Abstract
Aims/hypothesis
Morbid obesity (BMI>40 kg/m2) affecting 0.5–5% of the adult population worldwide is a major risk factor for type 2 diabetes. We aimed to elucidate the genetic bases of diabetes associated with obesity (diabesity), and to analyse the impact of corpulence on the effects of diabetes susceptibility genes.
Methods
We genotyped known single nucleotide polymorphisms (SNPs) in the adiponectin-encoding adipocyte C1q and collagen-domain-containing (ACDC) gene (−11,391G>A, −11,377C>G, +45T>G and +276G>T), the peroxisome proliferator-activated receptor gamma (PPARG) Pro12Ala SNP and ACDC exon 3 variants in 703 French morbidly obese subjects (BMI 47.6±7.4 kg/m2), 808 non-obese subjects (BMI<30 kg/m2) and 493 obese subjects (30≤BMI<40 kg/m2).
Results
Two 5′-ACDC SNPs −11,391G>A, −11,377C>G were associated with adiponectin levels (p=0.0003, p=0.008) and defined a ‘low-level’ haplotype associated with decreased adiponectin levels (p=0.0002) and insulin sensitivity (p=0.01) and with a risk of type 2 diabetes that was twice as high (p=0.002). In contrast, the prevalence of the PPARG Pro12Ala was identical in diabetic and normoglycaemic morbidly obese subjects. The PPARG Pro12 allele only displayed a trend of association with type 2 diabetes in the non-obese group. ACDC exon 3 variants were associated with type 2 diabetes in the non-obese group only (odds ratio 7.85, p<0.0001). In contrast, the 5′-ACDC ‘low-level’ haplotype was associated with type 2 diabetes in obese and morbidly obese subjects (odds ratio 1.73 and 1.92) but not in non-obese individuals.
Conclusions/interpretation
These data clarify the contribution of the 5′-ACDC SNPs to the risk of diabesity. Their interaction with corpulence suggests for the first time a different genetic profile of type 2 diabetes in morbidly obese patients compared with in less obese individuals.
Similar content being viewed by others
Introduction
Adiponectin is an adipokine encoded by the ACDC gene (adipocyte C1q and collagen-domain-containing, alternative names APM1, GBP28) involved in energy homeostasis. ACDC gene expression in adipocytes and serum adiponectin levels correlate with insulin sensitivity in humans [1–3]. In mouse models of insulin resistance, recombinant adiponectin attenuates type 2 diabetes [4]. Adiponectin, in contrast to TNF-α and leptin, is decreased in subjects with increased fat mass [3], type 2 diabetes or CHD [5]. Prospective studies in Caucasians and in the diabetes-susceptible Pima Indian population, showed that subjects with high adiponectin levels were protected against type 2 diabetes (odds ratio [OR] 0.63 in Pima Indians) [6, 7]. Heritability of adiponectin levels is 40–70% [8, 9], and single nucleotide polymorphisms (SNPs) in the coding and 5′ sequences of the gene [9, 10] define haplotypes at risk of type 2 diabetes that reduce adiponectin levels in diabetic and normoglycaemic populations [9, 11]. These data show that low adiponectin level might be one of the primary determinants of type 2 diabetes, which is in part genetically determined, a hypothesis that we recently evidenced further in the prospectively followed French Caucasian DESIR population [12]. The PPARG agonists, glitazones, increase adiponectin levels, suggesting that part of their hypoglycaemic action is mediated by the hormone release [13]. The PPARG Pro12Ala SNP is well established as a candidate gene for common forms of type 2 diabetes [14]. The relative risk (<1.20) conferred by the frequent at-risk allele cannot explain the whole genetic risk of type 2 diabetes as expected in multifactorial diseases where multiple genes intervene. An interaction between the Pro12Ala and ACDC SNPs was reported to modulate insulin sensitivity in a Chinese lean population [15], but their potential combined diabetogenic effect in overweight subjects is unknown.
