Abstract
Aims/hypothesis
SHIP2 is a physiologically important negative regulator of insulin signalling hydrolysing the PI3-kinase product, PI(3,4,5)P3, which also has an impact on insulin resistance. In the present study, we examined the effect of inhibiting the endogenous SHIP2 function on the insulin resistance caused by chronic insulin treatment.
Methods
The endogenous function of SHIP2 was inhibited by expressing a catalytically inactive SHIP2 (ΔIP-SHIP), and compared with the effect of treatments designed to restore the levels of IRS-1 in insulin signalling systems of 3T3-L1 adipocytes.
Results
Chronic insulin treatment induced the large (86%) down-regulation of IRS-1 and the modest (36%) up-regulation of SHIP2. Subsequent stimulation by insulin of Akt phosphorylation, PKCλ activity, and 2-deoxyglucose (2-DOG) uptake was markedly decreased by the chronic insulin treatment. Coincubation with the mTOR inhibitor, rapamycin, effectively inhibited the proteosomal degradation of IRS-1 caused by the chronic insulin treatment. Although the coincubation with rapamycin and advanced overexpression of IRS-1 effectively ameliorated subsequent insulin-induced phosphorylation of Akt, insulin stimulation of PKCλ activity and 2-DOG uptake was partly restored by these treatments. Similarly, expression of ΔIP-SHIP2 effectively ameliorated the insulin-induced phosphorylation of Akt without affecting the amount of IRS-1. Furthermore, the decreased insulin-induced PKCλ activity and 2-DOG uptake following chronic insulin treatment were ameliorated by the expression of ΔIP-SHIP2 more effectively than by the treatment with rapamycin.
Conclusions/interpretation
Our results indicate that the inhibition of endogenous SHIP2 is effective in improving the state of insulin resistance caused by chronic insulin treatment.
Similar content being viewed by others
Introduction
The activation of phosphatidylinositol 3-kinase (PI3-kinase) is known to be important to the various metabolic actions of insulin [1–4]. PI(3,4,5)P3 produced by activated PI3-kinase is thought to function as a key lipid second messenger in insulin signalling to further downstream molecules [3–5]. We and others identified SH2-containing inositol 5′-phosphatase 2 (SHIP2) as a lipid phosphatase possessing 5′-phosphatase activity to hydrolyse PI(3,4,5)P3 to PI(3,4)P2 [6, 7]. Previous reports have indicated that overexpression of SHIP2 inhibits insulin-induced glucose uptake and glycogen synthesis via its 5′-phosphatase activity in 3T3-L1 adipocytes and L6 myocytes [8, 9]. Targeted disruption of the SHIP2 gene in mice increased sensitivity to insulin without affecting other biological systems [10]. These findings indicate that SHIP2 is a physiologically important negative regulator that is relatively specific to insulin signalling. In addition, expression of SHIP2 protein is enhanced in the skeletal muscle and fat tissue of diabetic db/db mice [11]. Treatment with the insulin-sensitizing thiazolidinedione, rosiglitazone, lowered the elevated levels of SHIP2 in the db/db mice [11]. Furthermore, a deletion in the 3′ untranslated region within the motifs implicated in the control of protein synthesis leading to the possible increase in expression of SHIP2 protein was identified in the UK and Belgian population of individuals with type 2 diabetes [12]. Therefore, SHIP2 is implicated in insulin resistance as a cause of type 2 diabetes in addition to the physiological importance in insulin signalling. Based on these findings, inhibition of endogenous SHIP2 function may be a target for ameliorating insulin signalling in the state of insulin resistance.
Hyperinsulinaemia is a hallmark of insulin resistance [13–15]. Chronic hyperinsulinaemia causes a desensitization to subsequent insulin responses, which appears to be part of the vicious cycle involved in the pathogenesis of type 2 diabetes [16–18]. In this regard, chronic treatment with insulin is known to facilitate the proteosomal degradation of IRS-1 leading to the down-regulation of insulin signalling at IRS-1 in 3T3-L1 adipocytes [17–19]. However, it is unknown whether SHIP2 is also involved in the resistance caused by chronic exposure to insulin. In the present study, the change in SHIP2 expression following chronic insulin treatment was investigated in 3T3-L1 adipocytes. In addition, the effect of inhibition of endogenous SHIP2 function using adenovirus-mediated gene transfer of a dominant-negative SHIP2 (ΔIP-SHIP2) on the possible amelioration of decreased insulin signalling caused by the chronic insulin treatment was investigated. The down-regulation of insulin signalling at the level of IRS-1 caused by the chronic insulin treatment can be ameliorated by pretreatment with rapamycin, which is an inhibitor of mTOR-dependent proteosomal degradation of IRS-1 [20, 21]. Alternatively, the decrease of IRS-1 can be prevented by overexpression of IRS-1 through adenovirus-mediated gene transfer [22]. Finally, the effects of the amelioration at the level of IRS-1 and SHIP2 on the chronic insulin treatment-induced down-regulation of insulin signalling were compared.
