardo J, Egido EM, Marco J (2003) Interrelationship among insulin, glucagon and somatostatin secretory responses to exendin-4 in the perfused rat pancreas. Eur J Pharmacol 469:195–200
Fridolf T, Bottcher G, Sundler F, Ahrén B (1991) GLP-1 and GLP-1(7–36) amide: influences on basal and stimulated insulin and glucagon secretion in the mouse. Pancreas 6:208–215
Van Dijk G, Lindskog S, Holst JJ, Steffens AB, Ahrén B (1996) Effects of glucagon-like peptide-I on glucose turnover in rats. Am J Physiol 270:E1015–E1021
Ribel U, Larsen MO, Rolin B et al (2002) NN2211: a long-acting glucagon-like peptide-1 derivative with anti-diabetic effects in glucose-intolerant pigs. Eur J Pharmacol 451:217–225
D’Alessio DA, Vogel R, Prigeon R et al (1996) Elimination of the action of glucagon-like peptide 1 causes an impairment of glucose tolerance after nutrient ingestion by healthy baboons. J Clin Invest 97:133–138
Pospisilik JA, Stafford SG, Demuth HU, McIntosh CH, Pederson RA (2002) Long-term treatment with dipeptidyl peptidase IV inhibitor improves hepatic and peripheral insulin sensitivity in the VDF Zucker rat: a euglycemic-hyperinsulinemic clamp study. Diabetes 51:2677–2683
Deacon CF, Wamberg S, Bie P, Hughes TE, Holst JJ (2002) Preservation of active incretin hormones by inhibition of dipeptidyl peptidase IV suppresses meal-induced incretin secretion in dogs. J Endocrinol 172:355–362
Bell GI, Sanchez-Pescador R, Laybourn PJ, Najarian RC (1983) Exon duplication and divergence in the human preproglucagon gene. Nature 304:368–371
Ryan AS, Egan JM, Habener JF, Elahi D (1998) Insulinotropic hormone glucagon-like peptide-1-(7–37) appears not to augment insulin-mediated glucose uptake in young men during euglycemia. J Clin Endocrinol Metab 83:2399–2404
Flint A, Raben A, Ersboll AK, Holst JJ, Astrup A (2001) The effect of physiological levels of glucagon-like peptide-1 on appetite, gastric emptying, energy and substrate metabolism in obesity. Int J Obes Relat Metab Disord 25:781–792
Flint A, Raben A, Rehfeld JF, Holst JJ, Astrup A (2000) The effect of glucagon-like peptide-1 on energy expenditure and substrate metabolism in humans. Int J Obes 24:288–298
Ahrén B, Holst JJ, Mari A (2003) Characterization of GLP-1 effects on β-cell function after meal ingestion in humans. Diabetes Care 26:2860–2864
Nauck MA, Niedereichholz U, Ettler R et al (1997) Glucagon-like peptide 1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am J Physiol Endocrinol Metab 273:E981–E988
Vahl TP, Paty BW, Fuller BD, Prigeon RL, D’Alessio DA (2003) Effects of GLP-1-(7–36)NH2, GLP-1-(7–37), and GLP-1- (9–36)NH2 on intravenous glucose tolerance and glucose-induced insulin secretion in healthy humans. J Clin Endocrinol Metab 88:1772–1779
Vilsbøll T, Krarup T, Madsbad S, Holst JJ (2003) Both GLP-1 and GIP are insulinotropic at basal and postprandial glucose levels and contribute nearly equally to the incretin effect of a meal in healthy subjects. Regul Pept 114:115–121
Degn KB, Brock B, Juhl CB et al (2004) Effect of intravenous infusion of exenatide (synthetic exendin-4) on glucose-dependent insulin secretion and counterregulation during hypoglycemia. Diabetes 53:2397–2403
Nauck MA, Heimesaat MM, Behle K et al (2002) Effects of glucagon-like peptide 1 on counterregulatory hormone responses, cognitive functions, and insulin secretion during hyperinsulinemic, stepped hypoglycemic clamp experiments in healthy volunteers. J Clin Endocrinol Metab 87:1239–1246
Schirra J, Sturm K, Leicht P et al (1998) Exendin(9–39)amide is an antagonist of glucagon-like peptide-1(7–36)amide in humans. J Clin Invest 101:1421–1430
Gutniak MK, Linde B, Holst JJ, Efendic S (1994) Subcutaneous injection of the incretin hormone glucagon-like peptide 1 abolishes postprandial glycemia in NIDDM. Diabetes Care 17:1039–1044
