Abstract
Aims/hypothesis
The accumulation of AGE is related to the progression of the renal, retinal and vascular complications of diabetes. However, the relationship with diabetic neuropathy remains unclear. We recently showed that skin autofluorescence, measured non-invasively with an AutoFluorescence Reader (AFR), could be used to assess skin AGE accumulation. We evaluated the relationship between skin autofluorescence and the severity of diabetic neuropathy.
Materials and methods
Skin autofluorescence in arbitrary units (AU) was assessed in 24 diabetic patients with a history of neuropathic foot ulceration (NP+), 23 diabetic patients without clinical neuropathy (NP−) and 21 control subjects, using the AFR. Arterial occlusive disease was excluded in all. The severity of foot ulceration was assessed by the Wagner score. Peripheral nerve function was assessed by neurography, measuring motor and sensory nerve conduction velocity and amplitude of the median, peroneal and sural nerves. Heart rate variability (HRV) and baroreflex sensitivity (BRS) were measured by Finapres to assess autonomic nervous function.
Results
Autofluorescence was increased in NP− compared with control subjects. In NP+ patients, autofluorescence was further increased and correlated with the Wagner score. Autofluorescence correlated negatively with nerve conduction velocity and amplitude, HRV and BRS in both NP+ and NP− groups. Autofluorescence correlated with age, diabetes duration, mean HbA1c of the previous year, serum creatinine level, presence of microalbuminuria and severity of diabetic retinopathy.
Conclusions/interpretation
Skin autofluorescence correlates with the severity of peripheral and autonomic nerve abnormalities in diabetes, even before being clinically manifest. The AFR may be a convenient and rapid clinical tool for assessing risk of progression of long-term diabetic complications.
Similar content being viewed by others
Introduction
Peripheral sensorimotor neuropathy and autonomic neuropathy are the most frequent manifestations of diabetic neuropathy and both are independent predictors of foot ulceration, lower extremity amputation and mortality [1–4]. Several risk factors for the development of diabetic neuropathy have been identified (e.g. glycaemic status, microalbuminuria), but recent evidence has drawn attention to the accumulation of AGE [5–8].
Glycation of proteins is a series of complex and sequential reactions, collectively called the Maillard reaction, that occur in all tissues and body fluids. Early-stage reactions lead to the formation of the early glycation adducts (e.g. fructosyl–lysine) and later-stage reactions form AGE. Fructosyl–lysine slowly degrades to form AGE. Glyoxal, methylglyoxal and 3-deoxyglucosone are also potent glycating agents formed by the degradation of glycolytic intermediates, glycated proteins and lipid peroxidation. They react with proteins to form AGE [9–12]. Accumulation of chemically stable AGE adducts on long-lived proteins reflects the cumulative effects of oxidative stress and hyperglycaemia, and both are strongly related to the development of diabetic neuropathy. In a substudy of the Diabetes Control and Complications Trial (DCCT), skin AGE levels explained a major part of the variance in diabetic complications, even after adjustment for HbA1c [13]. Prevention of AGE accumulation, in predominantly experimental or animal studies, reduced the development of a wide range of diabetic complications, including nerve dysfunction [14–17]. However, little clinical evidence is available on the relationship between AGE accumulation and diabetic neuropathy. Tissue AGE assays are invasive and expensive, and have not reached the clinic. Analysis of AGE in blood proteins, total serum or plasma does not necessarily reflect tissue AGE concentrations [17].
Recently, we described a non-invasive technique for measuring skin autofluorescence using an Autofluorescence Reader (AFR) [18]. Skin autofluorescence measured with the AFR was correlated strongly with collagen-linked fluorescence and tissue accumulation of the AGE pentosidine, carboxymethyl-lysine (CML) and carboxyethyl-lysine (CEL) in diabetic patients and healthy subjects [19]. If skin autofluorescence reflects tissue AGE accumulation, the AFR may be a convenient tool for assessment of the risk of AGE-related complications. The cross-sectional study described below was designed to test the hypothesis that skin autofluorescence, an indirect measure of skin AGE accumulation, correlates with the severity of both peripheral and autonomic neuropathy in diabetic patients.