Materials and methods
Materials
Human crystal insulin was provided by Novo Nordisk Pharmaceutical (Copenhagen, Denmark). [γ-32P]ATP (111 TBq/mmol) and 2-[3H]deoxyglucose (DOG; 3,330 GBq/mmol) were purchased from NEN Life Science Products (Boston, MA, USA). The two polyclonal anti-SHIP2 antibodies were described previously [7]. A polyclonal anti-PKCλ antibody was kindly provided by Dr W. Ogawa (Kobe University, Japan) [22]. A monoclonal antiphosphotyrosine antibody (PY99) was from Transduction Laboratories (Lexington, KY, USA). A polyclonal anti-Thr308 phospho-specific Akt antibody, a polyclonal anti-Ser473 phospho-specific Akt antibody, and a monoclonal anti-PKCλ antibody were from Cell Signalling (Beverly, MA, USA). A polyclonal anti-Akt antibody and a polyclonal anti-Glut4 antibody were from Santa Cruz Biotechnology (Santa Cruz, CA, USA). A polyclonal IRS-1 antibody and a polyclonal anti-PDGF β receptor antibody were from Upstate Biotechnology (Lake Placid, NY, USA). Enhanced chemiluminescence reagents were from Amersham Pharmacia Biotech (Uppsala, Sweden). Dulbecco’s modified Eagle’s medium (DMEM), minimum essential medium (MEM) vitamin mixtures, and MEM amino acid solutions were from Gibco BRL Japan (Tokyo, Japan). All other reagents were of analytical grade and purchased from Sigma Chemical (St Louis, MO, USA) or Wako Pure Chemical Industries (Osaka, Japan).
Construction of adenoviral vectors
A cDNA encoding a phosphatidylinositol 5′-phosphatase-defective mutant of SHIP2 (ΔIP-SHIP2) containing Pro687 to Ala, Asp691 to Ala, and Arg692 to Gly changes was subcloned into the vector pAxCAwt, and transferred to recombinant adenovirus by homologous recombination utilizing an Adenovirus Expression Vector Kit (Takara Biomedicals, Tokyo, Japan) as described previously [8]. The adenoviral vector encoding IRS-1 was also described previously [23].
Cell culture and infections with adenovirus
3T3-L1 fibroblasts were grown and passaged in DMEM supplemented with 10% donor calf serum. Cells at 2–3 days postconfluence were used for differentiation. The differentiation medium contained 10% fetal bovine serum (FBS), 250 nmol/l dexamethasone, 0.5 mmol/l isobutyl methylxanthine, and 500 nmol/l insulin. After 3 days, the differentiation medium was replaced with postdifferentiation medium containing 10% FBS and 500 nmol/l insulin. After 3 more days, the postdifferentiation medium was replaced with DMEM supplemented with 10% FBS. ΔIP-SHIP2 and IRS-1 were transiently expressed in differentiated 3T3-L1 adipocytes by means of adenovirus-mediated gene transfer. A multiplicity of infection (m.o.i.) of 10–40 pfu/cell was used to infect 3T3-L1 adipocytes in DMEM containing 2% FBS, with the virus being left on the cells for 16 h prior to removal. Subsequent experiments were conducted 24–48 h after initial addition of the virus [8]. The efficiency of adenovirus-mediated gene transfer of ΔIP-SHIP2 and IRS-1 was approximately 95%.
Measurements of PI(3,4,5)P3 and PI(3,4)P2 levels in vivo
The same numbers of 3T3-L1 adipocytes transfected with LacZ or ΔIP-SHIP2 were starved of phosphate overnight in phosphate-free DMEM (Life Technology), then starved of serum for 3 h. [32P]Orthophosphate (3.7 MBq/ml) was added, and the cells were cultured for an additional 2 h. Following the labelling period, the cells were incubated with or without 1 μmol/l insulin for 15 min. The reaction was terminated by washing once with ice-cold PBS, followed by the addition of methanol and 1 N HCl (1:1). The labelling of the cells with [32P]orthophosphate was conducted at the same time in both sets of transfected cells. Phospholipids were then extracted with chloroform. The extracted lipid was deacylated and subjected to amino-exchange high-performance liquid chromatography (HPLC) using a Partisphere strong anion-exchange column (Whatman) as described previously [8]. The PI(3,4)P2 and PI(3,4,5)P3 levels in the same sample for each line were measured within a single HPLC run. The radioactivity was detected with an online radiochemical detector.
Chronic insulin treatment
3T3-L1 adipocytes grown in 6-well multiplates were incubated with DMEM containing 0.1% FBS with or without 100 nmol/l insulin at 37°C for various periods. For experiments with rapamycin treatment, 20 nmol/l rapamycin was added for 30 min before the addition of insulin. At the end of the chronic treatment with insulin, the cells were washed with PBS, incubated in serum-free DMEM for 30 min, and washed again with PBS. The cells were then treated with or without 17 nmol/l insulin for 5 min.
Plasma membrane fractionation
The cells were washed twice with PBS and once with HES buffer (255 mmol/l sucrose, 20 mmol/l HEPES, 1 mmol/l EDTA, 1 mmol/l phenylmethylsulphonyl fluoride [PMSF], 1 mmol/l Na3VO4, 2 μg/ml of aprotinin, and 50 ng/ml of okadaic acid, pH 7.4) and immediately homogenized by 20 strokes with a motor-driven homogenizer in HES buffer at 4°C. The homogenates (two 10-cm-diameter dishes per condition) were subjected to subcellular fractionation as described previously to isolate the plasma membrane (PM) [21]. In brief, the homogenates were centrifuged at 19,000 g for 20 min. The pellet obtained from the spin was resuspended in HES buffer, layered onto a 1.12 mol/l sucrose cushion, and centrifuged at 100,000 g in a swing rotor for 60 min. A white fluffy band at the interface was collected, resuspended in HES buffer, and centrifuged at 40,000 g for 20 min, yielding a pellet of PM. All fractions were adjusted to a final protein concentration of 1–3 mg/ml, which was measured by the Bradford method, and stored at −80°C until use.
