Abstract
Aims/hypothesis
The aim of this prospective study was to investigate predictors of deteriorating glucose tolerance in subjects of British extraction.
Methods
A total of 156 non-diabetic subjects (86 with a family history of type 2 diabetes) underwent a 75-g OGTT and anthropometric assessment at baseline and 5 years later. Pancreatic beta cell function and whole-body insulin sensitivity were studied by model assessment. Subjects were classified as progressors if glucose tolerance moved one or more steps from normal, impaired fasting glucose, impaired glucose tolerance and diabetes over the follow-up period.
Results
At baseline, the progressors (n=22) had increased adiposity and a higher proportion of familial diabetes and abnormal glucose tolerance than non-progressors. Baseline pancreatic beta cell sensitivity to changes in glucose (p<0.02) and whole-body insulin sensitivity (p<0.0001) were decreased in the progressors. Logistic regression revealed that baseline and follow-up changes in beta cell glucose sensitivity and insulin sensitivity, rather than the classical clinical predictors (adiposity, familial diabetes and glucose levels), were the key independent predictors of progression (explaining over 50% of the progression).
Conclusions/interpretation
Impaired pancreatic beta cell glucose sensing and whole-body insulin sensitivity predict progression to hyperglycaemia. Strikingly, these pathophysiological changes override the importance of the clinical risk factors and highlight potential metabolic targets for prevention strategies.
Similar content being viewed by others
Introduction
We are in the midst of a world-wide explosion in the prevalence of type 2 diabetes [1] that is the result of life-style changes on a background of genetic susceptibility. A major concern is that this will translate into a future burden of diabetes-related complications and premature mortality [1]. Understanding the pathogenesis of type 2 diabetes will facilitate the development of future effective strategies for prevention.
A number of longitudinal studies have been conducted among different ethnic groups to identify predisposing factors. Insulin insensitivity, frequently linked to increased total and central adiposity, is a key predisposing factor [2, 3]. However, impaired pancreatic beta cell function is an essential element in the development of abnormal glucose tolerance. Indeed, altered beta cell function is a known predisposing factor for type 2 diabetes [4–8], while other studies have found that insulin insensitivity and abnormal beta cell function are independent predictors [9–11]. A major problem until now has been the lack of detailed information about the specific abnormalities of beta cell function that predispose to diabetes. This is in part because the methods required to investigate beta cell function—such as the measurement of insulin pulsatility, beta cell glucose sensitivity (sensitivity to changes in blood glucose levels) and the response to different secretagogues—invariably involve complicated and time-consuming protocols. As a consequence, they are difficult to apply across the large number of individuals generally needed for prospective studies of predictors of diabetes.
What is needed, therefore, are alternative methods for assessing beta cell function that on the one hand are experimentally simple, but on the other also look at different aspects of beta cell function, so that the best predictors of progression can be identified. This in turn will inform the development of targeted therapies to prevent progression. We have recently developed a mathematical model that uses data from a standard oral glucose tolerance test to measure insulin secretion rates, beta cell glucose sensitivity and beta cell potentiation (effects of glucose itself and non-glucose secretagogues to magnify the response to glucose), together with an estimate of whole-body insulin sensitivity [12–14]. In this study we used this model to identify predictors of deterioration in glucose tolerance in a longitudinal study of non-diabetic subjects of British extraction with or without a family history of type 2 diabetes.
Subjects and methods
Subjects
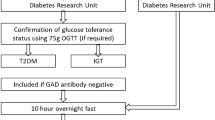
Non-diabetic subjects of British extraction were recruited and underwent investigation at baseline (1991–1993) and 5 years later (1996–1998). Of the original 180 subjects, 156 had a full data set available for analysis. Of these 156 subjects, 92 had a first-degree relative with type 2 diabetes and the remainder had no family history of diabetes. All subjects were residents of Newcastle and North Tyneside. Informed written consent was obtained from all subjects and the study was approved by the Newcastle and North Tyneside Health Authority and University of Newcastle upon Tyne Joint Ethics Committee.