Subjects and methods
Subjects
Twenty-four diabetic patients with a history of foot neuropathic ulceration, 23 diabetic patients without clinical neuropathy and 21 control subjects were studied. Exclusion criteria were factors that may interfere with nerve function, such as peripheral vascular disease (ankle–arm indices <0.90, toe–arm indices <0.70), electrocardiographic abnormalities, and use of β-blockers or calcium antagonists. Both type 1 (age at diagnosis of diabetes <30 years and insulin-dependent from onset) and type 2 diabetic patients were recruited randomly from our diabetes outpatient clinic. In control subjects, diabetes mellitus and renal failure were excluded by the respective conventional American Diabetes Association criteria and (for renal failure) a serum creatinine of <120 μmol/l.
The presence or absence of clinical neuropathy in diabetic patients was defined using the Dutch Diabetic Neuropathy Symptoms (DNS) scale, the Dutch Diabetic Neuropathy Examination (DNE) scale, and quantitative sensory function testing with Semmes–Weinstein monofilaments. In the group of diabetic patients without neuropathy, DNS and DNE scores (see below) had to be 0 points and ≤3 points, respectively, with the 10-g Semmes–Weinstein monofilament felt on all occasions. In the patients with foot ulcers and definite neuropathy, the DNS and DNE scores were ≥1 point and ≥4 points, respectively, while the 10-g Semmes–Weinstein filament was not felt on all occasions. In diabetic patients, data collected from chart reviews included known duration of diabetes mellitus, mean HbA1c during the previous year, blood pressure and presence of microalbuminuria. Microalbuminuria was defined as a urinary albumin excretion rate between 20 and 200 μg/min in at least two out of three overnight urine collections in the preceding year. Clinical characteristics of the subjects are given in Table 1.
Autofluorescence measurements, nerve conduction studies, heart rate variability and baroreflex sensitivity were measured in all subjects. Wagner scores were used to quantify the severity of ulcers in diabetic patients with foot ulcers. The participants were studied in the morning, 1.5 h after breakfast, during which the diabetic patients had taken their oral hypoglycaemic drugs or regular insulin injections. Subjects were instructed not to smoke or consume caffeine drinks 24 h before the study. The local ethics committee approved this study and informed consent was obtained prior to the measurements in all subjects.
Skin autofluorescence
Skin autofluorescence was assessed by the AFR (patent PCT/NL99/00607; prototype of current AGE Reader I, Diagnoptics BV, Groningen, The Netherlands). In short, the AFR illuminates a skin surface of 1 cm2, guarded against surrounding light, with an excitation light source between 300 and 420 nm (peak excitation ∼350 nm). Only light from the skin is measured with the spectrometer (Ocean Optics PC-1000 fiber optic spectrometer; Ocean Optics, Dunedin, FL, USA) in the 300–600 nm range, using 200-μm glass fibre (Farnell, Leeds UK). The measure of autofluorescence was defined as the average light intensity per nm in the range between 420 and 600 nm, divided by the average light intensity per nanometer in the range between 300 and 420 nm (autofluorescence).
Skin reflection measurements in the 300–420-nm range were analysed by comparing them with those of a white Teflon block (assuming 100% reflectance), i.e. the mean intensity reflected from the skin divided by the mean intensity reflected from the white Teflon block in the range 300–420 nm. This correction corrects for effects of skin pigmentation and redness, which may influence autofluorescence by light absorption [20, 21].
All measurements were performed at room temperature in a dark environment. After control measurements with the lamp off (dark), autofluorescence of the skin was measured six times (every 10 s) at the volar side of the arm approximately 10 cm below the elbow fold. Care was taken to perform the measurement at a normal skin site, thus without visible vessels, scars, lichenification or other skin abnormalities.