Immunoprecipitation and western blotting
The cells or the plasma membrane preparation were lysed in a buffer containing 20 mmol/l Tris, 150 mmol/l NaCl, 1 mmol/l EDTA, 1 mmol/l EGTA, 2.5 mmol/l sodium deoxycholate, 1 mmol/l β-glycerophosphate, 1% Triton X-100, 1 mmol/l PMSF, 1 mmol/l Na3VO4, 50 mmol/l sodium fluoride, 10 μg/ml of aprotinin, and 10 μmol/l leupeptin, pH 7.4, for 30 min at 4°C. The lysates were centrifuged to remove insoluble materials. The supernatants (100 μg of protein) were immunoprecipitated with antibodies for 2 h at 4°C. The precipitates or the lysates were then separated by 7.5% SDS-PAGE and transferred onto polyvinylidene difluoride membranes (PVDM) using a Bio-Rad Transblot apparatus. The membranes were blocked in a buffer containing 50 mmol/l Tris, 150 mmol/l NaCl, 0.1% Tween 20, and 2.5% bovine serum albumin (BSA) or 5% non-fat milk, pH 7.5, for 2 h at 20°C. They were then probed with antibodies for 2 h at 20°C or for 16 h at 4°C. After the membranes were washed in a buffer containing 50 mmol/l Tris, 150 mmol/l NaCl, and 0.1% Tween 20, pH 7.5, blots were incubated with a horseradish peroxidase-linked secondary antibody and subjected to enhanced chemiluminescence detection using ECL reagent according to the manufacturer’s instructions (Amersham) [8]. In each experiment, the intensity of the band derived from control cells was assigned a value of 1 arbitrary unit, and the intensity of all treated groups was expressed as a fold value of control.
Measurement of PKCλ activity
The cells were washed with ice-cold PBS and lysed with PKCλ buffer containing 50 mmol/l MOPS–HCl, 0.5% Triton X-100, 10% glycerol, 5 mmol/l EDTA, 5 mmol/l EGTA, 20 mmol/l NaF, 50 mmol/l β-glycerophosphate, 2 mmol/l Na3VO4, 2 mmol/l DTT, 1 μg/ml of leupeptin, and 2 mmol/l PMSF, pH 7.5. The lysates were centrifuged at 15,000 g for 20 min. The protein concentration in the resulting supernatants was determined with the use of bicinchoninic acid protein assay reagent (Pierce), and equal amounts of protein were subjected to immunoprecipitation with anti-PKCλ antibody. The immunoprecipitates were washed twice with PKCλ buffer containing 0.1% BSA, once with PKCλ buffer containing 0.1% BSA and 1 mol/l NaCl, and once with a solution containing 20 mmol/l Tris–HCl, 10% glycerol, 0.5 mmol/l EDTA, 0.5 mmol/l EGTA, 20 mmol/l 2-mercaptoethanol, 10 μg/ml of leupeptin, and 2 mmol/l PMSF, pH 7.5. Then, the precipitates were incubated for 14 min at 30°C with 14.8 kBq of [γ-32ATP] in a reaction mixture (25 μl) containing 35 mmol/l Tris, pH 7.5, 10 mmol/l MgCl2, 0.5 mmol/l EGTA, 0.1 mmol/l CaCl2, 40 μmol/l unlabelled ATP, 100 μg/ml of phosphatidylserine, and 30 μmol/l myelin basic protein (MBP) as a substrate. Kinase reactions were terminated by the addition of SDS sample buffer, and the samples were then fractionated by SDS-PAGE [8, 22]. The radioactivity incorporated into substrates was determined with a Fuji BAS 2000 image analyser.
Measurement of 2-DOG uptake
3T3-L1 adipocytes grown in 6-well multiplates were serum-starved for 3 h. The cells were treated with or without rapamycin for 30 min and further incubated with 17 nmol/l insulin for 6 h. The cells were washed once with PBS, three times with Krebs–Ringer phosphate (KRP)–HEPES buffer, 10 nmol/l HEPES, 131.2 mmol/l NaCl, 4.7 mmol/l KCl, 1.2 mmol/l MgSO4, 2.5 mmol/l CaCl2, and 2.5 mmol/l NaH2PO4, pH 6.0, and once with KRP–HEPES buffer containing 1% BSA, pH 7.4. The cells were then incubated with the same KRP–HEPES buffer for 1 h at 37°C. The cells were subsequently stimulated with various concentrations of insulin. Following 15 min of insulin treatment, 3.7 kBq of 2-[3H]DOG was added for 4 min. The reaction was stopped by the addition of 10 μmol/l cytochalasin B. The cells were washed three times with PBS and solubilized with 0.2 mmol/l SDS–0.2 N NaOH [8]. The radioactivity incorporated into the cells was measured by liquid scintillation counting.
Statistical analysis
The data are represented as means ± SEM. p Values were determined using Student’s t test, and p<0.05 was considered statistically significant.
Results
Effect of chronic insulin treatment on IRS-1 and SHIP2
Chronic treatment with insulin facilitates the proteosomal degradation of IRS-1 [20, 21, 24, 25]. Treatment with insulin reduced the amount of IRS-1, but not Akt, in a time-dependent manner in 3T3-L1 adipocytes. After 12 h of treatment, the amount of IRS-1 was 13.6±2.6% of the control level (Fig. 1a). In accordance with the reduced amount of IRS-1, the subsequent insulin-stimulated tyrosine phosphorylation of IRS-1 following chronic insulin treatment was markedly decreased to 13.2±1.8% (Fig. 1b). Thus, chronic insulin treatment caused an impairment of insulin signalling, at least, at the step involving IRS-1. Since SHIP2 is an important negative regulator of insulin signalling, alteration of its expression may cause insulin resistance [8–12]. In this regard, the amount of SHIP2 protein was relatively high after chronic treatment with insulin. Following 6 h of insulin treatment, the amount of SHIP2, but not Akt, was increased by 36.4±7.4% (Fig. 1c). Membrane targeting of SHIP2 is known to be important to its function to hydrolyse PI(3,4,5)P3 in insulin signalling [26]. The extent of insulin-induced translocation of SHIP2 to the plasma membrane fraction was increased by 33.4±8.3% compared to that without chronic insulin treatment. To assure equal amounts of protein were loaded among the samples, the PM fraction was immunoblotted with anti-PDGF β receptor antibody (Fig. 1d). These results indicate that chronic insulin treatment elicits insulin resistance, at least in part, at the level of SHIP2 as well as IRS-1.