Morbid obesity (BMI>40 kg/m2) is now a prevalent condition worldwide, targeting 0.5–5% of the adult population and constituting a major public health problem. Morbid obesity is associated with high premature mortality, mainly due to type 2 diabetes, cardiovascular diseases and several cancers. Apart from surgery, no treatment has yet been shown to effectively reverse morbid obesity. More than 100,000 severely obese subjects underwent bariatric surgery in the US in 2003 (10,000 in France), but the indications are still unclear and data on risk markers for metabolic and vascular complications as well as those more generally related to the health outcome of extreme cases of obesity are still missing. Indeed, morbidly obese subjects are generally insulin resistant, but the majority of these patients do not develop type 2 diabetes, and the molecular determinants of diabetes associated with obesity (diabesity) in this population are mostly unknown. We hypothesised that ACDC SNPs may be significant markers of the development of type 2 diabetes in the morbidly obese population, associated with a decrease in adiponectin levels and with worsening insulin resistance. There may also be interaction with other known or unknown diabetes susceptibility genes. To address this issue, we investigated 703 morbidly obese Caucasians and carried out the following: (1) an analysis of the effect of ACDC SNPs associated with type 2 diabetes and/or insulin resistance in less obese subjects [10, 11] on adiponectin levels and insulin sensitivity (evaluated by homeostasis model assessment [HOMA-S]); (2) an assessment of the contribution of ACDC SNPs and of the PPARG Pro12 allele to the risk of type 2 diabetes; and (3) an extension of the analyses to non-obese and obese subjects to search for interaction between genetic risk factors and corpulence.
Subjects and methods
Subjects
Unrelated, randomly selected subjects from French Caucasian families were included in the present study. Patients with a BMI of 40 kg/m2 or higher (n=703) formed the morbidly obese group (mean age 45.6±12.0 years, mean BMI 47.6±7.4 kg/m2, 25% men). Patients with a BMI below 40 kg/m2 (n=1,301) represented the population for which the at-risk 5′-sequences haplotype was initially reported [9]. In this population of 1,301 subjects, those with a BMI of 30 kg/m2 or higher formed the obese group (n=493, mean age 51.0±13.7 years, mean BMI 34.2±3.0 kg/m2, 41% men) and those with a BMI below 30 kg/m2 formed the non-obese group (n=808, mean age 60.6±12.2 years, mean BMI 25.1±2.6 kg/m2, 48% men). The ethics committee of Hôtel-Dieu Hospital Paris approved the protocol. Informed written consent was obtained beforehand. Only untreated diabetic patients were included in the study. The diabetic status was assessed for every subject according to the WHO criteria using fasting glycaemia for known diabetic patients and OGTT for other subjects. Adiponectinaemia was measured in patients for whom serum was available using a commercial assay kit (LINCO Research). Thus, adiponectinaemia data were available for 444 patients (mean age 45.3±11.6 years, mean BMI 47.4±7.1 kg/m2, 26% men) from the morbidly obese group, 307 patients (mean age 52.0±13.6 years, mean BMI 33.8±2.9 kg/m2, 39% men) from the obese group and 535 patients (mean age 60.9±11.6 years, mean BMI 25.2±725 kg/m2, 47% men) from the non-obese group. Insulin sensitivity was estimated using the HOMA model [9, 16].
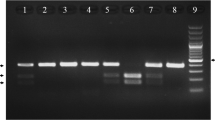
Genotyping of the ACDC SNPs
ACDC exon 3 SNPs were genotyped by direct sequencing and SNPs −11,391G>A, −11,377C>G, +45T>G and +276G>T were genotyped using LightCycler technology (Roche, Mannheim, Germany) as previously described [9]. Primer sequences and conditions are available on request.