AFR measurements on 1 day and intra-individual seasonal variance showed an Altman error percentage of <6%. The differences between repeated measurements did not alter depending on autofluorescence level. The autofluorescence ratio is calculated offline by automated analysis and is observer independent.
Diabetic neuropathy
The DNS and DNE scales have been described in detail previously [22]. The DNS scale is a 12-item validated-symptom scale modified from earlier neuropathy scores [23], with a high predictive value to screen for distal polyneuropathy and autonomic neuropathy in diabetes. Symptoms of unsteadiness in walking, neuropathic pain, paraesthesia, dizziness and numbness are elicited, and the presence of a symptom is scored as one point.
The DNE scale is a sensitive and validated hierarchical scoring system for diabetic neuropathy. The score includes measures of muscle strength, reflexes and sensation, with a total of eight items, scoring normal, moderate deficit or severely disturbed per item.
Semmes–Weinstein 10-g monofilaments and Vibration Perception Threshold (VPT) using a handheld biothesiometer (Biomedical Instruments, OH, USA) were used as quantitative sensory tests [24, 25]. Deficits in sensing were measured using a 10-g 5.07 Semmes–Weinstein monofilament applied to eight areas on the dorsal foot skin; deficits in one or more skin areas was defined as impaired sensing. If at VPT the voltage needed for vibration had to be increased to such a level that the mean of three readings at the first toe was above 25 V, the response was defined as certainly defective, and if the mean was between 16 and 24 V it was denoted as intermediately impaired vibration perception.
Nerve conduction studies were performed with standard surface stimulation and recording techniques using an electromyograph (Nicolet Viking IIe and IV) with standard filter settings. All measurements were performed after warming of forearm and lower leg in hot (38°C) water for at least 15 min. Motor nerve conduction velocity was measured on the left forearm segments of the median nerve and the left peroneal nerve. Sensory nerve conduction velocity was measured antidromically with ring electrodes placed around digit 3 (median nerve) and stimulation at the wrist. The sural nerve was tested antidromically after lateral stimulation of the Achilles tendon (sural nerve), 10–12 cm proximal from the active electrode. Peak–peak amplitude values were used.
Heart rate variability was measured in accordance with the guidelines of the Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology [26]. ECG signals were sampled at 100 Hz and stored, and analysed offline by using the CARSPAN program as described previously [27]. After artefact correction and stationary check, discrete Fourier transformation of the RR interval (ms) was performed. To assess baroreflex sensitivity (BRS), blood pressure and heart rate were measured beat to beat by Finapres. BRS was determined by the transfer function method using the CARSPAN program, as previously described in detail [28].
Statistical analyses
Differences in autofluorescence between the three studied groups were analysed using ANOVA with post hoc Bonferroni correction. For HRV and BRS, a logarithmic transformation was used to obtain normal distribution for further analysis. In the case of normal distribution of variables, Pearson’s correlation was assessed, in the case of non-normal distribution or of categorical values Spearman’s correlation was assessed. Multivariable stepwise regression analyses were performed for determination of independent effects. A two-tailed p value <0.05 was considered significant. Data are shown as means±SD.
Results
Skin autofluorescence in general
Autofluorescence was increased in diabetic patients without clinical neuropathy compared with control subjects (respectively, 0.017±0.004 arbitrary units [AU] vs 0.011±0.001 AU, p<0.01) and further increased in diabetic patients with neuropathic foot ulcers (0.025±0.007 AU, p<0.001). In diabetic patients, autofluorescence correlated with age (r=0.46, p<0.01), diabetes duration (r=0.47, p<0.01), mean HbA1c of the previous year (r=0.61, p<0.01), serum creatinine level (r=0.50, p<0.01), the severity of diabetic retinopathy (r=0.42, p<0.01) and urinary albumin excretion (r=0.37, p<0.01). No correlations were observed between autofluorescence and specific medical treatment, insulin dosage, body mass index, sex or smoking habits. Approximately 60% of the variance in autofluorescence could be explained by the independent effects of age (p=0.03), mean HbA1c of the previous year (p=0.01) and the presence of microalbuminuria (p=0.001) in diabetic patients (overall r=0.77, p<0.001). In control subjects, autofluorescence correlated with age (r=0.53, p=0.01) and smoking habits (p<0.01).