Effect of chronic insulin treatment on IRS-1 and SHIP2. 3T3-L1 adipocytes were treated with 17 nmol/l insulin for the periods indicated (chronic insulin treatment). a The cells were lysed, and the proteins were separated by SDS-PAGE and immunoblotted with anti-IRS-1 antibody or anti-Akt antibody. b After chronic insulin treatment, the cells were washed with PBS and incubated in insulin-free medium for 30 min, then stimulated with 17 nmol/l insulin for 5 min (acute insulin treatment). The cell lysates were immunoprecipitated with anti-IRS-1 antibody. The precipitates were subjected to SDS-PAGE, and immunoblotted with anti-phosphotyrosine antibody (PY99) or anti-IRS-1 antibody. c The cell lysates were separated by SDS-PAGE and immunoblotted with anti-SHIP2 antibody or anti-Akt antibody. *p<0.05 versus amounts of SHIP2 without chronic insulin treatment. d The cells were homogenized and subjected to subcellular fractionation to yield the plasma membrane (PM) fraction. Samples in the PM fraction were separated by SDS-PAGE and immunoblotted with anti-SHIP2 antibody or anti-PDGF β receptor antibody. *p<0.05 versus amounts of SHIP2 at PM following 5 min of insulin stimulation without chronic insulin treatment. Results are means ± SEM of three separate experiments.
Inhibition of endogenous SHIP2 function by expression of ΔIP-SHIP2
Because an elevated amount of SHIP2, especially at the plasma membrane, appears to be involved in the insulin resistance caused by the chronic insulin treatment, expression of ΔIP-SHIP2, which acts in a dominant-negative manner, may ameliorate the impaired insulin signalling. Adenovirus-mediated gene transfer produced an eightfold increase in ΔIP-SHIP2 expression compared to the endogenous level of SHIP2 (Fig. 3b). The expression of ΔIP-SHIP2 increased insulin-induced generation of PI(3,4,5)P3, whereas the amount of PI(3,4)P2 was decreased (Fig. 2a). Thus, the expression of ΔIP-SHIP2 in fact functions to inhibit the endogenous 5′-phosphatase activity of SHIP2 in 3T3-L1 adipocytes. In addition, insulin-induced increase in the levels of PI(3,4,5)P3 was decreased to 25% after chronic insulin exposure. ΔIP-SHIP2 expression ameliorated the reduced levels of PI(3,4,5)P3 to 61% of the control level (data not shown). Thus, expression of ΔIP-SHIP2 appears to effectively ameliorate the decreased PI(3,4,5)P3 levels caused by chronic insulin treatment.
Inhibition of endogenous SHIP2 function by expression of ΔIP-SHIP2. 3T3-L1 adipocytes were transfected with LacZ or ΔIP-SHIP2 at an m.o.i. of 40 pfu/cell. The cells were labelled with [32P]orthophosphate for 2 h and incubated with or without insulin, and lipids were extracted with chloroform. The extracted lipids were analysed by HPLC after being deacylated. The amounts of 32P-labelled PI(3,4,5)P3 (a) and PI(3,4)P2 (b) generated were determined with an online radiochemical detector. Results are means of two separate experiments.
Effect of ΔIP-SHIP2 and IRS-1 expression, and pretreatment with rapamycin on insulin-induced phosphorylation of Akt after chronic insulin treatment
Treatment with PI3-kinase inhibitor LY294002 effectively inhibited the chronic insulin treatment-induced degradation of IRS-1. Expression of ΔIP-SHIP2 partly abolished the inhibitory effect of LY294002 on the IRS-1 degradation, because SHIP2 is located downstream of PI3-kinase (data not shown). These results indicate that chronic insulin treatment induces the degradation of IRS-1 via PI3-kinase dependent mechanism. mTOR is a downstream molecule of PI3-kinase, and rapamycin is known to efficiently inhibit mTOR-dependent proteosomal degradation of IRS-1 in 3T3-L1 adipocytes [19–21]. Thus, the decrease in the amount of IRS-1 induced by degradation after chronic insulin treatment was effectively prevented by pretreatment with rapamycin. In contrast, expression of ΔIP-SHIP2 alone did not affect the loss of IRS-1 caused by the chronic insulin treatment. In addition, the preventive effect of rapamycin was not affected by the expression of ΔIP-SHIP2, because SHIP2 is located upstream of mTOR [8]. The decrease in IRS-1 caused by chronic insulin treatment can also be prevented by advanced overexpression of IRS-1. Thus, overexpression of IRS-1 in advance prevented the decrease in IRS-1 caused by chronic insulin treatment in an m.o.i.-dependent manner (data not shown). At an m.o.i. of 10 pfu/cell, the amount of IRS-1 after chronic insulin treatment was similar to that without chronic insulin treatment. The amount of protein loaded among the samples was confirmed to be identical by immunoblotting with anti-Akt antibody (Fig. 3b). As a result, rapamycin treatment and IRS-1 overexpression ameliorated the decreased levels of PI(3,4,5)P3 by chronic insulin treatment to 52% and 58%, respectively, of the control level (data not shown). Akt is an important mediator of the metabolic actions of insulin, and the activation of Akt is induced by the phosphorylation at Thr308 and Ser473 [8, 26–28]. Chronic insulin treatment decreased the subsequent insulin-stimulated phosphorylation of Akt at Thr308 and Ser473 to 23.8±2.0% and 28.5±2.1%, respectively. The reduction can be caused by the alteration of IRS-1 and/or SHIP2 following chronic insulin treatment. In this regard, pretreatment with rapamycin ameliorated the insulin-induced phosphorylation of Akt at Thr308 and Ser473. Similarly, overexpression of ΔIP-SHIP2 effectively ameliorated the phosphorylation of Akt at Thr308 and Ser473 in an m.o.i.-dependent manner (data not shown), and it was most effectively ameliorated at an m.o.i. of 40 pfu/cell. The amelioration was more apparent and almost fully restored to the control level by both pretreatment with rapamycin and expression of ΔIP-SHIP2. In addition, the effective restoration of insulin-stimulated phosphorylation of Akt following chronic insulin treatment was also seen after advanced overexpression of IRS-1 (Fig. 3a).