Study protocol
All subjects underwent the same anthropometric and metabolic investigations at baseline and approximately 5 years later. Subjects fasted for 10 h overnight, having avoided alcohol and vigorous exercise for the preceding 24 h. The following morning, an indwelling cannula was placed in an antecubital vein. Fasting samples (three samples separated by 5-min intervals) were taken, and then the subjects were given a standard 75 g oral glucose load (388 ml degassed Lucozade; Glaxo Smithkline, Brentford, UK). Further blood samples were taken 0, 10, 20, 30, 45, 60, 90 and 120 min after the oral load. Height, weight and waist and hip circumferences were measured according to the protocol of the World Health Organization (WHO) MONICA Project [15]. Blood pressure was measured according to the guidelines of the British Hypertension Society [16].
Biochemical measurements
Plasma glucose concentrations were measured using a glucose oxidase method (interassay CV 3.5%; YSI 2300 Stat Plus; Yellow Springs Instruments, Farnborough, UK). Sera for hormone determinations were separated at 4°C and stored at −40°C. Subject samples were analysed in batches to minimise interassay variation. Plasma insulin and C-peptide concentrations were determined by specific enzyme immunoassays (Dako Diagnostics, Ely, UK). For the insulin assay, the interassay CV was 4.8% at 34 pmol/l with 0.3 and 0% cross-reactivity with proinsulin and C-peptide, respectively. For the C-peptide assay, the inter-assay CV was 3.5% at 160 pmol/l, with 63 and 0% cross-reactivity with proinsulin and insulin, respectively. Assays for measurement of glucose, C-peptide and insulin were identical at baseline and follow-up, and throughout this period the assays were monitored as part of the UK National External Quality Assurance Scheme.
Data analysis
Glucose tolerance status was classified according to 2000 WHO criteria [17]. Thus, at the baseline examination subjects were classified as having NGT (fasting glucose <6.1 mmol/l, 2-h glucose <7.8 mmol/l), IGT (fasting glucose <6.1 mmol/l, 2-h glucose 7.8–11.1 mmol/l), IFG (fasting glucose 6.1–7.0 mmol/l, 2-h glucose <7.8 mmol/l), or combined IFG and IGT (IFG*IGT). Those subjects classified as having IGT had a repeat OGTT (fasting and 2-h glucose concentrations measured only) within 2–4 weeks to identify those with persistent IGT. Based on the OGTT performed at follow-up, subjects were classified as progressors if their glucose tolerance deteriorated (from a lower step to any of the higher steps in the ascending sequence NGT → IFG → IGT → IFG*IGT → diabetes) or non-progressors if their glucose tolerance status did not change or improved.
Insulin sensitivity, as an estimate from the OGTT of the glucose clearance during a euglycaemic clamp (expressed in ml per min per square metre of body surface area), was calculated from the plasma glucose and insulin values during the OGTT according to the method of Mari and colleagues [12], which has been validated against the euglycaemic insulin clamp technique. Insulin secretion rates were calculated from plasma C-peptide concentrations by deconvolution, as previously described [18]. Parameters of beta cell function were derived from mathematical analysis of plasma glucose and C-peptide concentrations during the OGTT, using a previously developed model [13, 14]. According to this method, glucose-stimulated insulin secretion [S(t)] is the sum of two components: S(t)=P(t)f(G)+S d(t). The first component, P(t)f(G), represents the dependence of insulin secretion on the absolute glucose concentration (G) at any time point. It is expressed as the product of a dose–response function, f(G), relating insulin secretion to glucose concentration, and a potentiation factor, P(t), which modulates the dose–response relationship. The potentiation factor represents a time-dependent relative augmentation of insulin secretion [14, 19] due to several factors (glucose-mediated potentiation, non-glucose secretagogues, gastrointestinal hormones and neurotransmitters). Thus, P(t) is a positive function of time and averages 1 during the experiment.
A characteristic parameter of the dose–response curve is its mean slope in the observed glucose concentration range, denoted beta cell glucose sensitivity. Glucose sensitivity represents the ability of the beta cell to respond to an increment in glucose concentration. It has been shown to have good reproducibility (24%) [13]. A characteristic parameter of the potentiation factor is the ratio between its value at the end of the OGTT (100–120 min) and its initial value (0–20 min). It has been observed that this potentiation ratio is greater than 1 in normal subjects (representing a relative increase in insulin secretion in relation to the glucose levels over the course of the OGTT), and is progressively depressed as glucose tolerance worsens [20].
The second insulin secretion component, S d(t), accounts for the observation that rapid changes in glucose concentration enhance insulin release. S d(t) is proportional to the rate of change of plasma glucose concentration during the OGTT [Sd(t) = kd dG(t)/dt for dG(t)/dt > 0, otherwise S d(t) = 0]. A characteristic parameter of this secretion component is the constant k d, termed ‘rate sensitivity’. This parameter has limited reproducibility (52%) [13].