Skin autofluorescence and neuropathy
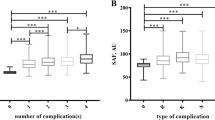
Table 2 describes the analysis of diabetic neuropathy parameters in our study populations. Autofluorescence correlated with the DNS (r=0.34, p=0.02) and DNE scale (r=0.50, p=0.001). Table 3 shows the correlations for autofluorescence with nerve conduction velocity and amplitude of the median, peroneal and sural nerve in both diabetic groups and control subjects. Autofluorescence correlated negatively with both sensory and motor nerve conduction velocities and amplitude in both diabetic groups. In control subjects, autofluorescence showed a negative trend with nerve conduction velocity. Figure 1 shows the relationship between autofluorescence and sensory nerve conduction velocity of the median nerve.
Nerve conduction velocity and amplitude further correlated with age (r=−0.4, p=0.03), mean HbA1c of the previous year (r=−0.5, p<0.01), diabetes duration (r=−0.36, p=0.02), serum creatinine level (r=−0.4, p=0.04) and presence of microalbuminuria (p=0.02). Stepwise multivariate analysis showed that autofluorescence independently explained 55% of the variance in nerve conduction velocity and amplitude (r=0.74, p<0.01).
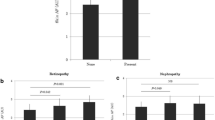
Autofluorescence correlated negatively with heart rate variability (HRV; r=−0.61, p<0.01; Fig. 2) and with baroreflex sensitivity (BRS; r=−0.63, p<0.01) in the group of diabetic patients, but not in control subjects. Both HRV and BRS also correlated with age (r=−0.57, p<0.01), mean HbA1c (r=−0.41, p<0.01), diabetes duration (r=−0.33, p=0.03), serum creatinine level (r=−0.39, p<0.01), systolic blood pressure (r=−0.44, p<0.01) and the presence of microalbuminuria (p<0.01). Approximately 50% of the variance in heart rate variability and baroreflex sensitivity could be explained by the independent effects of autofluorescence and the presence of microalbuminuria in diabetic patients (overall r=0.68, p<0.01). There was no, or only weak, correlation (r<0.2) of BRS and HRV with nerve conduction velocity or amplitude.
In diabetic patients with neuropathic foot ulcers, the Wagner score correlated with autofluorescence (r=0.64, p<0.01), mean HbA1c of the previous year (r=0.45, p=0.03), systolic blood pressure although not significantly (r=0.42, p=0.06), presence of microalbuminuria (p=0.01), BRS (r=−0.46, p=0.04), sensory nerve conduction velocity and amplitude (r=−0.61, p=0.01) and serum creatinine level (r=0.50, p=0.01). Autofluorescence was related independently to the Wagner score, and Fig. 2 shows autofluorescence for diabetic patients with higher vs lower Wagner scores. The stepwise multivariate analysis showed that autofluorescence explained independently approximately 50% of the variance in the Wagner score (r=0.69, p<0.01).
Over half of the diabetic patients with neuropathy had microalbuminuria. The multivariate analysis showed that the presence of microalbuminuria was related strongly to nerve dysfunction. Importantly, the above-mentioned correlations were, to a lesser extent, also observed in diabetic patients without microalbuminuria.
Discussion
Our study shows that skin autofluorescence is increased in diabetic patients in relation to the severity of diabetic neuropathy and foot ulceration. But even before clinical symptoms of diabetic neuropathy exist, skin autofluorescence is closely related to nerve conduction and to markers of autonomic nerve function. As skin autofluorescence reflects AGE accumulation [19], our study supports the idea that AGE accumulation is an important risk factor for neuropathy in diabetic patients. Skin autofluorescence reflects accumulation independently of other well-known risk factors for neuropathy such as age, hyperglycaemia and microalbuminuria.