Todd JF, Wilding JPH, Edwards CMB et al (1997) Glucagon-like peptide-1 (GLP-1): a trial of treatment in non-insulin-dependent diabetes mellitus. Eur J Clin Invest 27:533–536
Gutniak MK, Larsson H, Sanders SW et al (1997) GLP-1 tablet in type 2 diabetes in fasting and postprandial conditions. Diabetes Care 20:1874–1879
Gutniak MK, Svartberg J, Hellstrom PM et al (2001) Antidiabetogenic action of glucagon-like peptide-1 related to administration relative to meal intake in subjects with type 2 diabetes. J Intern Med 250:81–87
Willms B, Werner J, Holst JJ et al (1996) Gastric emptying, glucose responses, and insulin secretion after a liquid test meal: effects of exogenous glucagon-like peptide-1 (GLP-1)-(7–36) amide in type 2 (noninsulin-dependent) diabetic patients. J Clin Endocrinol Metab 81:327–332
Meier JJ, Gallwitz B, Salmen S et al (2003) Normalization of glucose concentrations and deceleration of gastric emptying after solid meals during intravenous glucagon-like peptide 1 in patients with type 2 diabetes. J Clin Endocrinol Metab 88:2719–2725
Behme MT, Dupre J, McDonald TJ (2003) Glucagon-like peptide 1 improved glycemic control in type 1 diabetes. BMC Endocrine Disorders 3:3
Nauck MA, Kleine N, Ørskov C et al (1993) Normalization of fasting hyperglycaemia by exogenous glucagon-like peptide 1 (7–36 amide) in type 2 (non-insulin-dependent) diabetic patients. Diabetologia 36:741–744
Creutzfeldt WOC, Kleine N, Willms B et al (1996) Glucagonostatic actions and reduction of fasting hyperglycemia by exogenous glucagon-like peptide I(7–36) amide in type I diabetic patients. Diabetes Care 19:580–586
Nauck MA, Sauerwald A, Ritzel R, Holst JJ, Schmiegel W (1998) Influence of glucagon-like peptide 1 on fasting glycemia in type 2 diabetic patients treated with insulin after sulfonylurea secondary failure. Diabetes Care 21:1925–1931
Nauck MA, Heimesaat MM, Ørskov C et al (1993) Preserved incretin activity of glucagon-like peptide 1 [7–36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest 91:301–307
Vilsbøll T, Krarup T, Madsbad S, Holst JJ (2002) Defective amplification of the late phase insulin response to glucose by GIP in obese Type II diabetic patients. Diabetologia 45:1111–1119
Ahrén B, Larsson H, Holst JJ (1997) Effects of glucagon-like peptide-1 on islet function and insulin sensitivity in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 82:473–478
Kolterman OG, Buse JB, Fineman MS et al (2003) Synthetic exendin-4 (exenatide) significantly reduces postprandial and fasting plasma glucose in subjects with type 2 diabetes. J Clin Endocrinol Metab 88:3082–3089
Juhl CB, Hollingdal M, Sturis J et al (2002) Bedtime administration of NN2211, a long-acting GLP-1 derivative, substantially reduces fasting and postprandial glycemia in type 2 diabetes. Diabetes 51:424–429
Zander M, Madsbad S, Madsen JL, Holst JJ (2002) Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and β-cell function in type 2 diabetes: a parallel-group study. Lancet 359:824–830
Meneilly GS, Greig N, Tildesley H et al (2003) Effects of 3 months of continuous subcutaneous administration of glucagon-like peptide 1 in elderly patients with type 2 diabetes. Diabetes Care 26:2835–2841
Degn KB, Juhl CB, Sturis J et al (2004) One week’s treatment with the long-acting glucagon-like peptide 1 derivative liraglutide (NN2211) markedly improves 24-h glycemia and α- and β-cell function and reduces endogenous glucose release in patients with type 2 diabetes. Diabetes 53:1187–1194
Harder H, Nielsen L, Thi TD, Astrup A (2004) The effect of liraglutide, a long-acting glucagon-like peptide 1 derivative, on glycemic control, body composition, and 24-h energy expenditure in patients with type 2 diabetes. Diabetes Care 27:1915–1921
Madsbad S, Schmitz O, Ranstam J, Jakobsen G, Matthews DR (2004) Improved glycemic control with no weight increase in patients with type 2 diabetes after once-daily treatment with the long-acting glucagon-like peptide 1 analog liraglutide (NN2211): a 12-week, double-blind, randomized, controlled trial. Diabetes Care 27:1335–1342
