Abstract
Aims/hypothesis
Established autoimmune markers of type 1 diabetes, including islet cell autoantibodies (ICA) and autoantibodies to glutamic acid decarboxylase (GADA) have been used to screen people presenting with type 2 diabetes for latent autoimmune diabetes in adults. We have examined the prevalence of autoantibodies to protein tyrosine phosphatase isoforms IA-2 (IA-2A) and IA-2β/phogrin (IA-2βA) in a cohort of adult UKPDS patients thought to have type 2 diabetes, and investigated the possible role of these autoantibodies in predicting requirement for insulin therapy.
Methods
IA-2A and IA-2βA were measured by a validated radioimmunoassay with human recombinant autoantigens in 4,169 white Caucasian patients aged 25–65 years and newly diagnosed with type 2 diabetes. The clinical requirement for insulin therapy within 6 years was examined in 2,556 patients not randomised to insulin.
Results
IA-2A and IA-2βA were present in 2.2 and 1.4%, respectively, of these patients. IA-2A were more prevalent in younger patients (p for trend <0.00001), more often associated with the HLA-DR4 allele (26.3 vs 8.0%, p<0.0001), and their presence increased the likelihood of insulin therapy requirement within 6 years from diagnosis [relative risk (95%CI) 12.2 (9.8–15.3)]. The presence of IA-2A together with GADA increased the relative risk of requiring insulin therapy from 5.4 (4.1–7.1) for GADA alone to 8.3 (3.7–18.8) and the corresponding positive predictive value from 33 to 50%.
Conclusions/interpretation
In type 2 diabetes, the presence of IA-2A is infrequent, associated with the HLA-DR4 haplotype, and highly predictive of future need for insulin therapy. The measurement of IA-2βA does not provide additional information.
Similar content being viewed by others
Introduction
Type 1 diabetes can occur at any age and in adults may masquerade initially as type 2 diabetes with slow deterioration in metabolic control before progressing to insulin dependency. This process, termed latent autoimmune diabetes in adults (LADA) [1], has been classified by the World Health Organization (WHO) [2] as a slowly progressive form of type 1 autoimmune diabetes with a phenotype in adults that is clinically indistinguishable from that of type 2 diabetes. Identifying LADA patients is important, as they often require insulin therapy earlier than those with type 2 diabetes [3] and may respond differently when included in diabetes prevention or intervention trials.
Established autoimmune markers of type 1 diabetes include autoantibodies to islet cell cytoplasm (ICA), to glutamic acid decarboxylase (GADA), insulin (IAA) and protein tyrosine phosphatase isoforms IA-2 (IA-2A) and IA-2β/phogrin (IA-2βA). ICA and GADA have been used to screen for LADA and to help predict future need for insulin therapy [4, 5]. UK Prospective Diabetes Study (UKPDS) analyses [4] showed that, by 6 years from diagnosis of presumed type 2 diabetes, 38% of subjects requiring insulin were GADA-positive, whereas 95% of those not requiring insulin were GADA-negative. IAA, which are a frequent marker of childhood diabetes, with a frequency inversely related to age [6], are unlikely to be useful for LADA screening.
IA-2A and IA-2βA [7] have been described in adults presenting with type 2 diabetes but their clinical relevance is uncertain. We have examined their prevalence and clinical associations in UKPDS patients and analysed their predictive value, together with GADA and ICA, for the clinical requirement for insulin by 6 years from diagnosis of presumed type 2 diabetes.
Subjects, materials and methods
Patients
We studied 4,169 of 5,102 UKPDS patients who were white Caucasians and for whom IA-2A and IA-2βA assay results were available. The UKPDS recruited patients who were aged 25–65 years with type 2 diabetes newly diagnosed by their general practitioner, and with two subsequent fasting plasma glucose (FPG) values above 6.0 mmol/l. Exclusion criteria were: severe vascular disease (myocardial infarction in the past year, current angina or heart failure), accelerated hypertension, proliferative or pre-proliferative retinopathy, renal failure with plasma creatinine greater than 175 μmol/l, other life-threatening disease such as cancer, an illness requiring systemic steroids, an occupation precluding insulin treatment, unfamiliarity with English, and ketonuria greater than 3 mmol/l, which is suggestive of type 1 diabetes.