The power of skin autofluorescence as the best indicator for risk factors related to diabetic neuropathy was illustrated in the multivariate analysis in comparison with risk factors like hyperglycaemia. As we have previously shown that increased skin autofluorescence reflects increased AGE accumulation, it may represent the cumulative effect of hyperglycaemia, oxidative stress and renal dysfunction. Furthermore, AGE accumulation may be increased due to exogenous sources, such as smoking [29, 30]—as shown in our control subjects—and nutrition [31]. Importantly, tissue AGE accumulation may represent the long-term effects of a final common pathway for various risk factors. Thus, based on the present work, skin autofluorescence may integrate these factors and be more informative than the actual levels of these risk factors in themselves.
AGE accumulation has been related to the development of diabetic neuropathy [32]. The peripheral nervous system and, to a lesser extent, the central nervous system have been shown to be vulnerable to AGE accumulation in diabetes [16, 33]. Both intensive metabolic control of diabetic patients [13] and treatment with aminoguanidine (AGE inhibitor) in diabetic rats decrease the accumulation of AGE and the progression of diabetic neuropathy; they also reduce abnormal nerve conduction [16, 34]. Interestingly, we found increased skin autofluorescence in parallel with reduced nerve conduction velocity and amplitude in diabetic patients without clinical manifestations of diabetic neuropathy (Fig. 2, Table 3). Nerve conduction abnormalities of both peripheral and central nerves have been shown in diabetic patients without clinical neuropathy [35], but not as of yet in relation to AGE accumulation. Even in our control subjects, skin autofluorescence was related to nerve conduction velocity (Fig. 2, Table 3).
The severity of diabetic foot ulceration was also related to skin autofluorescence in our study. Although the presence of peripheral macrovascular disease was an exclusion criterion in our study, a complex inter-relationship between neuropathy and microvascular disease exists in diabetic patients. Microvascular disease may worsen ulceration, and endothelial dysfunction has been demonstrated in relation to both diabetic neuropathy and foot ulceration [36, 37]. AGE accumulation has also been reported to worsen endothelial function, and endothelial RAGE has been proposed as the major key in such an interaction. Blockade of RAGE accelerates wound closure in diabetic mice and suppresses levels of cytokines such as tumour necrosis factor [38]. AGE activation of inflammatory cells and a chronic inflammatory state can be established by the ability of cytokines to secrete proteases in excess of their inhibitors [39]. Therefore AGE accumulation may play a role in diabetic foot ulceration by its effects on neuropathy, on vascular disease and on delayed wound repair.
Our observation that skin autofluorescence increases in concert with autonomic dysfunction in diabetic patients has not been reported before. Different pathophysiological mechanisms in the development of autonomic and peripheral neuropathies have been suggested, as both types of neuropathy do not develop in concert in type 2 diabetic patients [40]. Importantly, HRV parameters in part normalise after intensive glycaemic control. We have also shown previously that the relationship between glycaemic status and autonomic function extends to the non-diabetic range, and suggested that, besides the glucose levels, oxidative stress might be involved in this correlation [41–44].
