Abstract
Aims/hypothesis
Gestational diabetes mellitus (GDM) and type 2 diabetes share a common pathophysiological background, including beta cell dysfunction and insulin resistance. In addition, women with GDM are at increased risk of developing type 2 diabetes later in life. Our aim was to investigate whether, like type 2 diabetes, GDM has a genetic predisposition by studying five common polymorphisms in four candidate genes that have previously been associated with type 2 diabetes.
Materials and methods
We studied 1,777 unrelated Scandinavian women (588 with GDM and 1,189 pregnant non-diabetic controls) for polymorphisms in the genes encoding potassium inwardly rectifying channel subfamily J, member 11 (KCNJ11 E23K), insulin receptor substrate 1 (IRS1 G972R), uncoupling protein 2 (UCP2 −866G→A) and calpain 10 (CAPN10 SNP43 and SNP44).
Results
The EE, EK and KK genotype frequencies of the KCNJ11 E23K polymorphism differed significantly between GDM and control women (31.5, 52.7 and 15.8% vs 37.3, 48.8 and 13.9%, respectively; p=0.050). In addition, the frequency of the K allele was increased in women with GDM (odds ratio [OR]=1.17, 95% CI 1.02−1.35; p=0.027), and this effect was greater under a dominant model (KK/EK vs EE) (OR=1.3, 95% CI 1.05−1.60; p=0.016). Analysis of the IRS1 G972R polymorphism showed that RR homozygosity was found exclusively in women with GDM (91.0, 8.3 and 0.7% vs 90.7, 9.3 and 0.0% for GG, GR and RR genotypes, respectively; p=0.014). The genotype and allele frequencies of the other polymorphisms studied were not statistically different between the GDM and control women.
Conclusions/interpretation
The E23K polymorphism of KCNJ11 seems to predispose to GDM in Scandinavian women.
Similar content being viewed by others
Introduction
Gestational diabetes mellitus (GDM) is defined as glucose intolerance that is first diagnosed during pregnancy [1]. It complicates about 2% of pregnancies in Sweden [2]. However, the prevalence varies between populations [3]. GDM results when pancreatic beta cells fail to compensate for the increased insulin resistance during pregnancy [4, 5]. However, the degree of beta cell dysfunction seems to be the predominant determinant of who will develop GDM [6]. In support of this, several studies have demonstrated that insulin secretion was substantially reduced in women with NGT and a history of GDM compared with controls after pregnancy [7, 8]. In addition, impaired insulin secretion as well as a history of GDM have been shown to predict future type 2 diabetes [9, 10]. Epidemiological studies have shown that beta cell dysfunction and insulin resistance are the main determinants of type 2 diabetes [11, 12]. Furthermore, both type 2 diabetes and GDM may share other risk factors and the same genetic susceptibility [13]. Also, women with a family history of type 2 diabetes are at increased risk of developing GDM [14].
Type 2 diabetes is considered a paradigm for a multifactorial polygenic disease where common variants in several genes interact with environmental factors to cause the disease [11, 15]. We have originally shown that the Ala allele of the peroxisome proliferator activated receptor gamma (PPARG Pro12Ala) polymorphism has been associated with reduced risk of type 2 diabetes [16]. In addition, we and others have reported association between the E23K polymorphism of the potassium inwardly rectifying channel subfamily J, member 11 (KCNJ11) gene and increased risk of type 2 diabetes [15, 17]. Although the G972R polymorphism of the insulin receptor substrate 1 (IRS1) gene has been associated with type 2 diabetes in several studies [15], no association was found in a recent large study [18]. Variations in the calpain 10 (CAPN10) gene have also been associated with type 2 diabetes [15]. A promoter polymorphism (–866G→A) in the uncoupling protein 2 (UCP2) gene was originally associated with reduced risk of obesity [19] as well as with reduced [20, 21] or increased [22] risk of type 2 diabetes.