The UKPDS design has been reported [8]. It was carried out according to the Helsinki guidelines, all patients gave informed consent and the protocol received Research Ethics Committee approval. After a 3-month dietary run-in period patients with FPG values between 6.0 and 14.9 mmol/l and without hyperglycaemic symptoms were randomised to diet, insulin, sulphonylurea or metformin (if overweight) therapy. Those with FPG values of 15.0 mmol/l or higher, or with hyperglycaemic symptoms were randomised to therapies other than diet. Those with FPG values below 6.0 mmol/l remained on diet alone but were randomised as above, if their FPG values subsequently rose to 6.0 mmol/l or higher. The UKPDS protocol [8] stipulated that patients not randomised to insulin became insulin-requiring only when FPG values were 15.0 mmol/l or higher, or hyperglycaemic symptoms developed after therapy with maximum tolerated doses of sulphonylurea and metformin.
Autoantibodies
Plasma IA-2A and IA-2βA levels were determined on samples taken within 1 year of diagnosis, using a combined radiobinding assay [9, 10] and retested if higher than the 95th centile. 1.2% of samples assayed were taken at 2 or 3 years from diagnosis. Levels were converted into arbitrary units by extrapolation from a standard curve and thresholds for positivity determined from the 99th centile of control subjects. These corresponded to 1 unit for IA-2A and IA-2βA. The IA-2A assay used has been shown to have 58% sensitivity and 100% specificity for the diagnosis of diabetes in the first assay proficiency evaluation of the diabetes antibody standardisation programme [11]. ICA and GADA were measured by indirect immunofluorescence and radiobinding assays respectively, as reported previously [4]. ICA positivity was taken as 5 JDF units or more and GADA positivity as 20 reference units or more. The sensitivity and specificity of the assays for the diagnosis of diabetes at these thresholds were 88 and 97% for ICA [12] and 75 and 100% for GADA under the conditions of the JDF Combinatorial Autoantibody Workshop of 1995 [13].
Clinical and biochemical measurements
Age, sex and ethnicity were recorded at diagnosis and FPG, fasting plasma insulin (FPI), HbA1c and BMI after the dietary run-in. FPG, FPI and HbA1c levels were assayed as described previously [14]. Beta cell function and insulin sensitivity were derived from simultaneous FPG and FPI measurements by Homeostasis model assessment (HOMA) [15, 16], using the HOMA2 Calculator (http://www.dtu.ox.ac.uk). The relationship of IA-2A to HLA DRB1*03, DRB1*04 and the high-risk DRB1*04-DQB1*0302 haplotype was assessed in a subgroup of 2,168 patients previously genotyped for these loci [17].
Statistical analysis
Statistical analyses were performed using SAS version 8.2 (SAS Institute, Cary, NC, USA). Data are reported as means (±standard deviation), median (interquartile range [IQR]) or as percentages. Comparisons of continuous data employed two-sample t-tests or Wilcoxon’s signed-rank test for non-normally distributed data. Chi square tests were used for categorical variables or, where cells contained less than 5% of the data, Fisher’s exact test. The Cochran–Armitage test for trend was used where appropriate. Specificity, sensitivity and positive predictive values (PPV) were calculated from frequency tables comparing positive groups with those negative for all three autoantibodies. Relative risks (RR) were calculated from these same frequency tables. Multivariate logistic regression analysis was used to assess the importance of demographic and clinical characteristics to the requirement for insulin at 6 years. All variables were entered simultaneously into the model. All p values are quoted to two significant figures with p<0.05 taken as conventionally significant.
Results
IA-2A and IA-2βA prevalence and clinical associations
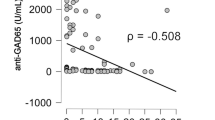
Of the 4,169 white Caucasian patients studied here, 93 (2.2%) were positive for IA-2A (irrespective of IA-2βA) and 58 (1.4%) for IA-2βA (irrespective of IA-2A) at diagnosis (Table 1). There were 42 (1.0%) patients positive for IA-2A alone, seven (0.2%) for IA-2βA alone and 51 (1.4%) for both IA-2A and IA-2βA. As only seven patients were positive for IA-2βA but not positive for IA-2A, subsequent analyses are restricted to the 93 IA-2A-positive patients. The prevalence of IA-2A positivity was inversely related to age (p for trend <0.00001). The HLA DRB1*03/DRB1*04 genotype was present in a higher proportion of IA-2A-positive (28.3%) than IA-2A-negative (9.0%) patients (p<0.0001). HLA DRB1*04 was present in 66.7% of IA2A-positive, compared with 36.2% of IA-2A-negative patients, irrespective of DRB1*03 (p<0.0001).