One limitation of the AFR is that not all AGE exhibit fluorescent properties. ELISA-based studies have shown increased accumulation of specific AGE before increased autofluorescence in diabetes [45]. Fluorescence represents group reactivity, which fails to provide quantitative information on concentrations of individual compounds. Importantly, the current understanding of physiological AGE indicates that the major AGE are not fluorescent cumulatively. However, our previous results in diabetic patients showed that skin autofluorescence may function as a marker of the AGE pool, based on the strong correlations with both fluorescent and non-fluorescent skin AGE levels [19]. Another limitation in our study is that we do not yet know the degree to which the relationship of autofluorescence with AGE accumulation is affected by other skin fluorophores, such as the oxidation degradation product of tryptophan, N-formylkynurenine, or elastin-linked fluorescence. In particular, advanced lipoxidation end-products (ALE) may also contribute to tissue and skin autofluorescence. The quantitative relationship between AGE and ALE in diabetes is still unknown, but dyslipidaemia may be as important as hyperglycaemia in chemical modification of proteins in diabetes [46]. Apparent changes in skin fluorescence as a consequence of light absorption by haemoglobin or NADH have been described [20]. Despite these theoretical limitations in AFR assays, skin biopsy fluorescence itself is strongly related to long-term diabetic complications [13].
Sunlight exposure as a source of skin photo-ageing might be considered as a confounding factor in skin AGE accumulation, but previous results with the AFR suggest that this effect is limited [19]. The present study was performed in Caucasian patients and controls, and, for the moment, our conclusions on the value of skin autofluorescence in diabetic neuropathy should be limited to non-pigmented skin.
The relevance of our non-invasive autofluorescence measurements in predicting progression of diabetic complications and mortality is now being investigated in a larger prospective study. Our results in diabetic patients with subclinical neuropathy show that the AGE accumulation as assessed by the AFR is associated with accepted early, preclinical markers of long-term complications, such as delayed nerve conduction velocity, and HRV and BRS abnormalities.
In conclusion, our results show that skin autofluorescence is increased during early stages of diabetic neuropathy and correlates with the severity of nerve dysfunction and foot ulceration. Assuming that autofluorescence reflects AGE accumulation, our study supports the important clinical impact of AGE accumulation in the pathogenesis of diabetic neuropathy. Long-term prospective studies must reveal the predictive value of AGE accumulation, or skin autofluorescence, in the progression of neuropathy and other diabetic complications.
Abbreviations
- AFR:
-
autofluorescence reader
- AU:
-
arbitrary units
- BRS:
-
baroreflex sensitivity
- DNS:
-
Dutch Diabetic Neuropathy Symptoms
- DNE:
-
Dutch Diabetic Neuropathy Examination
- HRV:
-
heart rate variability
- NCV/A:
-
nerve conduction velocity/amplitude
- NP+ :
-
patients with a history of neuropathic foot ulceration
- NP− :
-
patients without clinical neuropathy
- RAGE:
-
receptor for advanced glycation end-products
References
Holzer SE, Camerota A, Martens L, Cuerdon T, Crystal-Peters J, Zagari M (1998) Costs and duration of care for lower extremity ulcers in patients with diabetes. Clin Ther 20:169–181
Young MJ, Boulton AJM, McLeod AF, Williams DRR, Sonksen PH (1993) A multicentre study of the prevalence of diabetic neuropathy in the UK hospital clinical population. Diabetologia 36:150–154
Boulton AJM (1996) The pathogenesis of diabetic foot problems: an overview. Diabet Med 13:12–16
