Abstract
Aims/hypothesis
The molecular mechanisms of obesity-related insulin resistance are incompletely understood. Macrophages accumulate in adipose tissue of obese individuals. In obesity, monocyte chemoattractant protein-1 (MCP-1), a key chemokine in the process of macrophage accumulation, is overexpressed in adipose tissue. MCP-1 is an insulin-responsive gene that continues to respond to exogenous insulin in insulin-resistant adipocytes and mice. MCP-1 decreases insulin-stimulated glucose uptake into adipocytes. The A–2518G polymorphism in the distal regulatory region of MCP-1 may regulate gene expression. The aim of this study was to investigate the impact of this gene polymorphism on insulin resistance.
Methods
We genotyped the Ludwigshafen Risk and Cardiovascular Health (LURIC) cohort (n=3307). Insulin resistance, estimated by homeostasis model assessment, and Type 2 diabetes were diagnosed in 803 and 635 patients respectively.
Results
Univariate analysis revealed that plasma MCP-1 levels were significantly and positively correlated with WHR (p=0.011), insulin resistance (p=0.0097) and diabetes (p<0.0001). Presence of the MCP-1 G–2518 allele was associated with decreased plasma MCP-1 (p=0.017), a decreased prevalence of insulin resistance (odds ratio [OR]=0.82, 95% CI: 0.70–0.97, p=0.021) and a decreased prevalence of diabetes (OR=0.80, 95% CI: 0.67–0.96, p=0.014). In multivariate analysis, the G allele retained statistical significance as a negative predictor of insulin resistance (OR=0.78, 95% CI: 0.65–0.93, p=0.0060) and diabetes (OR=0.80, 95% CI: 0.66–0.96, p=0.018).
Conclusions/interpretation
In a large cohort of Caucasians, the MCP-1 G–2518 gene variant was significantly and negatively correlated with plasma MCP-1 levels and the prevalence of insulin resistance and Type 2 diabetes. These results add to recent evidence supporting a role for MCP-1 in pathologies associated with hyperinsulinaemia.
Similar content being viewed by others
Introduction
The molecular mechanisms that link obesity and insulin resistance are incompletely understood [1, 2, 3]. Obesity, insulin resistance and diabetes mellitus share a chronic, low-grade inflammatory component [4, 5, 6, 7], as reflected by increased expression of proinflammatory cytokines such as TNF-α [8], IL-6 [9], and monocyte chemoattractant protein-1 (MCP-1) [6, 7, 10, 11]. Adipose tissue functions as an endocrine organ that secretes a number of biologically active proteins, including TNF-α [8], IL-6 [6, 12], IL-8 [13], C-reactive protein, inducible nitric oxide synthase [6], TGF-β1, plasminogen-activator inhibitor-1 (PAI-1) [14], adiponectin [15], resistin [16], leptin [13, 17], macrophage inflammatory protein-1α (MIP-1α) [7, 13] and MCP-1 [6, 7, 10, 11, 17]. Obesity alters adipose tissue endocrine function and leads to the increased secretion of proinflammatory cytokines (so-called “adipokines”), hormones and fatty acids [6, 7, 10]. In turn, TNF-α, IL-1β, and other adipokines stimulate MCP-1 production and release by human differentiated adipocytes [13].
MCP-1, which is a member of the chemokine family, plays a key role in the recruitment of monocytes/macrophages to inflammatory foci [18]. High glucose directly up-regulates MCP-1 expression in vascular endothelial cells and monocytes [19, 20]. MCP-1 mRNA is dramatically overexpressed (increased by a factor of seven) in white adipose tissue of genetically obese (ob/ob) mice compared with lean control mice [10]. In these mice, the highest level of MCP-1 expression is in subcutaneous adipose tissue, with the liver showing <10% and the kidney and lung showing 1–2% of the level of MCP-1 expression in adipose tissue [10]. Insulin induces the production and secretion of substantial amounts of MCP-1 in insulin-resistant adipocytes and insulin-resistant obese mice [10]. MCP-1 is similar to other genes such as PAI-1 and SREBP-1c in that it continues to respond to exogenous insulin in insulin-resistant states [10, 21]. Moreover, MCP-1 inhibits (by approximately 30%) insulin-stimulated glucose uptake into mouse adipocytes [10]. Transcriptional profiling experiments have shown that a number of inflammation and macrophage-enriched or specific genes, such as MCP-1, MIP-1α, ADAM8, MAC-1, F4/80 and CD68, are up-regulated in white adipose tissue of mice with genetic or diet-induced obesity [6, 7]. Of the 100 genes whose expression was most significantly correlated with body mass, 30% encoded proteins that are characteristic of macrophages. In human subcutaneous adipose tissue, both BMI and average adipocyte size were significant predictors of macrophage accumulation [6]. In bone marrow transplant experiments in irradiated mice, 85% of the macrophages that accumulated in adipose tissue after placing the mice on a high-fat diet were of bone marrow origin [6]. In addition, in Csf1 op/op mice lacking macrophages, the presence of cells expressing the macrophage marker F4/80 in adipose tissue was greatly reduced compared with that in wild-type mice [6]. These findings suggest new models involving macrophage infiltration into adipose tissue in obesity-related insulin resistance.