The model parameters were estimated from glucose and C-peptide concentration by regularised least-squares analysis, as previously described [13, 14]. Regularisation involves the choice of smoothing factors that were selected to obtain glucose and C-peptide model residuals with standard deviations close to the expected measurement error (~2% for glucose and ~4% for C-peptide).
Mean plasma glucose and insulin concentrations during the OGTT were calculated by the trapezoidal rule. The insulinogenic index was calculated as the ratio of the insulin concentration increment to the glucose concentration increment at 30 min into the OGTT (ΔI 30/ΔG 30). The ability of the beta cell to compensate for the extant degree of insulin resistance was estimated by calculating the product of insulin sensitivity and the insulinogenic index, analogous to the disposition index (DI, in units of ml min−1 m−2 pmol mmol−1) proposed by Kahn and colleagues [21].
Statistical analysis
Normally distributed data are given as the mean ± SD. Non-normally distributed data are presented as the median and interquartile range (difference between 75th and 25th percentile numbers) in the tables and text, and plotted as median and SEM in the figures. Categorical variables were compared by the chi square test, continuous variables by the Mann–Whitney U test. Changes over time were analysed by analysis of covariance, with the change in parameter (value at 5 years minus baseline value) as the dependent variable, group as the independent variable, and the baseline value as a covariate. For this analysis, non-normally distributed parameters were transformed into their natural logarithms. Logistic regression was used to test for the association between predictor variables and incident abnormalities of glucose tolerance. Results are given as the odds ratio (OR) and 95% CI. A p value of <0.05 was considered statistically significant.
Results
Baseline
Table 1 summarises the baseline clinical characteristics of the subjects classified as progressors or non-progressors. There were 22 progressors in total; seven subjects each became IFG, IGT or overtly diabetic and one became IFG*IGT. The progressors and non-progressors were matched for age and sex. However, the progressors had a higher proportion of subjects with familial diabetes, a higher proportion of subjects with abnormal glucose tolerance, and had a greater BMI and WHR. Fasting and post-oral glucose load plasma glucose, but not plasma insulin, concentrations were higher in the progressors.
Table 2 summarises the measures of beta cell function and whole-body insulin sensitivity at baseline in the progressors and non-progressors. Absolute insulin secretion rates, both fasting and total, were higher, or tended to be higher, in the progressors and were associated with a decrease in whole-body insulin sensitivity compared with the non-progressors. However, beta cell glucose sensitivity and disposition index (30-min insulin response in relation to whole-body insulin sensitivity) were significantly decreased in the progressors. Neither beta cell rate sensitivity nor potentiation, nor the insulinogenic index differed between the two groups.
Changes in glucose tolerance and metabolic measures with follow-up
As predicted by the a priori classification, plasma glucose profiles were higher at 5 years compared with baseline in the progressors but not in the non-progressors (Fig. 1). Plasma insulin and C-peptide concentrations, on the other hand, were essentially superimposable at baseline and follow-up in both groups (data not shown). Table 3 summarises the changes in the key anthropometric and metabolic measurements between baseline and 5 years in the progressors and non-progressors. There was a greater increase in BMI and fasting insulin secretion, and a decrease in whole-body insulin sensitivity in the progressors. There was also a greater decrease in beta cell glucose sensitivity and disposition index in the progressors compared with the non- progressors. Figure 2 shows the stimulus–secretion dose–response curves (the slope of which is glucose sensitivity) in the two groups at baseline and follow-up: the decline in beta cell glucose sensitivity between baseline and 5 years at plasma glucose levels above 7 mmol/l was greater in the progressors than in the non-progressors.
In Fig. 3, beta cell glucose sensitivity and insulin sensitivity are plotted against each other to show that in progressors both parameters were worse at baseline and deteriorated in parallel over 5 years, while in the non-progressors they were better at baseline and remained essentially unchanged with time. Those subjects (n=8) in whom glucose tolerance improved over this period of observation tended to follow an inverse path.