Ewing DJ, Campbell IW, Clarke BF (1976) Mortality in diabetic autonomic neuropathy. Lancet 1:601–603
Cameron NE, Eaton SE, Cotter MA, Tesfaye S (2001) Vascular factors and metabolic interactions in the pathogenesis of diabetic neuropathy. Diabetologia 44:1973–1988
Baynes JW (2002) Glycation and advanced glycation reaction. In: Gries FA, Cameron NE, Low PA, Ziegler D (eds) Diabetic neuropathy. Thieme Medical, Stuttgart
Obrosova IG (2003) Update on the pathogenesis of diabetic neuropathy. Curr Diab Rep 3:439–445
King RH (2001) The role of glycation in the pathogenesis of diabetic polyneuropathy. Mol Pathol 54:400–408
Schleicher E, Wagner E, Nerlich AG (1997) Increased accumulation of the glycoxidation product Ne-(carboxymethyl)lysine in human tissues in diabetes and aging. J Clin Invest 9:457–468
Makita Z, Radoff S, Rayfield EJ et al (1991) Advanced glycosylation end products in patients with diabetic nephropathy. N Engl J Med 325:836–842
Baynes JW, Thorpe SR (1999) Role of oxidative stress in diabetic complications. A new perspective on an old Paradigm. Diabetes 48:1–9
Nishikawa T, Edelstein D, Du XL et al (2000) Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 404:787–790
Monnier VM, Bautista O, DCCT Skin Collagen Ancillary Study Group (1999) Skin collagen glycation, glycoxidation, and crosslinking are lower in subjects with long-term intensive versus conventional therapy of type 1 diabetes. Diabetes 48:870–880
Nilsson BO (1999) Biological effects of aminoguanidine: an update. Inflamm Res 48:509–515
Stracke H, Lindemann A, Federlin K (1996) Benfotiamin–vitamin B combination in treatment of diabetic neuropathy. Exp Clin Endocrinol Diabetes 104:311–316
Cameron NE, Cotter MA, Dines K, Love A (1992) Effects of aminoguanidine on peripheral nerve function and polyol pathway metabolites in streptozotocin-diabetic rats. Diabetologia 35:946–950
Dorrian CA, Cathcart S, Clausen J, Shapiro D, Dominiczak MH (1998) Factors in human serum interfere with the measurement of advanced glycation endproducts. Cell Mol Biol 44:1069–1079
Meerwaldt R, Smit AJ, Navis GJ, van Roon AM, Graaff R, Gans ROB (2000) Increased skin autofluorescence in diabetes mellitus and renal failure. Diabetologia 44 [Suppl]:A1046
Meerwaldt R, Graaff R, Oomen PHN et al (2004) Simple noninvasive assessment of advanced glycation endproduct accumulation. Diabetologia 47:1324–1330
Coremans JMC, Ince C, Bruining HA, Puppels GJ (1997) (Semi-) quantitative analysis of reduced nicotinamide adenine dinucleotide fluorescence image of blood perfused rat heart. Biophys J 72:1849–1860
Na R, Stender IM, Henriksen M, Wulf HC (2001) Autofluorescence of human skin is age-related after correction for skin pigmentation and redness. J Invest Dermatol 116:536–540
Meijer JWG, van Sonderen E, Blaauwwiekel EE et al (2000) Diabetic neuropathy examination: a hierarchical scoring system to diagnose distal polyneuropathy in diabetes. Diabetes Care 23:750–753
Dyck PJ (1998) Detection, characterization and staging of polyneuropathy: assessed in diabetics. Muscle Nerve 11:21–32
Kumar S, Fernando DJS, Veves A, Knowles EA, Young MJ, Boulton AJM (1991) Semmes Weinstein monofilaments: a simple, effective and inexpensive screening device for identifying diabetic patients at risk of foot ulceration. Diabetes Res Clin Pract 13:63–68
Young MJ, Breddy JL, Veves A, Boulton AJM (1994) The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds. Diabetes Care 17:557–560
Task Force of the European Society of Cardiology and the Northern American Society of Pacing and Electrophysiology (1996) Heart rate variability. Standards of measurement, physiological interpretation and clinical use. Circulation 93:1043–1065
Lefrandt JD, Hoogenberg K, van Roon AM, Dullaart RPF, Gans ROB, Smit AJ (1999) Baroreflex sensitivity is depressed in microalbuminuric type 1 diabetic patients at rest and during sympathetic manoeuvres. Diabetologia 42:1345–1349