In addition to being younger, IA-2A-positive compared with IA-2A-negative patients (Table 2) had lower BMI and beta cell function but higher (p<0.00001) FPG, HbA1c and insulin sensitivity. These relationships were consistent across 5-year age groups, with the exception of HbA1c (data not shown).
IA-2A, ICA, GADA and early requirement for insulin therapy
The prevalence of various islet autoantibody combinations in the 2,556 patients with assay results for all three autoantibodies, randomised initially to therapies other than insulin, are reported in Table 3. Of these patients, 268 (10.5%) clinically required insulin therapy by 6 years, of whom 257 (10.0%) had GADA, 141 (5.5%) had ICA and 57 (2.2%) had IA-2A. Overall, 316 (12.4%) were positive for at least one autoantibody and 96 (3.8%) were positive for two or three autoantibodies. Patients older than 45 years at diagnosis were more likely to require insulin than those aged 45 years or less (23.4 vs 7.8% respectively, p<0.00001).
The presence of any one islet autoantibody in patients requiring insulin (133/268) conferred an RR (95% CI) of 12.2 (9.8–15.3) for IA–2A, 8.8 (7.0–11.1) for ICA and 8.1 (6.6–9.9) for GADA (Table 3). The PPV for IA-2A, irrespective of GADA or ICA, was 74 and 76% for ICA+GADA. ICA, irrespective of GADA or IA-2A, gave a PPV of 53%, while GADA, irrespective of IA-2A or ICA, gave 49% (Table 3). Sensitivity was lowest for IA-2A (24%), compared with 36% for ICA and 48% for GADA, while specificity for each autoantibody was high. IA-2A positivity was significantly associated with both ICA and GADA positivity (p<0.00001), and was found in the absence of ICA and GADA in only six patients. The increased risk for early insulin requirement in younger patients was consistent throughout (data not shown).
GADA levels were significantly higher in patients positive for both GADA and ICA than in patients positive for GADA alone [median (IQR) 99 (89–111) vs 52 (30–91), p<0.0001]. Stratification of patients by quartiles of GADA levels for all those with GADA higher than 20 units, of whom three had missing ICA data, showed a significant trend for a higher likelihood of requiring insulin within 6 years of diagnosis of diabetes with higher GADA levels: 48 of 65 (74%) with 101.5 units or more, 36 of 65 (55%) with 82.5 units or more and less than 101.5 units, 30 of 65 (46%) with 37.5 units or more and less than 82.5 units and 13 of 65 (20%) with 20 units or more and less than 37.5 units (p<0.000001 for trend across the groups).
Multivariate logistic regression analysis of the likelihood of requiring insulin by 6 years showed that in patients younger than 45 years at diagnosis GADA status, IA-2A status and beta cell function were significant predictors. In patients aged 45 years or older at diagnosis, GADA and ICA status, but not IA-2A status were significant, along with beta cell function and male sex (Table 4).
Discussion
IA-2A were present in only 2.2% of adults presenting with type 2 diabetes and recruited into the UKPDS. Their presence, however, significantly increased the likelihood that insulin therapy would be required within 6 years of diagnosis, as reported previously for GADA [4, 5]. As for GADA, IA-2A were more prevalent in patients who were diagnosed younger, and their presence identified a subset of patients with more prominent characteristics of insulin deficiency. The association of IA-2A with the HLA-DR4 phenotype observed in juvenile-onset type 1 diabetes [18], was confirmed in this cohort of adult-onset autoimmune diabetes. The presence of IA-2A in addition to GADA increased the RR of requiring insulin therapy within 6 years of diagnosis from 5.4 for GADA alone to 8.3, although this increase was not statistically significant because of the small numbers of patients with both IA-2A and GADA positivity; it increased the corresponding PPV from 33 to 50%.