Plot of beta cell glucose sensitivity vs insulin sensitivity in progressors (solid squares), non-progressors (hatched squares) and regressors (solid circles) at baseline and follow-up. Data points and bars are mean ± SE for insulin sensitivity and median ± SE for beta cell glucose sensitivity. Scatter is not indicated for the small group of regressors (n=8)
Predictors of progression
Several logistic regression models were tested to identify predictors of progression to hyperglycaemia over the follow-up period. With a model including just the clinical characteristics (sex, a 10-year difference in age, a 3-unit difference in BMI and a positive family history of type 2 diabetes), only a higher BMI (OR=1.5; CI=1.1–2.0, p<0.01) and familial diabetes (OR=3.2; CI=1.1–9.8, p<0.04) were significant independent predictors (14% of the variance explained). In a model considering only fasting or 2-h plasma glucose concentrations, a 0.2 mmol/l rise in fasting glucose conferred a risk of progression (OR=1.4; CI=1.2–1.6, p<0.001) similar to a 1 mmol/l rise in 2-h plasma glucose (OR=1.4; CI=1.1–1.9, p=0.02). When the baseline metabolic measures (i.e. baseline beta cell glucose sensitivity and baseline insulin sensitivity) were included in the analysis, each was an independent predictor of progression (together explaining 11% of the variability in progression). By then including the changes in beta cell glucose sensitivity and insulin sensitivity at follow-up in the analysis, 43% of the variability in progression could be explained (Fig. 4). When the baseline and changes in beta cell glucose sensitivity and insulin sensitivity were added to the model, the clinical characteristics (age, sex, BMI, familial diabetes and change in BMI), the disposition index and the plasma glucose levels were no longer significant independent predictors. When the analysis was restricted to those subjects classified as NGT at baseline (n=130, of whom 14 progressed to worse glucose tolerance), the pattern of results was essentially unchanged.
Multivariate prediction of hyperglycaemia in the whole cohort: dots and lines are point estimates of odds ratio and 95% confidence intervals, respectively, for baseline values and changes over time in insulin sensitivity (for each 20 ml·min−1·m−2) and beta cell glucose sensitivity (for each pmol min−1 m−2 mmol l−1)
Discussion
The present study is based on a cohort enriched with individuals at enhanced risk of incident hyperglycaemia because of a positive family history of diabetes. Numerous studies have found that individuals with a positive family history are at increased risk of developing diabetes [22–24], and show decreased insulin secretion after adjustment for whole-body insulin sensitivity in cross-sectional studies [25, 26]. In our cohort of non-diabetic subjects, there were fewer subjects with NGT in the group with familial diabetes than in the group without such a history. Over 5 years, glucose tolerance deteriorated according to the defined criteria in a total of 22 subjects, i.e. at a rate of 1.4%/year for individuals with no family history of diabetes and 4.0%/year for subjects who had a first-degree relative with diabetes (p=0.02). This underlines the increased risk of progression in those subjects with a positive family history of type 2 diabetes.
The clinical phenotype of the progressors was characterised by central obesity, slightly elevated fasting and postchallenge glucose levels, and modest whole-body insulin insensitivity. While plasma insulin concentrations, fasting or after glucose, did not clearly discriminate between progressors and non-progressors, insulin secretory rates were higher in the progressors. Nonetheless, dynamic indices of beta cell function, such as glucose sensitivity and beta cell compensation for insulin insensitivity [21], were significantly and markedly impaired (by ~25%) in the progressors. Thus, insulin hypersecretion masked the fact that the intrinsic ability of the beta cell to acutely respond to glucose was already compromised in the progressors at baseline.
These findings suggest that whole-body insulin insensitivity and beta cell dysfunction not only mark the high-risk condition of progressors but precede the actual deterioration of glucose tolerance in ‘confirmed’ individuals. Analysis of the prospective data supports this interpretation. In a multivariate model of prediction, baseline whole-body insulin insensitivity, beta cell glucose insensitivity and their changes over time were independent predictors of incident hyperglycaemia, together explaining a large proportion of the observed progression. A striking and novel finding of this study is that these pathophysiological changes totally replaced the classical clinical risk factors (such as obesity, familial diabetes and plasma glucose concentrations) as predictors of progression towards type 2 diabetes. This differs somewhat from the findings of a similar prospective study [27] in which type 2 diabetes was predicted by a combination of metabolic and classical risk factors (obesity and plasma glucose levels). However, this may be because the metabolic measures were comparatively restricted, and did not include detailed assessment of beta-cell function, such as measures of insulin secretion and glucose sensitivity.