Genetic predisposition to GDM has been reported for variations in the insulin receptor (INSR), insulin-like growth factor 2 (IGF2), β3-adrenergic receptor (ADRB3), sulphonylurea receptor 1 (ABCC8), CAPN10 and mannose-binding lectin (MBL2) genes [23–27], whereas no associations were found for the PPARG Pro12Ala polymorphism or insulin gene variable number of tandem repeats (INS VNTR) [28]. Also, an association with the ADRB3 W64R variant could not be replicated in subsequent studies [29, 30]. However, this might be due to lack of power, given the small effect size of most common variants, or due to ethnic heterogeneity between different populations.
There are few data on the role of the KCNJ11 E23K, IRS1 G972R, UCP2 −866G→A and CAPN10 (SNP43 and SNP44) variants in the risk of GDM. Therefore, in the present study we investigated whether GDM has a genetic predisposition similar to that of type 2 diabetes by genotyping these variants in a case–control study of 1,777 pregnant Scandinavian women, 33.1% of whom had GDM.
Subjects and methods
Study population
In southern Sweden (Skåne), all pregnant women are routinely offered a 75-g OGTT at 27–28 weeks of pregnancy. Women at high risk (previous GDM or a family history of diabetes) are also offered a 75-g OGTT at 12–13 weeks. The tests are performed in the local antenatal care clinics, using HemoCue devices (HemoCue, Ängelholm, Sweden) for capillary whole-blood analysis. GDM is defined as a 2-h capillary glucose concentration (double test) of at least 9 mmol/l according to the proposal by the European Diabetic Pregnancy Study Group [31].
We studied 1,777 unrelated Scandinavian women (588 women with GDM and 1,189 non-diabetic pregnant controls). Women were recruited from two different resources. Two hundred and twenty seven women with GDM were recruited from women referred to Malmö or Lund University Hospitals during the period from March 1996 until December 2003. The other group of women with GDM (n=361) and all non-diabetic pregnant controls (n=1,189) were ascertained among women participating in the Diabetes Prediction in Skåne (DiPiS) study, which is a prospective, longitudinal study of the prediction of type 1 diabetes in all newborns in southern Sweden [32]. At delivery (for DiPiS subjects) and after oral consent, a blood sample was drawn and information obtained about possible GDM or diabetes status. When the child was 2 months old and had been entered into the population registry, the parents were invited by letter to participate with their child in the DiPiS study. If the parents agreed to do so, they gave their written consent and filled out a psychosocial and hereditary questionnaire including information about diabetes status in the family and their country of birth. Ethnicity was also determined using both surname and given name. Since the DiPiS study was not restricted to Swedish subjects but included immigrants as well, we chose only women with a Scandinavian background for the present study. Most of the Scandinavian women were of Swedish origin and a few were of Danish, Norwegian or Finnish origin. Informed oral and/or written voluntary consent was obtained from all study subjects. The study was approved by the ethics committee of Lund University.
Genetic analyses
DNA extraction
Total DNA was isolated from peripheral blood lymphocytes or blood samples were collected as dried blood spots (DBS) on Schleicher and Schuell Grade 2992 filters (Schleicher and Schuell, Dassel, Germany) and punch-outs in 96-well plates were soaked in PCR amplification buffer.
Genotyping using DNA
When peripheral blood DNA was available from the subjects, genotyping of all single nucleotide polymorphisms (SNPs) was carried out using a TaqMan allelic discrimination assay. The assay was carried out using an ABI Prism 7900 Sequence Detection System (Applied Biosystems, Foster City, CA, USA) in a reaction volume of 5 μl, according to the manufacturer's instructions. Primers and probes were designed using Assays-by-Design (Applied Biosystems). The primers and probes used are listed in electronic supplementary material (ESM) Table S1.
Genotyping using DBS
When DBS were available from the subjects, SNP genotyping was carried out using PCR-RFLP, SNaPshot or TaqMan allelic discrimination assay.