Effect of ΔIP-SHIP2 and IRS-1 expression, and pretreatment with rapamycin on insulin-induced phosphorylation of Akt after chronic insulin treatment. 3T3-L1 adipocytes were transfected with LacZ and ΔIP-SHIP2 at an m.o.i of 40 pfu/cell, or IRS-1 at an m.o.i. of 10 pfu/cell. Serum-starved transfected cells were incubated with vehicle or 20 nmol/l rapamycin for 30 min, and treated with 17 nmol/l insulin for 6 h. The cells were washed with PBS and incubated in insulin-free medium for 30 min, and the cells were stimulated with 17 nmol/l insulin for 5 min. a The cells were lysed and the lysates were separated by SDS-PAGE and immunoblotted with anti-Ser473-phospho-specific or anti-Thr308-phospho-specific Akt antibody. The amount of Akt phosphorylated at Ser473 and Thr308 was quantitated by densitometry. Results are means ± SEM of four separate experiments. *p<0.05 versus amounts of phosphorylated Akt in LacZ-transfected cells with chronic insulin treatment. b The cell lysates were separated by SDS-PAGE, and immunoblotted with anti-IRS-1 antibody, anti-SHIP2 antibody, or anti-Akt antibody.
Effect of ΔIP-SHIP2 and IRS-1 expression, and pretreatment with rapamycin, on insulin-induced activation of PKCλ after chronic insulin treatment
Another important molecule downstream of PI3-kinase for metabolic insulin signalling is atypical PKC in 3T3-L1 adipocytes [22, 29]. In accordance with the results of insulin-induced phosphorylation of Akt, insulin stimulation of PKCλ activity was decreased to 23.8±3.9% of the control level after chronic insulin treatment. Pretreatment with rapamycin only partly restored the decreased PKCλ activity to 49.8±3.8%. Although the effect was still partial, expression of ΔIP-SHIP2 relatively efficiently ameliorated the reduced PKCλ activity caused by the chronic insulin treatment to 65.0±7.5% of the control level. A combination of rapamycin treatment and expression of ΔIP-SHIP2 more effectively restored the insulin-induced activation of PKCλ. In contrast to the results for the phosphorylation of Akt, the restoration of PKCλ activity was still partial, and was 75.2±4.1% of the control level. The partial amelioration of insulin-stimulated PKCλ activity after chronic insulin treatment was also seen with advanced overexpression of IRS-1 (Fig. 4a). The amount of PKCλ protein was not altered either by chronic insulin treatment, treatment with rapamycin, or expression of ΔIP-SHIP2 and IRS-1 (Fig. 4b).
Effect of ΔIP-SHIP2 and IRS-1 expression, and pretreatment with rapamycin, on insulin-induced activation of PKCλ after chronic insulin treatment. 3T3-L1 adipocytes were transfected with LacZ and ΔIP-SHIP2 at an m.o.i. of 40 pfu/cell, or IRS-1 at an m.o.i. of 10 pfu/cell. Serum-starved transfected cells were incubated with vehicle or 20 nmol/l rapamycin for 30 min, and treated with 17 nmol/l insulin for 6 h. The cells were washed with PBS, incubated in insulin-free medium for 30 min, and stimulated with 100 nmol/l insulin for 5 min. They were then lysed and immunoprecipitated with anti PKCλ antibody. Kinase reactions were conducted, and samples were fractionated by SDS-PAGE. a The radioactivity incorporated into substrates was determined with a Fuji BAS 2000 image analyser. Results are means ± SEM of three separate experiments; *p<0.05 versus insulin-stimulated PKCλ activity in LacZ-transfected control cells with chronic insulin treatment. b The cell lysates were separated by SDS-PAGE, and immunoblotted with anti-PKCλ antibody.
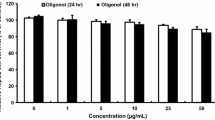
Effect of ΔIP-SHIP2 and IRS-1 expression, and pretreatment with rapamycin, on insulin-induced 2-DOG uptake after chronic insulin treatment
Since insulin-stimulated phosphorylation of Akt and PKCλ activity decreased by the chronic insulin treatment was ameliorated by rapamycin treatment and expression of ΔIP-SHIP2 and IRS-1, we next examined these effects on insulin stimulation of 2-DOG uptake (Fig. 5a). Again, insulin-induced 2-DOG uptake was markedly decreased to 25.6±5.2% after chronic insulin treatment. Pretreatment with rapamycin and expression of ΔIP-SHIP2 partially restored the decreased 2-DOG uptake to 47.5±3.7% and 54.4±4.1%, respectively, of the control level. Both rapamycin treatment and ΔIP-SHIP2 expression more efficiently ameliorated the reduced 2-DOG uptake to 69.2±4.4%. Advanced overexpression of IRS-1 also improved the reduced 2-DOG uptake to 69.7±2.5% of the control level. The amount of Glut4 protein was not altered either by chronic insulin treatment, treatment with rapamycin, or overexpression of ΔIP-SHIP2 and IRS-1 (Fig. 5b).