Robbe HW, Mulder LJ, Ruddel H, Langewitz WA, Veldman JB, Mulder G (1987) Assessment of baroreceptor reflex sensitivity by means of spectral analysis. Hypertension 10:538–543
Cerami C, Hounds H, Nicholl L et al (1997) Tobacco smoke is a source of toxic reactive glycation products. Proc Natl Acad Sci U S A 94:13915–13920
Nicoll ID, Stitt AW, Moore JE (1998) Increased levels of advanced glycation endproducts in the lenses and blood vessels of cigarette smokers. Mol Med 4:594–601
Koschinsky T, He CJ, Mitsuhashi T et al (1997) Orally absorbed reactive glycation products (glycotoxins): an environmental risk factor in diabetic nephropathy. Proc Natl Acad Sci U S A 94:6474–6479
Thornalley PJ (2002) Glycation in diabetic neuropathy: characteristics, consequences, causes, and therapeutic options. Int Rev Neurobiol 50:37–57
Cellek S, Qu W, Schmidt AM, Moncade S (2004) Synergistic action of advanced glycation end products and endogenous nitric oxide leads to neural apoptosis in vitro: a new insight into selective nitregic neuropathy in diabetes. Diabetologia 47:331–339
Tanaka Y, Uchino H, Shimizu T et al (1999) Effect of metformin on advanced glycation endproduct formation and peripheral nerve function in streptozotocin-induced diabetic rats. Eur J Pharmacol 376:17–22
Baba M, Ozaki I (2001) Electrophysiological changes in diabetic neuropathy: from subclinical alterations to disabling abnormalities. Arch Physiol Biochem 109:234–240
Veves A, Akbari CM, Primavera J et al (1998) Endothelial dysfunction and the expression of endothelial nitric oxide synthetase in diabetic neuropathy, vascular disease, and foot ulceration. Diabetes 47:457–463
Jude EB, Abbott CA, Young MJ, Anderson SG, Douglas JT, Boulton AJ (1999) The potential role of cell adhesion molecules in the pathogenesis of diabetic neuropathy. Diabetologia 41:330–336
Goova MT, Kislinger T, Qu W et al (2001) Blockade of receptor for advanced glycation end-products restores effective wound healing in diabetic mice. Am J Pathol 159:513–525
Pierce GF (2001) Inflammation in nonhealing diabetic wounds. Am J Pathol 159:399–403
Toyre JP, Partanen JV, Niskanen LK, Lansimies EA, Uusitupa MI (1997) Divergent development of autonomic and peripheral somatic neuropathies in NIDDM. Diabetologia 40:953–958
Burger AJ, Weinrauch LA, D’Elia JA, Aronson D (1999) Effect of glycemic control on heart rate variability in type 1 diabetic patients with cardiac autonomic neuropathy. Am J Cardiol 84:687–691
Lefrandt JD, Mulder MC, Bosma E, Smit AJ, Hoogenberg K (2001) Relation between autonomic function and blood glucose in the nondiabetic range. Diabetes Care 24:2017
Lefrandt JD, Mulder MC, Bosma E, Smit AJ, Hoogenberg K (2003) Inverse relationship between blood glucose and autonomic function in healthy subjects. Diabetes Care 23:1862–1864
Lefrandt JD, Diercks GF, van Boven AJ, Crijns HJ, van Gilst WH, Gans RO (2000) High fasting glucose and QTc duration in a large healthy cohort. Diabetologia 43:1332–1333
Beisswenger PJ, Makita Z, Curphey TJ et al (1995) Formation of immunochemical advanced glycosylation end products precede and correlate with early manifestations of renal and retinal disease in diabetes. Diabetes 44:824–829
Baynes JW, Thorpe SR (2000) Glycoxidation and lipoxidation in atherogenesis. Free Radic Biol Med 28:1708–1716
Acknowledgements
We would like to thank E. Bosma and J.H. van der Hoeven.
Duality of Interest:
R. Graaff and A. J. Smit are founders of Diagnoptics, The Netherlands, who manufacture the autofluorescence readers (http://www.diagnoptics.com).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meerwaldt, R., Links, T.P., Graaff, R. et al. Increased accumulation of skin advanced glycation end-products precedes and correlates with clinical manifestation of diabetic neuropathy. Diabetologia 48, 1637–1644 (2005). https://doi.org/10.1007/s00125-005-1828-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1828-x