Measurement of IA-2A or ICA identified few cases in addition to GADA, which remained the most sensitive autoantibody marker for identifying UKPDS patients who would require insulin [19]. A substantial number of patients were positive for ICA but not GADA or IA-2A (19%), but the likelihood of requiring insulin in these patients was similar to that in patients negative for all three autoantibodies, indicating that ICA reactivity in itself was not a specific marker for rapid loss of beta cell function and should not be considered typical of LADA. Nevertheless, like IA-2A, ICA stratified risk in GADA-positive patients, indicating that the measurement of ICA in such patients can be useful. As shown previously [4], GADA levels were significantly higher in patients who were also ICA-positive and effective stratification of the likelihood of requiring insulin could be achieved by GADA levels alone. The introduction of the WHO standard for GADA measurement [20], and the relatively high concordance in GADA quantification observed in international standardisation programmes [11], makes this strategy feasible. GADA together with IA-2A or ICA, or alternatively quantified measurement of GADA, is therefore recommended for the classification of adult patients with type 2 diabetes for inclusion in trials of immune intervention. Recent studies of GADA and other markers of autoimmunity in various populations have highlighted the difficulties of classifying diabetes in adults, suggesting that many genetic and clinical research studies, as well as pharmaceutical trials of therapies for type 2 diabetes, may have been confounded by the inclusion of LADA subjects [21]. Correct classification of subjects in trials of prevention of type 2 diabetes that are now underway may also be a problem. We recommend that all participants in future type 2 diabetes studies be screened for GADA and other autoantibodies. This may be especially important in genetic [22] as well as therapeutic studies.
Participating UK Centres
Radcliffe Infirmary, Oxford; Royal Infirmary, Aberdeen; University Hospital, Birmingham; St. George’s Hospital, Hammersmith Hospital and Whittington Hospital, London; City Hospital and Royal Victoria Hospital, Belfast; North Staffordshire Royal Infirmary, Stoke-on-Trent; St. Helier Hospital, Carshalton; Norfolk and Norwich Hospital, Norwich; Lister Hospital, Stevenage; Ipswich Hospital, Ipswich; Ninewells Hospital, Dundee; Northampton General Hospital, Northampton; Torbay Hospital, Torbay; Peterborough General Hospital, Peterborough; Scarborough Hospital, Scarborough; Derbyshire Royal Infirmary, Derby; Manchester Royal Infirmary, Manchester; Hope Hospital, Salford; Leicester General Hospital, Leicester; Royal Exeter and Devon Hospital, Exeter.
Abbreviations
- FPG:
-
fasting plasma glucose
- FPI:
-
fasting plasma insulin
- GADA:
-
glutamic acid decarboxylase autoantibodies
- HOMA:
-
homeostasis model assessment
- IAA:
-
antibodies to insulin
- IA-2A:
-
protein tyrosine phosphatase isoforms IA-2
- IA-2βA:
-
IA-2β/phogrin
- ICA:
-
islet cell autoantibodies
- IQR:
-
interquartile range
- JDF:
-
Juvenile Diabetes Federation
- LADA:
-
latent autoimmune diabetes in adults
- PPV:
-
positive predictive value
- RR:
-
relative risk
- UKPDS:
-
United Kingdom Prospective Diabetes Study
- WHO:
-
World Health Organization
References
Tuomi T, Groop LC, Zimmet PZ, Rowley MJ, Knowles W, Mackay IR (1993) Antibodies to glutamic acid decarboxylase reveal latent autoimmune diabetes mellitus in adults with a non-insulin-dependent onset of disease. Diabetes 42:359–362
World Health Organization (1999) Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications Report of a WHO Consultation Part 1: Diagnosis and Classification of Diabetes Mellitus
Atkinson M, Eisenbarth G (2001) Type 1 diabetes: new perspectives on disease pathogenesis and treatment. Lancet 358:221–229
UKPDS Group (1997) UKPDS 25: Clinical value of ICA and GADA in predicting insulin requirement in patients with newly diagnosed NIDDM at different ages. Lancet 350:1288–1293
Tuomi T, Carlsson A, Isomaa B et al (1999) Clinical and genetic characteristics of type 2 diabetes with and without GAD antibodies. Diabetes 48:150–157