Genetic differences in chemokine expression may contribute to differences in the severity of inflammatory processes between individuals. Substantial inter-individual variability in MCP-1 production in response to proinflammatory cytokines has previously been described [22, 23]. Human MCP-1 transcription is under the control of two distinct regions within the 5’-flanking sequence of the gene. The distal region contains two NF-κB binding sites and is essential for cytokine-dependent regulation, while the proximal region contains a GC box that may regulate tissue-specific expression [24]. A common A→G polymorphism located at position −2518 in the distal regulatory region regulates MCP-1 expression. This was demonstrated by transfection experiments in A172 and 293T cells using reporter gene constructs containing the distal regulatory region of the MCP-1 gene with either variant at position −2518 [22, 25]. Moreover, MCP-1 expression in isolated, cytokine-stimulated human peripheral blood mononuclear cells [22, 25] and hepatic cells [26], and plasma MCP-1 levels in patients with lupus nephritis support the assumption that the gene polymorphism regulates MCP-1 expression at the transcriptional level [25]. Case-control gene association studies have reported statistical associations between the polymorphism and lupus nephritis [25], coronary artery disease (CAD) [27] and asthma [28]. The aim of the present study was to test the hypothesis that the MCP-1 A–2518G polymorphism influences plasma MCP-1 levels and the risk of developing insulin resistance and Type 2 diabetes.
Subjects and methods
Study population and clinical definitions
We genotyped the Ludwigshafen Risk and Cardiovascular Health (LURIC) cohort of 3316 individuals who underwent coronary angiography because of chest pain or non-invasive tests consistent with myocardial ischaemia [29]. All individuals were Caucasians born in Germany to parents of German ancestry. Coronary artery disease was defined angiographically by a ≥20% reduction in lumenal diameter in one or more major epicardial coronary arteries or a 10% to 19% reduction in three or more (out of 15) coronary artery segments. Genetic testing of this cohort was approved by the appropriate institutional ethics committee and informed consent was obtained from the patients. After excluding nine individuals with Type 1 diabetes, the study population included 3307 individuals. Insulin resistance was estimated by homeostasis model assessment (HOMAIR) [30] in the 2798 individuals who were not receiving oral hypoglycaemic drugs or insulin treatment. The threshold for insulin resistance was defined as the 90th percentile of HOMAIR distribution in individuals (n=350) with no markers of the metabolic syndrome [30]. Type 2 diabetes was defined according to the new criteria of the American Diabetes Association (ADA) and the provisional criteria of the World Health Organization (WHO) [31, 32, 33]. Unlike in a previous study of the same cohort [34], subjects with a single test showing a high blood glucose level, in the absence of a confirmatory test, were not assigned an unequivocal diabetes status. Older age was defined by the 50th percentile of the study population.
Assessment of plasma MCP-1 levels
Plasma MCP-1 was measured in a subgroup of 940 consecutive patients (starting from recruitment number 1001) using the Quantikine Human MCP-1 Immunoassay (R&D Systems, Abingdon, UK). There were no significant differences (p>0.1) between this subgroup and the study population as a whole with respect to insulin resistance or diabetes distribution. Blood samples were collected, processed and stored according to the manufacturer’s instructions. The sensitivity of the kit is approximately 0.6 pmol/l, which is well below the lowest concentration measured in the present study (2.9 pmol/l).
Genotyping
Genotyping of the MCP-1 A–2518G polymorphism was carried out by RFLP-PCR as described previously [22]. Data are incomplete due to missing or equivocal results in five subjects.
Statistical analysis
Data are shown as frequencies in percent (numbers of subjects) or median values (25–75 percentiles). The JMP program (Version 5; SAS Institute, Cary, N.C., USA) was used for statistical analysis. Frequencies were compared by the Cochrane–Armitage trend test. Due to skewed distribution, plasma MCP-1 data were analysed by non-parametric tests (Wilcoxon and Kruskal–Wallis rank-sum tests). The gene counting method estimated allele frequencies, and the chi square test was used to test for deviations of genotype frequencies from Hardy–Weinberg equilibrium. The independent contributions of clinical and genetic characteristics (age, insulin resistance, diabetes, obesity, WHR, HDL cholesterol, triglycerides, hypertension, CAD and MCP-1 polymorphism) to MCP-1 plasma levels (entered as the dependent variable) were assessed by multivariate analysis (standard least square). The independent contributions of the MCP-1 polymorphism to insulin resistance and diabetes were determined by nominal logistic analysis, with insulin resistance or diabetes entered as the dependent variable, and age, sex, obesity, hypertension, HDL cholesterol, triglycerides and WHR entered as independent variables. In a subanalysis, diabetes was entered as a three-class-dependent variable (encoded as no diabetes = 0, non-insulin-treated diabetes = 1, insulin-treated diabetes = 2). A p value (two-tailed) of less than 0.05 was considered to be statistically significant.