Our results extend previous findings [9, 11] in several respects. First, whole-body insulin insensitivity, even of a mild degree and at a relatively young age, is a consistent antecedent of hyperglycaemia of any severity (ranging from IFG to overt diabetes). Second, when beta cell glucose insensitivity is measured (by modelling in our case), it proves to be a powerful determinant of glucose tolerance and an accurate predictor of its changes over time regardless of the actual amounts of insulin secreted. The disposition index assesses the adequacy of the acute insulin response to the prevailing insulin sensitivity [21]. In our cohort, the disposition index was a weak predictor of incident hyperglycaemia in univariate association (OR=1.32; CI=0.97–1.79, p=0.08) and was not an independent predictor in the multivariate model including beta-cell glucose sensitivity and insulin sensitivity. Finally, no previous study has assessed the impact of changes in different aspects of beta cell function and insulin sensitivity over time on glucose intolerance. This was made possible in our study by the use of the OGTT, i.e. a relatively simple clinical test, as the data source for modelling analysis of both beta-cell function and insulin sensitivity. It is important to emphasise that, while whole-body insulin insensitivity and beta cell glucose insensitivity were quantitatively small in our cohort, they interact with one another strongly. Thus, insulin insensitivity and its changes over time explained 40% of the progression, and beta cell glucose insensitivity and its spontaneous changes over time explained 22% of the progression, but the two together accounted for over half of the observed variability.
We accept that this study has some limitations. The cohort was comparatively small, although it is the largest prospective longitudinal study of its kind to date of a cohort of British extraction. The classification of conversion was based upon progression to a composite based upon IFG and IGT and frank type 2 diabetes. However, evidence from the Pima Indians indicates that the pathophysiology underlying the deterioration in glucose tolerance is the same whether from NGT to IGT or from IGT to type 2 diabetes [11]. Finally, the metabolic measures are generated from the modelling of data derived from a standard OGTT. However, the overall finding that measures of beta cell function and insulin sensitivity are the key determinants of deterioration of glucose tolerance is in keeping with the findings from similar longitudinal studies that have used other empirical methods to measure baseline metabolic functions. Importantly, our approach is suitable for large-scale longitudinal studies.
In conclusion, we have shown that changes in both pancreatic beta cell function and whole-body insulin sensitivity are associated with deterioration in glucose tolerance in subjects of British extraction. Preliminary evidence from this study suggests that changes in glucose sensing appear to be a key change in beta cell function. Strikingly, it is clear that the pathophysiology overrides the effects of the classical clinical risk factors (obesity, familial history and plasma glucose levels) in predicting deterioration in glucose tolerance.
Abbreviations
- OR:
-
odds ratio
- WHO:
-
World Health Organization
References
Zimmet P, Alberti KG, Shaw J (2001) Global and societal implications of the diabetes epidemic. Nature 414:782–787
Lillioja S, Mott DM, Howard BV et al (1988) Impaired glucose tolerance as a disorder of insulin action. Longitudinal and cross-sectional studies in Pima Indians. N Engl J Med 318:1217–1225
Humphriss DB, Stewart MW, Berrish TS et al (1997) Multiple metabolic abnormalities in normal glucose tolerant relatives of NIDDM families. Diabetologia 40:1185–1190
O’Rahilly SP, Nugent Z, Rudenski AS et al (1986) Beta-cell dysfunction, rather than insulin insensitivity, is the primary defect in familial type 2 diabetes. Lancet 2:360–364
Kahn SE (2001) Clinical review 135: the importance of beta-cell failure in the development and progression of type 2 diabetes. J Clin Endocrinol Metab 86:4047–4058
Gautier JF, Wilson C, Weyer C et al (2001) Low acute insulin secretory responses in adult offspring of people with early onset type 2 diabetes. Diabetes 50:1828–1833
Gerich JE (2002) Is reduced first-phase insulin release the earliest detectable abnormality in individuals destined to develop type 2 diabetes? Diabetes 51(Suppl 1)S117–S121