The polymorphisms KCNJ11 E23K (rs5219), UCP2 −866G→A (rs659366) and IRS1 G972R (rs1801278) were genotyped using PCR-RFLP or TaqMan allelic discrimination assay (see below). The primers used for template PCR amplification are listed in ESM Table S2. The template PCR was performed with an initial two cycles at 4°C for 30 s followed by 98°C for 3 min, followed by holding at 80°C while the PCR mix was added. Then the PCR programme was continued with an initial denaturation (94°C for 5 min), followed by 45 cycles of denaturation (94°C for 30 s), annealing (30 s) and extension (72°C for 30 s), followed by final extension (72°C for 10 min). PCR amplification was carried out with 3×3 mm of DBS in a total volume of 40 μl containing 1× Pharmacia Amersham buffer (Amersham Pharmacia Biotech, Uppsala, Sweden), 4 nmol each dNTP (MBI Fermentas, St Leon-Rot, Germany), 20 pmol of each primer, 20 μmol Betaine (Sigma-Aldrich, Stockholm, Sweden) and 1.5 U Taq polymerase (New England Biolabs, Beverly, MA, USA). The following restriction enzymes were used to digest the PCR products, with name, origin, incubation conditions and agarose gel concentrations in parentheses: KCNJ11 E23K (BanII; New England Biolabs; 37°C for 4 h; 3.5% agarose gel), UCP2 −866G→A (MluI; MBI Fermentas; 37°C for 4 h; 3% agarose gel) and IRS1 G972R (BstNI; New England Biolabs; 60°C for 2 h; 4.5% agarose gel). PCR products were separated on agarose gel (SeaKem, Rockland, ME, USA) and stained with ethidium bromide to visualise the fragments.
CAPN10 SNP43 (rs3792267) and SNP44 (rs2975760) were genotyped using the SNaPshot assay with an ABI Prism 3100 Sequence Detection System according to the manufacturer's instructions or using the TaqMan allelic discrimination assay (see below). The template PCR was carried out as described above (see description of PCR-RFLP above) and followed by primer extension. The template PCR primers are listed in ESM Table S2. The primers used for primer extension were: CAPN10 SNP43 5′-GGCTTAGCCTCACCTTCAAA and SNP44 5'-GACTGAGGGCGCTCACGCTTGCTG.
The majority of the samples (n=949) were genotyped using TaqMan allelic discrimination assay for all the SNPs. Initially, a template PCR was carried out as described above (see description of PCR-RFLP above) using primers listed in ESM Table S2. The template PCR was followed by a TaqMan allelic discrimination assay, which was carried out with 2 μl of the PCR product according to the manufacturer's instructions.
Genotyping and quality control
The genotyping success rate was 99.2% for cases (KCNJ11 E23K, 100%; UCP2 −866G→A, 98.3%; IRS1 G972R, 99.8%; CAPN10 SNP43, 98.1%; SNP44, 99.6%) and 99.3% for controls (KCNJ11 E23K, 99.2%; UCP2 −866G→A, 98.7%; IRS1 G972R, 100%; CAPN10 SNP43, 99.3%; SNP44, 99.3%). Genotyping accuracy, as determined by regenotyping a random 1124 (12.6%) duplicates for all SNPs [KCNJ11 E23K, 170 (9.6%); UCP2 −866G→A, 212 (11.9%); IRS1 G972R, 176 (9.9%); CAPN10 SNP43, 297 (16.7%); SNP44, 269 (15.1%)], was 99.82%. In addition, 38 (6.5%) of women with GDM had both peripheral blood DNA and DBS and their genotype results were compared to assess the concordance between the different genotyping methods; we found no discrepancies. For all SNPs, both GDM and control groups were in Hardy–Weinberg equilibrium (χ 2 test, p>0.05), apart from the control group for the UCP2 −866G→A polymorphism, which showed mild deviation from equilibrium (p=0.029). Our quality control measures suggest that the deviation is due to chance variation rather than genotyping error.
Statistical analyses
Significance of the difference in age (mean±SEM) between GDM and control groups was tested by ANOVA using the Number Cruncher Statistical Systems (NCSS, Kaysville, UT, USA). The χ 2 or Fisher's exact test was used to compare group frequencies. Odds ratios (ORs) and 95% CIs were obtained from logistic regression analysis. The significance of difference in allele frequencies of the KCNJ11 E23K polymorphism between GDM and controls was also tested by 1,000 permutations. Two-sided p values equal to or less than 0.05 were considered statistically significant.