Effect of ΔIP-SHIP2 and IRS-1 expression, and pretreatment with rapamycin, on insulin-induced 2-DOG uptake after chronic insulin treatment. 3T3-L1 adipocytes were transfected with LacZ and ΔIP-SHIP2 at an m.o.i. of 40 pfu/cell, or IRS-1 at an m.o.i. of 10 pfu/cell. Serum-starved transfected cells were incubated with vehicle or 20 nmol/l rapamycin for 30 min, and treated with 100 nmol/l insulin for 6 h. The cells were washed with PBS, incubated in insulin-free medium for 3 h, and washed again with PBS and incubated in glucose-free medium for another 30 min. After the cells had been stimulated with 10 nmol/l insulin for 5 min, 3.7 kBq of 2-[3H]DOG was added for 3 min. The reaction was stopped by the addition of 10 μmol/l cytochalasin B. The cells were washed three times with PBS and solubilized with 0.2 mmol/l SDS–0.2 N NaOH. a The radioactivity incorporated into the cells was measured with a liquid scintillation counter. Results are means ± SEM of three separate experiments. *p<0.05 versus insulin-induced 2-DOG uptake in LacZ-transfected control cells with chronic insulin treatment. b The cell lysates were separated by SDS-PAGE and immunoblotted with anti-Glut4 antibody.
Discussion
Chronic insulin exposure is known to cause a subsequent insulin resistance, by reducing the level of IRS-1 via PI3-kinase and rapamycin-dependent pathways [17–21, 30, 31]. In fact, our results demonstrated that chronic insulin treatment induced a reduction in IRS-1 levels in a time-dependent manner. In addition to the impaired IRS-1–dependent signalling pathway, the present study showed increased amounts of SHIP2 following chronic insulin exposure. Since SHIP2 is the physiologically important negative regulator of insulin signalling with a fundamental impact on the state of insulin resistance [8–12], the increase in SHIP2 protein appears to be part of the novel molecular mechanism of insulin resistance caused by chronic insulin treatment. Because SHIP2 is translocated to the plasma membrane where it functions to hydrolyse PI(3,4,5)P3, the increase in the amount of SHIP2 protein in the plasma membrane preparation further supports the possible involvement of SHIP2 in insulin resistance in 3T3-L1 adipocytes [26].
We employed two approaches to ameliorate the decrease in IRS-1 levels caused by the chronic insulin treatment. As shown in Fig. 3, pretreatment with rapamycin prevented the mTOR-dependent proteosomal degradation of IRS-1 caused by the chronic insulin treatment. Overexpression of exogenous IRS-1 in advance normalized the decreased IRS-1 levels caused by the insulin treatment. On the other hand, endogenous SHIP2 function was efficiently inhibited by expression of the 5′-phosphatase defective dominant-negative SHIP2 (ΔIP-SHIP2) as shown in Fig. 2. These approaches would be useful for clarifying whether the rescue of insulin signalling at the level of IRS-1 and/or SHIP2 is effective in ameliorating insulin resistance caused by chronic insulin treatment. The decrease in the phosphorylation of Akt caused by the chronic insulin treatment was effectively ameliorated by either prevention of the decrease in IRS-1 by rapamycin treatment or advanced IRS-1 overexpression, or inhibition of endogenous SHIP2 function by expression of the dominant-negative SHIP2 (ΔIP-SHIP2). These results indicate that insulin-induced phosphorylation of Akt is closely associated with the IRS-1–mediated PI3-kinase pathway. In addition, the full input of insulin signal does not appear to be required for the sufficient phosphorylation of Akt, because amelioration of insulin signalling at the step involving IRS-1 or SHIP2 is sufficient for the efficient restoration of the phosphorylation of Akt.
Phosphorylation at both Thr308 and Ser473 is required for the full activation of Akt [8, 26–28]. In this context, our results showed that the rescue of IRS-1 levels by treatment with rapamycin and overexpression of IRS-1 in advance, and expression of the dominant-negative SHIP2 (ΔIP-SHIP2), efficiently ameliorated the decreased insulin-induced phosphorylation of Akt at both residues caused by the chronic insulin treatment. In contrast to the effective recovery of acute insulin stimulation of Akt phosphorylation, the recovery of acute insulin stimulation of PKCλ activation was only partial for both the restoration of IRS-1 levels and inhibition of SHIP2 function. Thus, pretreatment with rapamycin, advanced IRS-1 overexpression, and ΔIP-SHIP2 expression only partially ameliorated the insulin-induced activation of PKCλ to 49.8±3.8%, 67.2±8.5%, and 65.0±7.5%, respectively, of the control value. The rescue of the PKCλ activity was still partial with a combination of ΔIP-SHIP2 expression and rapamycin pretreatment (or IRS-1 expression—data not shown). Therefore, the insulin resistance caused by chronic treatment may also impair insulin signalling at the step important for PKCλ activation more directly in addition to the IRS-1–PI3-kinase pathway. It is possible that another insulin signalling system important for glucose uptake including the CAP–Cbl–TC10 pathway may be a candidate implicated in the signalling step, although further investigation is needed to clarify the issue [32, 33]. We can not rule out the possibility that full activation of the IRS-1–PI3-kinase pathway is required for the efficient activation of PKCλ, although resistance at the levels of IRS-1 and SHIP2 appears to be efficiently rescued by pretreatment with rapamycin and expression of ΔIP-SHIP2.