Genotyping the PPARG Pro12Ala polymorphism
The PPARG Pro12Ala polymorphism was genotyped using Taqman technology (Applied Biosystems, assay on demand C_1129864_10; RS1801282). Samples were processed using a TECAN robotic device (TECAN Group, Switzerland), avoiding manual handling.
For every SNP used as a control quality test, 10% of the randomly selected subjects were regenotyped.
Statistical analyses
Genotype frequencies were compared by chi square or likelihood tests with determination of p values via permutations for allelic associations [17]. Linkage disequilibrium was estimated using Haploview software [18]. Continuous variables were compared using the Wilcoxon–Kruskal–Wallis test. The program THESIAS (Testing Haplotype Effects In Association Studies) was used to test the effect of a particular SNP inside a haplotype on a quantitative phenotype among unrelated individuals. This program is based on the maximum likelihood model described by Tregouet et al. [19] and is linked to the SEM algorithm [20]. To test for the effect of one SNP in a haplotype background we calculated the log likelihood in the general model (L all) and the likelihood in a model where some parameters (haplotype effects) are constrained. The effects of haplotypes that differ only for the tested SNP were set equally. We also estimated the effect of haplotypes by a method that estimates the haplotype frequency (and the probability vector of each individual) as well as the effect of the haplotype (haplotype trend regression [HTR]) [21]. This is equivalent to assigning probability scores. We inferred for each individual the most likely haplotypes using two different algorithms (EM and SSD) [22, 23] of the Genecounting and Phase softwares, respectively [23, 24]. Results of both inferences were compared and found to be similar. As the LD between the two loci was high (D′=−0.99) and mean posterior probability was 0.999, inferred haplotypes were then analysed as multi-allelic markers in subsequent statistical analyses. Adiponectin levels and HOMA-S insulin sensitivity indices were corrected for age, sex and BMI using multivariate linear regression of the log-transformed variables. Odds ratios and their 95% confidence intervals were determined using classical procedures. To test for interaction between corpulence and the genetic status, the method described by Paul and Donner was used. This tests whether odds ratios are significantly different across strata [25]. A p value of less than 0.05 was considered significant.
Results
Study of ACDC SNPs in the morbidly obese group
Allelic frequencies of ACDC exon 3 missense mutations G90S and Y111H were 0.993/0.007 and 0.975/0.025, respectively. No previously reported or new mutations were detected in this sample.
Genotype and allelic frequencies for SNPs −11,391G>A, −11,377C>G, +45T>G (G15G) and +276G>T are presented in Table 1. Except SNP +45T>G, all SNPs were in Hardy–Weinberg equilibrium. Therefore, we regenotyped SNP +45 in the 703 morbidly obese patients and the results were in accordance with the initial genotyping (99% concordance). Standardised linkage disequilibrium (D′) between all studied SNPs is presented in Table 2. The values are similar to those previously reported in a French population of unrelated obese and non-obese subjects [9]. The association of each SNP with adjusted adiponectin levels was first assessed. As reported in the literature, adiponectin levels were lower in diabetic patients than in normoglycaemic patients [3]. Nevertheless, associations between adiponectin level and genetic variations (SNPs, haplotypes) were similar in the normoglycaemic and diabetic groups, taken separately (data not shown), allowing us to investigate the 444 morbidly obese patients for whom adiponectinaemia data were available as a single group. 