Power calculations were performed using the Genetic Power Calculator (available at http://ibgwww.colorado.edu/~pshaun/gpc/) [33]. Our power estimates have shown that, under a multiplicative model, the present study with a sample size of 588 cases and 1,189 controls has 80% power to detect an effect size of 1.23 (as measured in terms of genotypic relative risk) when the frequency of the predisposing allele equals to 30%, with a 5% type 1 error rate.
Results
Table 1 shows some phenotypic characteristics of the study subjects. Women with GDM were slightly older than non-diabetic control women (32.2±0.2 vs 30.5±0.1 years, p<0.0001) and gained more weight (5–10 kg) during pregnancy (31 vs 19.1%, p=0.0001). The genotype and allele frequency distributions of all polymorphisms are presented in Table 2.
KCNJ11 E23K
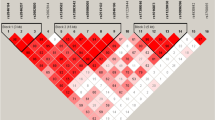
The EE, EK and KK genotype frequencies of the KCNJ11 E23K polymorphism differed significantly between GDM and control women (31.5, 52.7 and 15.8% vs 37.3, 48.8 and 13.9%, respectively; p=0.050). In addition, the K allele was increased in women with GDM (OR 1.17, 95% CI 1.02−1.35; p=0.027) and the effect was greater under a dominant model (KK/EK vs EE) (OR 1.3, 95% CI 1.05−1.60; p=0.016) (Fig. 1). The association became slightly stronger when women who were positive for GAD65Ab, IA–2Ab or both (n=21; data were not available for all subjects) or when women with GDM who had low fasting C-peptide levels (<0.3 nmol/l) (n=15; data were not available for all subjects) were excluded (Table 3). To verify the results obtained with the χ 2 test (in an exact manner), we further analysed differences in allele frequency between cases and controls using 1,000 permutations and the empirical two-tailed p value was the same as that found with the χ 2 test.
IRS1 G972R
RR homozygosity of the IRS1 G972R polymorphism was found exclusively in women with GDM (91.0, 8.3 and 0.7% vs 90.7, 9.3 and 0.0% for GG, GR and RR genotypes, respectively; p=0.014), and this was statistically significant under a recessive model (RR vs GR/GG) (0.7 vs 0.0%; p=0.011). However, the R972 allele frequency was similar in the two groups (OR 1.04, 95% CI 0.75–1.44; p=0.80).
UCP2 −866G→A
There was no significant difference in genotype frequencies of the AA, GA and GG genotypes of the UCP2 −866G→A polymorphism between GDM and control women (15.0, 46.4 and 38.6% vs 13.9, 51.7 and 34.4% respectively; p=0.11). Also, the allele frequencies were similar in the two groups (OR 1.07, 95% CI 0.92−1.23; p=0.38).
CAPN10 SNP43 and SNP44
To test for linkage disequilibrium between SNP43 and SNP44, we calculated both pairwise linkage disequilibrium measures (D′ and r 2). The D′ was 1.0 with high LOD (log of the odds) score values in cases (D′=1.0; CI 0.9–1.0; LOD=17.4) and controls (D′=1.0; CI 0.94–1.0; LOD=33.3), while the r 2 was 0.09 in both groups. Both SNPs were in Hardy–Weinberg equilibrium (p>0.4) for GDM and controls. There was no significant difference in the frequencies of the GG, GA and AA genotypes of SNP43 between GDM and controls (52.9, 38.1 and 9.0% vs 52.5, 40.3 and 7.2%, respectively; p=0.34) or in the allele frequencies of this SNP (OR 0.96, 95% CI 0.82–1.13; p=0.65). Neither was there any significant difference in the CC, TC and TT genotypes of SNP44 between women with GDM and control women (2.9, 30.2 and 66.9% vs 3.6, 29.7 and 66.7%, respectively; p=0.71) or in the allele frequencies (OR 0.97, 95% CI 0.81–1.16; p=0.71).
Discussion
To our knowledge, this is the largest study evaluating the role of common variants in genes predisposing for type 2 diabetes for their putative role in GDM.