Vardi P, Ziegler AG, Mathews JH et al (1988) Concentration of insulin autoantibodies at onset of type 1 diabetes. Inverse log-linear correlation with age. Diabetes Care 11:736–739
Notkins A, Lan M, Leslie R (1998) IA-2 and IA-2beta: the immune response in IDDM. Diabetes/Metab Rev 14:85–93
UKPDS Group (1991) UK Prospective Diabetes Study VIII: study design, progress and performance. Diabetologia 34:877–890
Bonifacio E, Lampaspona V, Genovese S, Ferrari M, Bosi E (1995) Identification of protein tyrosine phosphatase-like IA2 (islet cell antigen 512) as the insulin-dependent diabetes-related 37/40K autoantigen and a component of islet cell antibodies. J Immunol 155:5419–5426
Bonifacio E, Lampaspona V, Bingley PJ (1998) IA-2 (islet cell antigen 512) is the primary target of humoral autoimmunity against type 1 diabetes-associated tyrosine phosphate autoantigens. J Immunol 161:2648–2654
Bingley PJ, Bonifacio E, Mueller P (2003) Diabetes antibody standardization program: first assay proficiency evaluation. Diabetes 52:1128–1136
Bonifacio E, Bingley PJ, Shattock M et al (1990) Quantification of islet-cell antibodies and prediction of insulin dependent diabetes. Lancet 335:147–149
Verge CF, Stenger D, Bonifacio E et al (1998) Combined use of autoantibodies (IA-2 autoantibody, GAD autoantibody, insulin autoantibody, cytoplasmic islet cell antibodies) in type 1 diabetes: combinatorial islet autoantibody workshop. Diabetes 47:1857–1866
UKPDS Group (1994) UK Prospective Diabetes Study XI: biochemical risk factors in type 2 diabetic patients at diagnosis compared with age-matched normal subjects. Diabet Med 11:534–544
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Levy J, Matthews D, Hermans M (1998) Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 21:2191–2192
UKPDS Group (1999) UKPDS 43. Genetic heterogeneity of autoimmune diabetes: age of presentation in adults is influenced by HLA DRB1 and DQB1 genotypes. Diabetologia 42:608–616
Genovese S, Bonfanti R, Bazzigaluppi E et al (1996) Association of IA2 antibodies with HLA DR4 phenotype in insulin dependent diabetes. Diabetologia 39:1223–1226
Davis TME, Wright AD, Mehta ZM et al (2004) Islet cell autoantibodies in type 2 diabetes: prevalence and relationship with metabolic control. Diabetologia DOI 10.1007/s00125-005-1690-x
Mire-Sluis AR, Gaines Das R, Lermark A (2000) The world health organization international collaborative study for islet cell antibodies. Diabetologia 43:1282–1292
Zimmet PZ (1999) Diabetes epidemiology as a trigger to diabetes research. Diabetologia 42:499–518
Wiltshire S, Hattersley A, Hitman G et al (2001) A genomewide scan for loci predisposing to type 2 diabetes in a U.K. population (the Diabetes UK Warren 2 Repository): analysis of 573 pedigree provides independent replication of a susceptibility locus on chromosome 1q. Am J Hum Genet 69:553–569
UKPDS Group (1998) Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352:837–853
Acknowledgements
The cooperation of the patients and many NHS and non-NHS staff at the centres is much appreciated. The major grants for this study were from the UK Medical Research Council, British Diabetic Association, The British Heart Foundation, The UK Department of Health, The Italian Ministry of Health, The National Eye Institute and The National Institute of Digestive, Diabetes and Kidney Disease in the National Institutes of Health USA, Novo-Nordisk, Bayer, Bristol Myers Squibb, Hoechst, Lilly, Lipha and Farmitalia Carlo Erba. We thank Dr. Virginia Horton for the HLA assay results. Other funding companies and agencies, the supervising committees, and all participating staff are listed in an earlier paper [23].
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00125-005-1808-1
Rights and permissions
About this article
Cite this article
Bottazzo, G.F., Bosi, E., Cull, C.A. et al. IA-2 antibody prevalence and risk assessment of early insulin requirement in subjects presenting with type 2 diabetes (UKPDS 71). Diabetologia 48, 703–708 (2005). https://doi.org/10.1007/s00125-005-1691-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1691-9