5′-ACDC SNP −11,391 was associated with adjusted adiponectin levels (p=0.0003, adiponectin levels: 5.55±0.11, 6.57±0.23 and 8.09±0.76 μg/ml for GG, GA and AA genotypes, respectively). Likewise, an association was detected with SNP −11,377 (p=0.008, adiponectin levels: 6.05±0.13, 5.48±0.18 and 4.80±0.43 μg/ml for CC, CG and GG genotypes, respectively). A weak association with adjusted adiponectin level was displayed by SNP +276 (p=0.04). SNP +45 was not associated with adjusted adiponectin levels (p=0.97). As previous studies reported associations of adiponectin levels with SNPs −11,391 and −11,377 [9] or SNPs +45 and +276 [10], haplotypes including these four SNPs were constructed and analysed using Thesias software to estimate the individual effect of each SNP included in the four-loci haplotype on adjusted adiponectin level. The results excluded the possibility of significant individual effects of SNPs +45 and +276 (p=0.97 and p=0.65, respectively) but showed significant individual effects of SNPs −11,391 (p=0.0007) and −11,377 (p=0.012). These data were confirmed using HTR software, with adjusted adiponectin level as a quantitative trait, showing a strong association with haplotypes including the −11,391 and −11,377 SNPs (p<0.0001) but not with haplotypes including SNP +45 and +276 (p>0.5). Thus, haplotypes including the −11,391 and −11,377 SNPs were further investigated. HTR analysis of the −11,391 and −11,377 haplotypes using adjusted adiponectin level showed an association of the G_G haplotype with the lowest adjusted adiponectin levels (p=0.006) and of the A_C haplotype with the highest adjusted adiponectin levels (p<0.0001). Thus, regarding adiponectin levels, G_G and A_C haplotypes were considered ‘low-level’ and ‘high-level’, respectively. These associations of given haplotypes with adjusted adiponectin levels are far more significant than those with SNPs taken individually, in agreement with an ‘additive’ effect of both SNPs.
Haplotypes of the −11,391 and −11,377 SNPs of the promoter were then inferred for each subject, providing a diploid configuration. The two different algorithms used (EH and SSD) gave similar results. Inferred haplotypes were in Hardy–Weinberg equilibrium (data not shown). Adjusted adiponectin levels significantly differed according to diploid configuration (p=0.0015, Table 3). They were lower in subjects with at least one “low-level” haplotype and were higher for subjects with at least one ‘high-level’ haplotype. ACDC exon 3 rare mutation (G90S or Y111H) did not significantly modulate adiponectin levels in morbidly obese subjects (Table 4). The HOMA-S insulin sensitivity index was only determined for normoglycaemic subjects (n=270). As expected, the PM+EH+ software disclosed a significant association of the “low-level” G_G haplotype (p=0.01) with low insulin sensitivity confirmed by HTR analysis (p=0.04).
As SNPs −11,391 and −11,377 were associated with adiponectin levels, their haplotypes were analysed in subgroups of type 2 diabetes patients and normoglycaemic morbidly obese patients. When inferring haplotypes, the wild-type/‘low-level’ 5′-ACDC diploid configuration displayed a significantly increased risk of type 2 diabetes (OR 1.92 [95% CI 1.27–2.93], p=0.002, Table 5). Thus, this wild-type/“low-level” 5′-ACDC diploid configuration was considered to be an ‘at-risk’ genetic status. In contrast, allelic frequencies of the PPARG Pro12Ala SNP were not different in diabetic and normoglycaemic morbidly obese groups (0.89/0.11), and the PPARG Pro12 allele was not associated with HOMA-S or with adiponectin levels in this population. Moreover, we were unable to detect any effect of the PPARG Pro12Ala SNP and ACDC genetic variants on the risk of type 2 diabetes.
Investigations of the role of corpulence
To investigate the effect of corpulence on the genetic risk of type 2 diabetes conferred by ACDC and Pro12Ala PPARG SNPs, data of a group of 1,301 unrelated Caucasian subjects (BMI 28.5±7.5 kg/m2, range 20–39.9 kg/m2), in whom an association with type 2 diabetes and ACDC SNPs had been previously reported [9], were included in the present study. ACDC promoter haplotype diploid configurations were inferred for each subject of this group using Genecounting and Phase softwares as described above. Thus, pooling the morbidly obese population with this group of 1,301 subjects offered a cohort of 2004 unrelated subjects covering a broad BMI range. Three groups were then defined according to WHO criteria: (1) non-obese subjects (BMI <30 kg/m2, n=808); (2) obese subjects (30≤BMI<40 kg/m2, n=493); and (3) the above-described morbidly obese group (BMI ≥40 kg/m2, n=703). As shown in Table 3, the 5′-ACDC promoter haplotype diploid configuration significantly modulated adiponectin levels in the three groups. Conversely, the ACDC exon 3 missense mutations only modified adiponectin levels in the non-obese group (Table 4). The PPARG Pro12Ala SNP did not significantly modulate adiponectin level in any group of subjects (data not shown).