KCNJ11 E23K
The key finding of the present study is the modest association between the K allele of the E23K polymorphism in KCNJ11 and GDM. This is in line with the dominating role of beta cell dysfunction in GDM [5–9]. In vitro, the E23K variant leads to a modestly overactive pancreatic beta cell ATP-sensitive K+ (KATP) channel subunit (Kir6.2) with decreased sensitivity to ATP, resulting in decreased insulin release [34]. We have previously shown that the E23K variant in KCNJ11 is associated with decreased insulin secretion in glucose-tolerant subjects [17]. Some caution is still warranted in the interpretation of the data. We did not correct for multiple comparisons, as we primarily tested the hypothesis that a polymorphism increasing susceptibility to type 2 diabetes would also increase susceptibility to GDM.
IRS1 G972R
IRS1 is a major substrate for the insulin receptor and is present in insulin-sensitive tissues [35]. The G972R polymorphism of IRS1, which is located between two potential tyrosine phosphorylation sites involved in binding of the p85 subunit of PI-3 kinase, has previously been associated with type 2 diabetes [15], although we could not replicate this finding in our recent large study of 9,000 individuals [18], which is a common problem in genetic association studies [36]. The G972R polymorphism has also been associated with impaired beta cell function in NGT subjects as well as with reduced insulin content and impaired insulin secretion in isolated human islets [37, 38]. Our finding that homozygosity for the G972R polymorphism was found only in women with GDM might indicate an increased risk for GDM in Scandinavian women. This is consistent with a report on a healthy man homozygous for the R allele, who showed 22% reduction of fasting insulin and 48% reduction of C-peptide values as well as ~25% reduction in acute responses of insulin and C-peptide to intravenous glucose compared with carriers of the wild-type allele [39]. Of note, the IRS1 protein level is reduced in adipose tissue of obese women with GDM [40].
UCP2 −866G→A
UCP2 is a member of the mitochondrial inner membrane carrier family that is expressed in a number of tissues and cell types, including the pancreatic islets [41]. Increased expression of UCP2 in pancreatic islets is associated with increased uncoupling, decreased formation of ATP and reduced insulin secretion [42]. The A allele of the common (−866G→A) polymorphism in the promoter of UCP2 has originally been associated with reduced risk of obesity [19]. Subsequently, a study by Wang et al. has shown association of the G allele with increased risk of type 2 diabetes (OR=1.43) in individuals of Northern European ancestry [20]. This was supported in the same study by the finding that the G allele was associated with decreased insulin secretion adjusted for the degree of insulin resistance (i.e. the disposition index) in non-diabetic individuals [20]. Another study has also shown association of the A allele with decreased risk of type 2 diabetes in Caucasians from Italy [21]. On the contrary, the AA genotype conferred an increased risk of type 2 diabetes (OR=1.84) in Italian women [22]. In line with that study, Sesti et al. found that the A allele was associated with decreased glucose-stimulated insulin secretion in subjects with NGT as well as in human islets [43]. Here, we could not find any association between the −866G→A polymorphism and GDM in Scandinavian women despite the fact that our study had 99% power to detect the OR reported for the AA genotype in Italian women with type 2 diabetes [22], or for the G allele reported by Wang et al. [20], as well as for the AA genotype reported in Caucasians [21].
CAPN10 SNP43 and SNP44
In keeping with previous results from our laboratory, SNP43 and SNP44 were in linkage disequilibrium [44]. Whereas D′ reflects recombination events between two SNPs, r 2 reflects the absolute redundancy between them. The difference we observed between D′ and r 2 occurs mainly because SNP44 arose on the same haplotype more rarely than SNP43. CAPN10 is a cysteine protease with the gene located on chromosome 2q37 [45]. It is widely expressed in different tissues, including the pancreatic islets [45, 46]. Calpain inhibitors have been shown to increase insulin secretion by accelerating exocytosis of insulin granules in mouse pancreatic islets [47]. In addition, an isoform of CAPN10 that is a Ca2+ sensor has recently been shown to trigger exocytosis in pancreatic beta cells [46]. The GG genotype of the SNP43 has been associated with reduced CAPN10 mRNA expression in skeletal muscle and subcutaneous adipose tissue [48, 49]. Moreover, it has been associated with increased insulin secretion [50], insulin resistance [44] and a decreased rate of glucose oxidation [48]. Consistent with the findings in the small study by Leipold et al. for SNP43, we did not observe any significant differences in allele or genotype frequencies between GDM and controls [26]. However, these authors reported association with SNP63 as well as a haplotype combination of SNP43, 19 and 63 (121/221) [26], but no data were available on the degree of linkage disequilibrium between these SNPs. Of note, SNP63 has been shown to be in tight linkage disequilibrium with SNP43 and SNP44 in Scandinavians [44].