Mitrakou A, Kelley D, Mokan M et al (1992) Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance. N Engl J Med 326:22–29
Haffner SM, Miettinen H, Gaskill SP, Stern MP (1995) Decreased insulin secretion and increased insulin resistance are independently related to the 7-year risk of NIDDM in Mexican-Americans. Diabetes 44:1386–1391
Lillioja S, Mott DM, Spraul M et al (1993) Insulin resistance and insulin secretory dysfunction as precursors of non-insulin-dependent diabetes mellitus. Prospective studies of Pima Indians. N Engl J Med 329:1988–1992
Weyer C, Tataranni PA, Bogardus C, Pratley RE (2001) Insulin resistance and insulin secretory dysfunction are independent predictors of worsening of glucose tolerance during each stage of type 2 diabetes development. Diabetes Care 24:89–94
Mari A, Pacini G, Murphy E, Ludvik B, Nolan JJ (2001) A model-based method for assessing insulin sensitivity from the oral glucose tolerance test. Diabetes Care 24:539–548
Mari A, Schmitz O, Gastaldelli A, Oestergaard T, Nyholm B, Ferrannini E (2002) Meal and oral glucose tests for assessment of beta-cell function: modeling analysis in normal subjects. Am J Physiol Endocrinol Metab 283:E1159–E1166
Mari A, Tura A, Gastaldelli A, Ferrannini E (2002) Assessing insulin secretion by modeling in multiple-meal tests: role of potentiation. Diabetes 51(Suppl 1):S221–S226
World Health Organization (1990) WHO MONICA Project MONICA manual (Part III, Section 1 [4.6]). WHO Cardiovascular Diseases Unit, Geneva
Petrie JC OBE, Littler WA, de Swiet M, Padfield PL, Dillow MJ (1990) Recommendations on blood pressure measurement, 2nd ed. BMJ Publishing, London
World Health Organization (1999) Report of a WHO Consultation. Definition, diagnosis and classification of diabetes mellitus and its complications. World Health Organization, Geneva
Van Cauter E, Mestrez F, Sturis J, Polonsky KS (1992) Estimation of insulin secretion rates from C-peptide levels. Comparison of individual and standard kinetic parameters for C-peptide clearance. Diabetes 41:368–377
Fehmann HC, Goke R, Goke B (1995) Cell and molecular biology of the incretin hormones glucagon-like peptide-I and glucose-dependent insulin releasing polypeptide. Endocr Rev 16:390–410
Ferrannini E, Gastaldelli A, Miyazaki Y, Matsuda M, Mari A, DeFronzo RA (2005) Beta-cell function in subjects spanning the range from normal glucose tolerance to overt diabetes: a new analysis. J Clin Endocrinol Metab 90:493–500
Kahn SE, Prigeon RL, McCulloch DK et al (1993) Quantification of the relationship between insulin sensitivity and beta-cell function in human subjects. Evidence for a hyperbolic function. Diabetes 42:1663–1672
Kobberling J, Tillil H (1982) Empirical risk figures for first degree relatives of non-insulin dependent diabetics. In: Kobberling J, Tillil H, Kobberling J, Tattersall R (eds) The genetics of diabetes mellitus. Academic Press, London, pp 201–209
Knowler WC, Pettitt DJ, Savage PJ, Bennett PH (1981) Diabetes incidence in Pima indians: contributions of obesity and parental diabetes. Am J Epidemiol 113:144–156
Mitchell BD, Kammerer CM, Reinhart LJ, Stern MP (1994) NIDDM in Mexican-American families. Heterogeneity by age of onset. Diabetes Care 17:567–573
Tripathy D, Wessman Y, Gullstrom M, Tuomi T, Groop L (2003) Importance of obtaining independent measures of insulin secretion and insulin sensitivity during the same test: results with the Botnia clamp. Diabetes Care 26:1395–1401
Arslanian SA, Bacha F, Saad R, Gungor N (2005) Family history of type 2 diabetes is associated with decreased insulin sensitivity and an impaired balance between insulin sensitivity and insulin secretion in white youth. Diabetes Care 28:115–119
Bonora E, Kiechl S, Willeit J et al (2004) Population-based incidence rates and risk factors for type 2 diabetes in white individuals: the Bruneck study. Diabetes 53:1782–1789
Acknowledgements
The study was funded by the UK MRC and Diabetes UK. Thanks to Sister Jean Gerrard and her staff for technical support, and to Drs Murray Stewart and David Humphriss for their contributions to the baseline studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00125-006-0204-9
Rights and permissions
About this article
Cite this article
Walker, M., Mari, A., Jayapaul, M.K. et al. Impaired beta cell glucose sensitivity and whole-body insulin sensitivity as predictors of hyperglycaemia in non-diabetic subjects. Diabetologia 48, 2470–2476 (2005). https://doi.org/10.1007/s00125-005-0004-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-0004-7