We further estimated the risk of type 2 diabetes associated with ACDC and PPARG SNPs according to corpulence (Table 5). The 5′-ACDC haplotype ‘at-risk’ diploid genetic status approximately ‘doubles’ the risk of type 2 diabetes in morbidly obese subjects, and was also associated with type 2 diabetes in the less obese population (OR 1.73 [95% CI: 1.07–2.82]) but not in the non-obese group.
The method described by Paul and Donner [25] to test whether odds ratios differ across the three groups of BMI showed a borderline significant result (p=0.048), in agreement with the notion of an interaction between corpulence and the genetic status at the ACDC promoter. Using the same test, no effect of corpulence and the genotype at the ACDC promoter on adiponectin level was detected (p=0.073). The ACDC exon 3 mutations were only associated with type 2 diabetes in the non-obese group (OR 7.85 [95% CI: 3.30–19.36]). Likewise, the PPARG Pro12Ala SNP only displayed a trend of association with type 2 diabetes in the non-obese group (OR 1.40 [95% CI: 0.94–2.09]). No significant interaction was detected between the PPARG Pro12Ala SNP and corpulence (p=0.42).
Discussion
All the patients included in the present study are unrelated French Caucasians. Although unlikely, we cannot exclude the possibility of bias resulting from unknown population stratification or cryptic relatedness. One of the major results of this study is the important association of the known 5′-ACDC SNP haplotype (including SNPs −11,391 and −11,377) with the genetic risk of type 2 diabetes in morbidly obese Caucasian subjects. This haplotype or an unknown nearby functional variant in linkage disequilibrium would decrease adiponectin levels and subsequent insulin sensitivity. These data corroborate those obtained in less obese subjects from different ethnic groups [9–11] and provide further evidence for the association of ACDC promoter SNP with the genetic modulation of adiponectinaemia and insulin sensitivity. Moreover, a prospective study in a general Caucasian population reported that genetic variations at the ACDC gene (including SNP −11,391) modulated adiponectin levels and increased the risk of becoming diabetic [12]. Although we could not detect an impact of ACDC promoter genetic variants on type 2 diabetes in non-obese subjects, they were closely associated with type 2 diabetes in obese (OR 1.73) and morbidly obese (OR 1.92) subjects, confirming the physiological role of adiponectin in the protection against the deleterious metabolic effects of an excess in corpulence. Indeed, interaction between corpulence and genetic variants only reached a level of significance of 0.048, as tested by the Paul and Donner test. It is well known that such statistical procedures used to test for interaction have a very low power [26, 27]. This reinforces the relevance of the interaction we report. Our data suggest for the first time that ‘effects’ of type 2 diabetes susceptibility gene variations may differ according to the level of corpulence. Indeed, ACDC exon 3 mutations are only type 2 diabetes risk factors in non-obese diabetic individuals, where they are rather prevalent (11%), although they are rare (<5%), in all other groups. It is worth noting that the most striking effects of several missense mutations in ACDC exon 3 were found in Japanese individuals, a population with a relatively low BMI [28]. The effect of these mutations is unclear but could involve both reduction of adiponectin level and impairment of the adiponectin multimerisation, which may impact signalling in tissues such as the liver [29].