Given the fact that GDM and type 2 diabetes have beta cell dysfunction in common, we tested the hypothesis that common variants in candidate genes that have been associated with type 2 diabetes, particularly with beta cell dysfunction, might also be operative in GDM. We conclude that the K allele of the E23K polymorphism in KCNJ11 seems to predispose to GDM in Scandinavian women. This is compatible with its effect on insulin secretion and the crucial role of impaired beta cell function in the pathogenesis of GDM.
Abbreviations
- CAPN10 :
-
gene encoding calpain 10
- DBS:
-
dried blood spots
- ESM:
-
electronic supplementary material
- GDM:
-
gestational diabetes mellitus
- IRS1 :
-
gene encoding insulin receptor substrate 1
- KCNJ11 :
-
gene encoding potassium inwardly-rectifying channel, subfamily J, member 11
- OR:
-
odds ratio
- SNP:
-
single-nucleotide polymorphism
- UCP2 :
-
gene encoding uncoupling protein 2
References
Metzger BE, Coustan DR, the Organizing Committee (1998) Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 21 (Suppl 2):B161–B167
Aberg A, Rydhstroem H, Frid A (2001) Impaired glucose tolerance associated with adverse pregnancy outcome: a population-based study in southern Sweden. Am J Obstet Gynecol 184:77–83
King H (1998) Epidemiology of glucose intolerance and gestational diabetes in women of childbearing age. Diabetes Care 21 (Suppl 2):B9–B13
Catalano PM, Huston L, Amini SB, Kalhan SC (1999) Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus. Am J Obstet Gynecol 180:903–916
Xiang AH, Peters RK, Trigo E, Kjos SL, Lee WP, Buchanan TA (1999) Multiple metabolic defects during late pregnancy in women at high risk for type 2 diabetes. Diabetes 48:848–854
Buchanan TA, Metzger BE, Freinkel N, Bergman RN (1990) Insulin sensitivity and B-cell responsiveness to glucose during late pregnancy in lean and moderately obese women with normal glucose tolerance or mild gestational diabetes. Am J Obstet Gynecol 162:1008–1014
Ryan EA, Imes S, Liu D et al (1995) Defects in insulin secretion and action in women with a history of gestational diabetes. Diabetes 44:506–512
Osei K, Gaillard TR, Schuster DP (1998) History of gestational diabetes leads to distinct metabolic alterations in nondiabetic African-American women with a parental history of type 2 diabetes. Diabetes Care 21:1250–1257
Buchanan TA, Xiang AH, Kjos SL, Trigo E, Lee WP, Peters RK (1999) Antepartum predictors of the development of type 2 diabetes in Latino women 11–26 months after pregnancies complicated by gestational diabetes. Diabetes 48:2430–2436
Kim C, Newton KM, Knopp RH (2002) Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 25:1862–1868
Groop L (2000) Pathogenesis of type 2 diabetes: the relative contribution of insulin resistance and impaired insulin secretion. Int J Clin Pract 113 (Suppl 1):3–13
Lyssenko V, Almgren P, Anevski D et al (2005) Predictors of and longitudinal changes in insulin sensitivity and secretion preceding onset of type 2 diabetes. Diabetes 54:166–174
Ben-Haroush A, Yogev Y, Hod M (2004) Epidemiology of gestational diabetes mellitus and its association with Type 2 diabetes. Diabet Med 21:103–113
Williams MA, Qiu C, Dempsey JC, Luthy DA (2003) Familial aggregation of type 2 diabetes and chronic hypertension in women with gestational diabetes mellitus. J Reprod Med 48:955–962
Parikh H, Groop L (2004) Candidate genes for type 2 diabetes. Rev Endocr Metab Disord 5:151–176
Altshuler D, Hirschhorn JN, Klannemark M et al (2000) The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet 26:76–80
Florez JC, Burtt N, de Bakker PI et al (2004) Haplotype structure and genotype–phenotype correlations of the sulfonylurea receptor and the islet ATP-sensitive potassium channel gene region. Diabetes 53:1360–1368