Interestingly, the decreased stimulation of 2-DOG uptake caused by chronic insulin treatment was only partly restored by the maintenance of IRS-1 levels by pretreatment with rapamycin or advanced overexpression of IRS-1, or expression of ΔIP-SHIP2 as shown in Fig. 5. These findings are consistent with the results of PKCλ activation, and not Akt activation. Although Akt and atypical PKC are downstream effectors of PI3-kinase strongly implicated in the metabolic actions of insulin, the relative importance of Akt versus atypical PKC in insulin-induced 2-DOG uptake is controversial [8, 22, 27–29, 34]. Our results indicate that PKCλ/ζ rather than Akt may be more closely linked to the insulin-stimulated glucose uptake and associated with the state of insulin resistance. It is unclear whether this difference between Akt and PKCλ activation in chronic insulin treatment reflects a small input of IRS-1–dependent insulin signalling sufficient for Akt activation, or whether factors other than IRS-1–dependent insulin signalling are involved in the impairment of PKCλ activation. In any event, our results indicate that PKCλ activity rather than Akt activity appears to be associated with the decreased glucose uptake caused by chronic insulin treatment. Regardless of the importance of PKCλ to the state of insulin resistance, overexpression of the constitutively active form of PKCλ did not completely rescue the decreased insulin-stimulated glucose uptake caused by the chronic insulin treatment (data not shown). Based on this observation, chronic insulin treatment appears to cause insulin resistance at multiple signalling steps including a step distal to the PKCλ activation leading to the glucose uptake. It is also possible that chronic insulin treatment impairs the glucose uptake involved in the Glut4 translocation system independent of insulin signalling as previously reported for the insulin resistance caused by dexamethasone treatment in 3T3-L1 adipocytes [23].
In summary, SHIP2 appears to participate in insulin resistance, at least in part, caused by chronic insulin treatment in 3T3-L1 adipocytes. In addition, (1) impaired early insulin signalling occurring mainly at IRS-1 for the PI3-kinase activation, (2) impaired insulin signalling for PKCλ activation, and (3) impaired glucose transport system may also be involved in the insulin resistance caused by chronic insulin treatment. Furthermore, the present study indicates that the inhibition of endogenous SHIP2 appears to be effective at ameliorating the insulin signal in a state of insulin resistance, and that the activity of PKCλ rather than Akt may be more closely associated with the decreased 2-DOG uptake caused by the chronic insulin treatment in 3T3-L1 adipocytes. Taken together, inhibition of the endogenous level and/or function of SHIP2 would be an important therapeutic target of insulin resistance in type 2 diabetes.
Abbreviations
- 2-DOG:
-
2-deoxyglucose
- Glut4:
-
glucose transporter 4
- IRS-1:
-
insulin receptor substrate-1
- mTOR:
-
mammalian target of rapamycin
- PDGF:
-
platelet-derived growth factor
- PI3-kinase:
-
phosphatidylinositol 3-kinase
- PI(3,4)P2:
-
phosphatidylinositol 3,4-bisphosphate
- PI(3,4,5)P3:
-
phosphatidylinositol 3,4,5-triphosphate
- PKC:
-
protein kinase C
- SHIP2:
-
SH2-containing inositol 5′-phosphatase 2
References
Rameh LE, Cantley LC (1999) The role of phosphoinositide 3-kinase lipid products in cell function. J Biol Chem 274:8347–8350
Cantley LC (2002) The phosphoinositide 3-kinase pathway. Science 296:1655–1657
Virkamäki A, Ueki K, Kahn CR (1999) Protein–protein interaction in insulin signaling and the molecular mechanisms of insulin resistance. J Clin Invest 103:931–943
Czech MP, Corvera S (1999) Signaling mechanisms that regulate glucose transport. J Biol Chem 274:1865–1868
Saltiel AR, Pessin JE (2002) Insulin signaling pathways in time and space. Trends Cell Biol 12:65–71
Pesesse X, Deleu S, De Smedt F, Drayer L, Erneux C (1997) Identification of a second SH2-domain-containing protein closely related to the phosphatidylinositol polyphosphate 5-phosphatase SHIP. Biochem Biophys Res Commun 239:697–700
Ishihara H, Sasaoka T, Hori H et al (1999) Molecular cloning of rat SH2-containing inositol phosphatase 2 (SHIP2) and its role in the regulation of insulin signaling. Biochem Biophys Res Commun 260:265–272
Wada T, Sasaoka T, Funaki M et al (2001) Overexpression of SH2-containing inositol phosphatase 2 results in negative regulation of insulin-induced metabolic actions in 3T3-L1 adipocytes via its 5′-phosphatase catalytic activity. Mol Cell Biol 21:1633–1646
Sasaoka T, Hori H, Wada T et al (2001) SH2-containing inositol phosphatase 2 negatively regulates insulin-induced glycogen synthesis in L6 myotubes. Diabetologia 44:1258–1267
Clement S, Krause U, Desmedt F et al (2001) The lipid phosphatase SHIP2 controls insulin sensitivity. Nature 409:92–97
Hori H, Sasaoka T, Ishihara H et al (2002) Association of SH2-containing inositol phosphatase 2 with the insulin resistance of diabetic db/db mice. Diabetes 51:2387–2394