The prevalence of the 5′-ACDC SNP diploid configuration associated with hypoadiponectinaemia was equally high in all type 2 diabetes groups, irrespective of the severity of obesity (39.4% in non-obese, 35.2% in obese and 36.8% in morbidly obese subjects). However, only 28.7% of obese and 25.9% of morbidly obese normoglycaemic subjects carry this type 2 diabetes-associated configuration compared with 35.3% in the non-diabetic non-obese group. Thus, the genetic profiles of the normoglycaemic obese or morbidly obese groups are characterised by a very low frequency of the 5′-ACDC SNPs associated with hypoadiponectinaemia, which suggests that the maintenance of sustained adiponectin levels is a key protecting factor against type 2 diabetes linked to obesity.
Is there a minimum adiponectin value under which obesity is highly associated with type 2 diabetes? Based on our data, values of 4.47–5.41 μg/ml observed in obese subjects carrying the 5′-ACDC SNP at-risk diploid configuration may be seen as a threshold for increasing the risk of type 2 diabetes two-fold. In this range of hypoadiponectinaemia, an impairment of PPARG activity provided by the Pro12 allele may have no detectable additional deleterious effect on insulin resistance. Prospective studies of morbidly obese individuals will indicate whether our assumption is correct. If true, a therapeutic goal to prevent the development of diabetes in the obesity context would be to restore adiponectin levels above 5 μg/ml.
Intriguingly, no association with BMI was detected in this study, although it was suggested that ACDC variants modulate visceral fat accumulation [30], a major risk factor for type 2 diabetes. In massively obese individuals, there is no specific regional adipose disposition but a large extent of multiple organ ectopic fat. In addition, the evaluation of body composition that might be heterogeneous is very difficult in these subjects. Given the role of adiponectin in fatty acid oxidation, a further reduction of adiponectin levels in massively obese subjects driven or associated with an at-risk ACDC diplotype, may impact the ability to ‘clear’ cellular fat depots. Metabolic investigation would be necessary in these subjects. In this regard, obese and morbidly obese subjects homozygous for the 5′-ACDC SNP haplotype associated with higher adiponectin levels and with a reduced risk of type 2 diabetes have nearly normal adiponectin levels, suggesting that if normal values of adiponectin are restored, the risk of diabesity would be greatly reduced. In obese subjects, ACDC genetic effects are not negligible. Obese and morbidly obese individuals homozygous for the ‘low-level’ haplotype have a 40–50% reduction of adiponectin levels compared with subjects with ‘high-level’ haplotype homozygous carriers, and this may have a non-negligible impact on the risk of type 2 diabetes.
In contrast to ACDC promoter SNPs, the PPARG Pro12Ala SNP only displayed a trend of association with type 2 diabetes in the non-obese group; an association with type 2 diabetes in obese groups failed to be demonstrated [31]. The OR found here in non-obese and obese groups (1.40 and 1.39, respectively) are in the same range as those previously reported in other populations [14]. In the morbidly obese group we did not find an association between the PPARG Pro12Ala SNP and type 2 diabetes, and allelic frequencies are very similar in the normoglycaemic and diabetic groups. However, we cannot exclude a lack of power. If the PPARG Pro12Ala SNP is associated with adiponectin level in the Japanese population [32], our results did not show such an association in a Caucasian population, in agreement with previous studies [33]. In a similar way we were unable to detect any effect of the PPARG Pro12Ala SNP and ACDC genetic variants on the risk of type 2 diabetes, although it was reported in a Japanese population [15].
If confirmed in other ethnic groups, our data will indicate that the genetic background associated with type 2 diabetes development may be different between morbidly obese individuals and non-obese or overweight subjects.
Obesity (BMI >30 kg/m2) and morbid obesity affect 30.5 and 4.7% of the US population, respectively [34]. Given the worldwide epidemic of the onset of obesity at an early age, it is likely that the contribution of adiponectin in diabesity will tend to increase. In this context, taking into account ACDC variants and adiponectin levels, in assessing further risk of type 2 diabetes and premature CHD [5] may more effectively encourage subjects who could benefit from help in the future to prevent the diseases and to determine a more efficient treatment increasing adiponectin secretion or action. Furthermore, the search for diabesity genes in morbidly obese subjects is crucial to establish the genetic profile of this very high-risk population and for a better understanding of the molecular determinants of metabolic complications of obesity.