Florez JC, Sjogren M, Burtt N et al (2004) Association testing in 9,000 people fails to confirm the association of the insulin receptor substrate-1 G972R polymorphism with type 2 diabetes. Diabetes 53:3313–3318
Esterbauer H, Schneitler C, Oberkofler H et al (2001) A common polymorphism in the promoter of UCP2 is associated with decreased risk of obesity in middle-aged humans. Nat Genet 28:178–183
Wang H, Chu WS, Lu T, Hasstedt SJ, Kern PA, Elbein SC (2004) Uncoupling protein-2 polymorphisms in type 2 diabetes, obesity, and insulin secretion. Am J Physiol Endocrinol Metab 286:E1–E7
Bulotta A, Ludovico O, Coco A et al (2005) The common −866G→A polymorphism in the promoter region of the UCP-2 gene is associated with reduced risk of type 2 diabetes in Caucasians from Italy. J Clin Endocrinol Metab 90:1176–1180
D'Adamo M, Perego L, Cardellini M et al (2004) The −866A/A genotype in the promoter of the human uncoupling protein 2 gene is associated with insulin resistance and increased risk of type 2 diabetes. Diabetes 53:1905–1910
Ober C, Xiang KS, Thisted RA, Indovina KA, Wason CJ, Dooley S (1989) Increased risk for gestational diabetes mellitus associated with insulin receptor and insulin-like growth factor II restriction fragment length polymorphisms. Genet Epidemiol 6:559–569
Festa A, Krugluger W, Shnawa N, Hopmeier P, Haffner SM, Schernthaner G (1999) Trp64Arg polymorphism of the beta3-adrenergic receptor gene in pregnancy: association with mild gestational diabetes mellitus. J Clin Endocrinol Metab 84:1695–1699
Rissanen J, Markkanen A, Karkkainen P et al (2000) Sulfonylurea receptor 1 gene variants are associated with gestational diabetes and type 2 diabetes but not with altered secretion of insulin. Diabetes Care 23:70–73
Leipold H, Knofler M, Gruber C, Haslinger P, Bancher-Todesca D, Worda C (2004) Calpain-10 haplotype combination and association with gestational diabetes mellitus. Obstet Gynecol 103:1235–1240
Megia A, Gallart L, Fernandez-Real JM et al (2004) Mannose-binding lectin gene polymorphisms are associated with gestational diabetes mellitus. J Clin Endocrinol Metab 89:5081–5087
Shaat N, Ekelund M, Lernmark A et al (2004) Genotypic and phenotypic differences between Arabian and Scandinavian women with gestational diabetes mellitus. Diabetologia 47:878–884
Alevizaki M, Thalassinou L, Grigorakis SI et al (2000) Study of the Trp64Arg polymorphism of the beta3-adrenergic receptor in Greek women with gestational diabetes. Diabetes Care 23:1079–1083
Tsai PJ, Ho SC, Tsai LP et al (2004) Lack of relationship between beta3-adrenergic receptor gene polymorphism and gestational diabetes mellitus in a Taiwanese population. Metabolism 53:1136–1139
Lind T, Phillips PR (1991) Influence of pregnancy on the 75-g OGTT. A prospective multicenter study. The Diabetic Pregnancy Study Group of the European Association for the Study of Diabetes. Diabetes 40 (Suppl 2):8–13
Lernmark B, Elding-Larsson H, Hansson G, Lindberg B, Lynch K, Sjoblad S (2004) Parent responses to participation in genetic screening for diabetes risk. Pediatr Diabetes 5:174–181
Purcell S, Cherny SS, Sham PC (2003) Genetic Power Calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics 19:149–150. Available from http://ibgwww.colorado.edu/~pshaun/gpc/, accessed 10 August 2005
Schwanstecher C, Meyer U, Schwanstecher M (2002) K(IR)6.2 polymorphism predisposes to type 2 diabetes by inducing overactivity of pancreatic beta-cell ATP-sensitive K(+) channels. Diabetes 51:875–879
Hirayama I, Tamemoto H, Yokota H et al (1999) Insulin receptor-related receptor is expressed in pancreatic beta-cells and stimulates tyrosine phosphorylation of insulin receptor substrate-1 and -2. Diabetes 48:1237–1244