Marion E, Kaisaki PJ, Pouillon V et al (2002) The gene INPPL1, encoding the lipid phosphatase SHIP2, is a candidate for type 2 diabetes in rat and man. Diabetes 51:2012–2017
Reaven GM (1988) Role of insulin resistance in human disease. Diabetes 37:1595–1607
DeFronzo RA, Ferrannini E (1991) Insulin resistance: a multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care 14:173–194
Goalstone ML, Natarajan R, Standley PR et al (1998) Insulin potentiates platelet-derived growth factor action in vascular smooth muscle cells. Endocrinology 139:4067–4072
Rondinone CM, Wang L-M, Lonnroth P, Wesslau C, Pierce JH, Smith U (1997) Insulin receptor substrate (IRS) 1 is reduced and IRS-2 is the main docking protein for phosphatidylinositol 3-kinase in adipocytes from subjects with non-insulin-dependent diabetes mellitus. Proc Natl Acad Sci U S A 94:4171–4175
Ricort J-M, Tanti J-F, Van Obberghen E, Le Marchand-Brustel Y (1995) Alterations in insulin signalling pathway induced by prolonged insulin treatment of 3T3-L1 adipocytes. Diabetologia 38:1148–1156
Thomson MJ, Williams MG, Frost SC (1997) Development of insulin resistance in 3T3-L1 adipocytes. J Biol Chem 272:7759–7764
Berg CE, Lavan BE, Rondinone CM (2002) Rapamycin partially prevents insulin resistance induced by chronic insulin treatment. Biochem Biophys Res Commun 293:1021–1027
Haruta T, Uno T, Kawahara J et al (2000) A rapamycin-sensitive pathway down-regulates insulin signaling via phosphorylation and proteasomal degradation of insulin receptor substrate-1. Mol Endocrinol 14:783–794
Takano A, Usui I, Haruta T et al (2001) Mammalian target of rapamycin pathway regulates insulin signaling via subcellular redistribution of insulin receptor substrate 1 and integrates nutritional signals and metabolic signals of insulin. Mol Cell Biol 21:5050–5062
Kotani K, Ogawa W, Matsumoto M et al (1998) Requirement of atypical protein kinase Cλ for insulin stimulation of glucose uptake but not for Akt activation in 3T3-L1 adipocytes. Mol Cell Biol 18:6971–6982
Sakoda H, Ogihara T, Anai M et al (2000) Dexamethazone-induced insulin resistance in 3T3-L1 adipocytes is due to inhibition of glucose transport rather than insulin signal transduction. Diabetes 49:1700–1708
Sun XJ, Goldberg JL, Qiao L, Mitchell JJ (2002) Insulin-induced insulin receptor substrate-1 degradation is mediated by the proteasome degradation pathway. Diabetes 48:1359–1364
Zhande R, Mitchell JJ, Wu J, Sun XJ (2002) Molecular mechanism of insulin-induced degradation of insulin receptor substrate 1. Mol Cell Biol 22:1016–1026
Ishihara H, Sasaoka T, Ishiki M et al (2002) Membrane localization of src homology 2-containing inositol 5′-phosphatase 2 via Shc association is required for the negative regulation of insulin signaling in rat1 fibroblasts overexpressing insulin receptors. Mol Endocrinol 16:2371–2381
Kitamura T, Ogawa W, Sakaue H et al (1998) Requirement for activation of the serine-threonine kinase Akt (protein kinase B) in insulin stimulation of protein synthesis but not of glucose transport. Mol Cell Biol 18:3708–3717
Wang Q, Somwar R, Bilan PJ et al (1999) Protein kinase B/Akt participates in Glut4 translocation by insulin in L6 myoblasts. Mol Cell Biol 19:4008–4018
Bandyopadhyay G, Standaert ML, Zhao L et al (1997) Activation of protein kinase C (α, β, and ζ) by insulin in 3T3/L1 cells: transfection studies suggest a role for PKC-ζ in glucose transport. J Biol Chem 272:2551–2558
Pessin JE, Saltiel AR (2000) Signaling pathways in insulin action: molecular targets of insulin resistance. J Clin Invest 106:165–169
Sykiotis GP, Papavassiliou AG (2001) Serine phosphorylation of insulin receptor substrate-1: a novel target for the reversal of insulin resistance. Mol Endocrinol 15:1864–1869
Baumann CA, Ribon V, Kanzaki M et al (2000) CAP defines a second signalling pathway required for insulin-stimulated glucose transport. Nature 407:202–207
Chiang S-H, Baumann CA, Kanzaki M et al (2001) Insulin-stimulated Glut4 translocation requires the CAP-dependent activation of TC10. Nature 410:944–948
Bandyopadhyay G, Kanoh Y, Sajan MP, Standaert ML, Farese RV (2000) Effects of adenoviral gene transfer of wild-type, constitutively active, and kinase-defective protein kinase C-λ on insulin-stimulated glucose transport in L6 myotubes. Endocrinology 141:4120–4127
Acknowledgements
This work was supported in part by a grant-in-aid for scientific research from the Japan Society for the Promotion of Science. We thank Dr Wataru Ogawa (Kobe University, Japan) for kindly providing the anti-PKCλ antibody and Dr Kazuyuki Hiratani (Toyama Medical and Pharmaceutical University, Japan) for technical assistance. T. Sasaoka and K. Fukui contributed equally to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sasaoka, T., Fukui, K., Wada, T. et al. Inhibition of endogenous SHIP2 ameliorates insulin resistance caused by chronic insulin treatment in 3T3-L1 adipocytes. Diabetologia 48, 336–344 (2005). https://doi.org/10.1007/s00125-004-1636-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1636-8