Abbreviations
- ACDC :
-
adipocyte C1q and collagen-domain-containing
- HOMA:
-
homeostasis model assessment
- HTR:
-
haplotype trend regression
- OR:
-
odds ratio
- PPARG :
-
peroxisome proliferator-activated receptor gamma
- SNP:
-
single nucleotide polymorphism
- WHO:
-
World Health Organization
References
Garaulet M, Viguerie N, Porubsky S et al (2004) Adiponectin gene expression and plasma values in obese women during very-low-calorie diet: relationship with cardiovascular risk factors and insulin resistance. J Clin Endocrinol Metab 89:756–760
Liu YM, Lacorte JM, Viguerie N et al (2003) Adiponectin gene expression in subcutaneous adipose tissue of obese women in response to short-term very low calorie diet and refeeding. J Clin Endocrinol Metab 88:5881–5886
Weyer C, Funahashi T, Tanaka S et al (2001) Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 86:1930–1935
Yamauchi T, Kamon J, Waki H et al (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 7:941–946
Ouchi N, Kihara S, Arita Y et al (2001) Adipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Circulation 103:1057–1063
Spranger J, Kroke A, Mohlig M et al (2003) Adiponectin and protection against type 2 diabetes mellitus. Lancet 361:226–228
Lindsay RS, Funahashi T, Hanson RL et al (2002) Adiponectin and development of type 2 diabetes in the Pima Indian population. Lancet 360:57–58
Comuzzie AG, Funahashi T, Sonnenberg G et al (2001) The genetic basis of plasma variation in adiponectin, a global endophenotype for obesity and the metabolic syndrome. J Clin Endocrinol Metab 86:4321–4325
Vasseur F, Helbecque N, Dina C et al (2002) Single-nucleotide polymorphism haplotypes in both the proximal promoter and exon 3 of the APM1 gene modulate adipocyte-secreted adiponectin hormone levels and contribute to the genetic risk for type 2 diabetes in French Caucasians. Hum Mol Genet 11:2607–2614
Hara K, Boutin P, Mori Y et al (2002) Genetic variation in the gene encoding adiponectin is associated with an increased risk of type 2 diabetes in the Japanese population. Diabetes 51:536–540
Menzaghi C, Ercolino T, Di Paola R et al (2002) A haplotype at the adiponectin locus is associated with obesity and other features of the insulin resistance syndrome. Diabetes 51:2306–2312
Fumeron F, Aubert R, Siddiq A et al (2004) Adiponectin gene polymorphisms and adiponectin levels are independently associated with the development of hyperglycemia during a 3-year period: the epidemiologic data on the insulin resistance syndrome prospective study. Diabetes 53:1150–1157
Maeda N, Takahashi M, Funahashi T et al (2001) PPARgamma ligands increase expression and plasma concentrations of adiponectin, an adipose-derived protein. Diabetes 50:2094–2099
Altshuler D, Hirschhorn JN, Klannemark M et al (2000) The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet 26:76–80
Yang WS, Hsiung CA, Ho LT et al (2003) Genetic epistasis of adiponectin and PPARgamma2 genotypes in modulation of insulin sensitivity: a family-based association study. Diabetologia 46:977–983
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Zhao JH, Curtis D, Sham PC (2000) Model-free analysis and permutation tests for allelic associations. Hum Hered 50:133–139
Barrett JC, Fry B, Maller J, Daly MJ (2004) Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21:263–265
Tregouet DA, Barbaux S, Escolano S et al (2002) Specific haplotypes of the P-selectin gene are associated with myocardial infarction. Hum Mol Genet 11:2015–2023