Hirschhorn JN, Lohmueller K, Byrne E, Hirschhorn K (2002) A comprehensive review of genetic association studies. Genet Med 4:45–61
Stumvoll M, Fritsche A, Volk A et al (2001) The Gly972Arg polymorphism in the insulin receptor substrate-1 gene contributes to the variation in insulin secretion in normal glucose-tolerant humans. Diabetes 50:882–885
Marchetti P, Lupi R, Federici M et al (2002) Insulin secretory function is impaired in isolated human islets carrying the Gly(972)→Arg IRS-1 polymorphism. Diabetes 51:1419–1424
Clausen JO, Hansen T, Bjorbaek C et al (1995) Insulin resistance: interactions between obesity and a common variant of insulin receptor substrate-1. Lancet 346:397–402
Catalano PM, Nizielski SE, Shao J, Preston L, Qiao L, Friedman JE (2002) Downregulated IRS-1 and PPARgamma in obese women with gestational diabetes: relationship to FFA during pregnancy. Am J Physiol Endocrinol Metab 282:E522–E533
Zhang CY, Baffy G, Perret P et al (2001) Uncoupling protein-2 negatively regulates insulin secretion and is a major link between obesity, beta cell dysfunction, and type 2 diabetes. Cell 105:745–755
Chan CB, De Leo D, Joseph JW et al (2001) Increased uncoupling protein-2 levels in beta-cells are associated with impaired glucose-stimulated insulin secretion: mechanism of action. Diabetes 50:1302–1310
Sesti G, Cardellini M, Marini MA et al (2003) A common polymorphism in the promoter of UCP2 contributes to the variation in insulin secretion in glucose-tolerant subjects. Diabetes 52:1280–1283
Orho-Melander M, Klannemark M, Svensson MK, Ridderstrale M, Lindgren CM, Groop L (2002) Variants in the calpain-10 gene predispose to insulin resistance and elevated free fatty acid levels. Diabetes 51:2658–2664
Horikawa Y, Oda N, Cox NJ et al (2000) Genetic variation in the gene encoding calpain-10 is associated with type 2 diabetes mellitus. Nat Genet 26:163–175
Marshall C, Hitman GA, Partridge CJ et al (2005) Evidence that an isoform of calpain-10 is a regulator of exocytosis in pancreatic beta-cells. Mol Endocrinol 19:213–224
Sreenan SK, Zhou YP, Otani K et al (2001) Calpains play a role in insulin secretion and action. Diabetes 50:2013–2020
Baier LJ, Permana PA, Yang X et al (2000) A calpain-10 gene polymorphism is associated with reduced muscle mRNA levels and insulin resistance. J Clin Invest 106:R69–R73
Carlsson E, Fredriksson J, Groop L, Ridderstrale M (2004) Variation in the calpain-10 gene is associated with elevated triglyceride levels and reduced adipose tissue messenger ribonucleic acid expression in obese Swedish subjects. J Clin Endocrinol Metab 89:3601–3605
Stumvoll M, Fritsche A, Madaus A et al (2001) Functional significance of the UCSNP-43 polymorphism in the CAPN10 gene for proinsulin processing and insulin secretion in nondiabetic Germans. Diabetes 50:2161–2163
Acknowledgements
This work was supported by grants from the JDF-Wallenberg Foundation, Swedish Medical Research Council, the European Commission, Lundberg Foundation, Novo Nordisk Foundation and grants to the Diabetes Prediction in Skåne (DiPiS) study. We thank all the subjects for their participation, and the DiPiS research group. We are indebted to M. Svensson, A. Berglund and A. Nilsson for excellent technical assistance, and to K. Lynch for helping with data analysis.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Shaat, N., Ekelund, M., Lernmark, Å. et al. Association of the E23K polymorphism in the KCNJ11 gene with gestational diabetes mellitus. Diabetologia 48, 2544–2551 (2005). https://doi.org/10.1007/s00125-005-0035-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-0035-0