Fineman MS, Bicsak TA, Shen LZ et al (2003) Effect on glycemic control of exenatide (synthetic exendin-4) additive to existing metformin and/or sulfonylurea treatment in patients with type 2 diabetes. Diabetes Care 26:2370–2377
Buse JB, Henry RR, Han J et al (2004) Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes. Diabetes Care 27:2628–2635
Zander M, Christiansen A, Madsbad S, Holst JJ (2004) Additive effects of glucagon-like peptide 1 and pioglitazone in patients with type 2 diabetes. Diabetes Care 27:1910–1914
Zander M, Taskiran M, Toft-Nielsen MB, Madsbad S, Holst JJ (2001) Additive glucose-lowering effects of glucagon-like peptide-1 and metformin in type 2 diabetes. Diabetes Care 24:720–725
Ahrén B, Landin-Olsson M, Jansson PA et al (2004) Inhibition of dipeptidyl peptidase-4 reduces glycemia, sustains insulin levels and reduces glucagon levels in type 2 diabetes. J Clin Endocrinol Metab 89:2078–2084
Jones-Leone AR, Yu T, Barilla D, He YL, Ho Y, Ligueros-Saylan M, Foley J, Kelley DE (2004) Evidence for insulin independent suppression of glucagon secretion by LAF237. Diabetologia 47(suppl 1):A289. 2004. Ref Type: Abstract
Gerich JE, Karam JH, Forsham PH (1973) Stimulation of glucagon secretion by epinephrine in man. J Clin Endocrinol Metab 37:479–481
DeFronzo RA, Binder C, Wahren J et al (1981) Sensitivity of insulin secretion to feedback inhibition by hyperinsulinaemia. Acta Endocrinologica (Copenh) 98:81–86
Paolisso G, Pizza G, De Riu S et al (1990) Effects of oxytocin upon the endocrine pancreas secretion and glucose turnover in normal man. Acta Endocrinologica (Copenh) 123:504–510
Ward FR, Leblanc H, Yen SS (1975) The inhibitory effect of somatostatin on growth hormone, insulin and glucagon secretion in diabetes mellitus. J Clin Endocrinol Metab 41:527–532
Dunning BE, Moltz JH, Fawcett CP (1984) Actions of neurohypophysial peptides on pancreatic hormone release. Am J Physiol 246:E108–E114
Santeusanio F, Faloona GR, Unger RH (1972) Suppressive effect of secretin upon pancreatic alpha cell function. J Clin Invest 51:1743–1749
Meier JJ, Gallwitz B, Siepmann N et al (2003) Gastric inhibitory polypeptide (GIP) dose-dependently stimulates glucagon secretion in healthy human subjects at euglycaemia. Diabetologia 46:798–801
Filipsson K, Tornoe K, Holst J, Ahrén B (1997) Pituitary adenylate cyclase-activating polypeptide stimulates insulin and glucagon secretion in humans. J Clin Endocrinol Metab 82:3093–3098
Knigge U, Holst JJ, Knuhtsen S et al (1984) Gastrin-releasing peptide: pharmacokinetics and effects on gastro-entero-pancreatic hormones and gastric secretion in normal men. J Clin Endocrinol Metab 59:310–315
Rushakoff RJ, Goldfine ID, Carter JD, Liddle RA (1987) Physiological concentrations of cholecystokinin stimulate amino acid-induced insulin release in humans. J Clin Endocrinol Metab 65:395–401
Fahrenkrug J, Pedersen JH, Yamashita Y et al (1987) Occurrence of VIP and peptide HM in human pancreas and their influence on pancreatic endocrine secretion in man. Regul Pept 18:51–61
Acknowledgements
The authors gratefully acknowledge the Swedish Medical Research Council (grant number 6834); the Swedish Diabetes Association; the Faculty of Medicine, Lund University; and the Region of Skåne for their interest and support.
Duality of interest.
B. Ahrén has served as a consultant for Novo Nordisk and Novartis. J. E. Foley is employed by Novartis Pharmaceuticals Corporation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dunning, B.E., Foley, J.E. & Ahrén, B. Alpha cell function in health and disease: influence of glucagon-like peptide-1. Diabetologia 48, 1700–1713 (2005). https://doi.org/10.1007/s00125-005-1878-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1878-0