Tregouet DA, Escolano S, Tiret L, Mallet A, Golmard JL (2004) A new algorithm for haplotype-based association analysis: the Stochastic-EM algorithm. Ann Hum Genet 68:165–177
Zaykin DV, Westfall PH, Young SS, Karnoub MA, Wagner MJ, Ehm MG (2002) Testing association of statistically inferred haplotypes with discrete and continuous traits in samples of unrelated individuals. Hum Hered 53:79–91
Excoffier L, Slatkin M (1995) Maximum-likelihood estimation of molecular haplotype frequencies in a diploid population. Mol Biol Evol 12:921–927
Stephens M, Smith NJ, Donnelly P (2001) A new statistical method for haplotype reconstruction from population data. Am J Hum Genet 68:978–989
Zhao JH, Lissarrague S, Essioux L, Sham PC (2002) Genecounting: haplotype analysis with missing genotypes. Bioinformatics 18:1694–1695
Paul SR, Donner A (1989) A comparison of tests of homogeneity of odds ratios in K 2×2 tables. Stat Med 8:1455–1468
Greenland S (1983) Tests for interaction in epidemiologic studies: a review and a study of power. Stat Med 2:243–251
Jones MP, O’Gorman TW, Lemke JH, Woolson RF (1989) A Monte Carlo investigation of homogeneity tests of the odds ratio under various sample size configurations. Biometrics 45:171–181
Kondo H, Shimomura I, Matsukawa Y et al (2002) Association of adiponectin mutation with type 2 diabetes: a candidate gene for the insulin resistance syndrome. Diabetes 51:2325–2328
Waki H, Yamauchi T, Kamon J et al (2003) Impaired multimerization of human adiponectin mutants associated with diabetes: molecular structure and multimer formation of adiponectin. J Biol Chem 278:40352–40363
Patel S, Unwin NC, Vasseur F, Froguel P, Walker M (2002) Investigation of the role of the T to G SNP in the adiponectin (APM1) gene in abdominal obesity using parent–offspring trios. Abstract of 38th annual meeting of the EASD. Diabetologia 45:413
Clement K, Hercberg S, Passinge B et al (2000) The Pro115Gln and Pro12Ala PPAR gamma gene mutations in obesity and type 2 diabetes. Int J Obes Relat Metab Disord 24:391–393
Yamamoto Y, Hirose H, Miyashita K et al (2002) PPAR(gamma)2 gene Pro12Ala polymorphism may influence serum level of an adipocyte-derived protein, adiponectin, in the Japanese population. Metabolism 51:1407–1409
Thamer C, Machicao F, Fritsche A, Stumvoll M, Haring H (2003) No influence of the PPARgamma2 Pro12Ala genotype on serum adiponectin concentrations in healthy Europeans. Metabolism 52:798; author reply 798–799
Flegal KM, Carroll MD, Ogden CL, Johnson CL (2002) Prevalence and trends in obesity among US adults, 1999–2000. JAMA 288:1723–1727
Acknowledgements
The authors wish to thank L. Olfert (Tib Molbiol Syntheselabor, Germany) for the design of the LightCycler probes. This work was partly supported by EU-funded Grants GIFT QLG2-CT-1999-00546 and NUGENOB QLK1-CT-2000-00618, and by grants of the Association Française des Diabétologues de Langue Française (ALFEDIAM), of the Direction de la Recherche Clinique/Assistance Publique-Hôpitaux de Paris and the Programme Hospitalier de Recherche Clinique (AOM 96088) and of the Association Française des Diabétiques (AFD). F. Vasseur and N. Helbecque contributed equally to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vasseur, F., Helbecque, N., Lobbens, S. et al. Hypoadiponectinaemia and high risk of type 2 diabetes are associated with adiponectin-encoding (ACDC) gene promoter variants in morbid obesity: evidence for a role of ACDC in diabesity. Diabetologia 48, 892–899 (2005). https://doi.org/10.1007/s00125-005-1729-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1729-z