Results
Clinical characteristics, insulin resistance and diabetes
In total, 29% (803 of 2798) of individuals who were not on pharmacological oral hypoglycaemic treatment had HOMAIR index values higher than or equal to 2.96, indicating insulin resistance. Type 2 diabetes was diagnosed in 20% (635 of 3205) of subjects. Among the diabetic patients, 25% (n=161) were on no oral hypoglycaemic drugs, 44% (n=278) were on oral hypoglycaemic drugs and 31% (n=196) were on insulin. Coronary angiography showed coronary artery stenoses (lumen reduction ≥50%) in 69% of patients, minor lesions (lumen reduction <50%) in 14% and smooth arteries in 17%. Table 1 shows the clinical characteristics of the study population subdivided according to insulin sensitivity or diabetes status, and the results of univariate analysis of the clinical characteristics in these subsets.
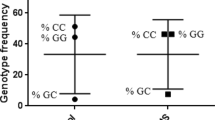
Genotype frequencies
In the population as a whole, the frequencies of the genotypes of the A–2518G polymorphism were: 1757 (53%) AA homozygous, 1303 (39%) GA heterozygous and 242 (7%) GG homozygous. The genotype frequencies were in Hardy–Weinberg equilibrium in the population as a whole and in cases and controls defined by insulin sensitivity or diabetes status. No differences were found between G allele carriers (GA or GG genotype) and non-carriers (AA genotype) with respect to age, sex, obesity, WHR, hypertension, triglycerides or HDL cholesterol between subsets (data not shown).
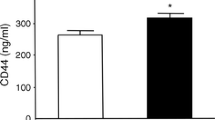
Associations between plasma MCP-1 levels and clinical and genetic data
In univariate analysis, plasma MCP-1 levels were significantly and positively correlated with age, CAD and markers of the metabolic syndrome (insulin resistance, Type 2 diabetes, hypertension, obesity, WHR, high triglycerides and low HDL cholesterol; Table 2). In addition, plasma MCP-1 levels were negatively correlated with the presence of the G allele at position −2518 of MCP-1 (p=0.043 and p=0.017 for genotype and G allele carrier frequencies respectively; Table 3). In multivariate analysis, age and HDL cholesterol remained associated with plasma MCP-1 (p<0.0001 and p=0.002 respectively), with a trend towards statistical significance for the MCP-1 polymorphism (p=0.06), whereas all other associations lost statistical significance (p>0.1).
Association between the MCP-1 A–2518G polymorphism and insulin resistance
The frequencies of the MCP-1 genotypes were significantly different between insulin-sensitive and insulin-resistant subjects (p=0.020), as were the frequencies of G allele carriers (p=0.021; Table 3). In multivariate analysis (Table 4), both genotype and G allele carrier frequencies retained significant associations with insulin resistance (χ2=7.56, p=0.023 and χ2=7.55, p=0.006 respectively).
Association between the MCP-1 A–2518G polymorphism and Type 2 diabetes
Presence of the G allele was associated with a decreased prevalence of Type 2 diabetes (p=0.014; Table 3). In multivariate analysis, genotype and G allele carrier frequencies were significantly associated with a decreased prevalence of diabetes (χ2=7.03, p=0.030 and χ2=5.62, p=0.018, respectively; Table 5). The decrease in the frequency of G allele carriers was more marked in the subgroup of insulin-treated patients than in the subgroup of non-insulin-treated diabetic patients (39% and 44% respectively, vs 48% in non-diabetic individuals; χ2=7.76, p=0.021 by three-class analysis).
Association between the MCP-1 A–2518G polymorphism and obesity-related insulin resistance
A subgroup analysis revealed that, among obese patients, the insulin-sensitive subgroup contained a higher proportion of MCP-1 G–2518 carriers than the insulin-resistant subgroup (52.5% vs 43.9%; p=0.04). Similarly, obese individuals who did not develop Type 2 diabetes were more likely to be G allele carriers than those who became diabetic (48.5% vs 40.5%; p=0.06). Plasma MCP-1 levels were significantly increased in obese diabetic patients compared with those in obese non-diabetic patients (21.4 vs 17.6 pmol/l; p<0.05).
Discussion
There is increasing evidence that MCP-1, a potent chemoattractant of monocytes/macrophages, participates in metabolic activities that involve regulation of adipose tissue functions, inhibition of insulin-stimulated glucose uptake into adipocytes [10] and accumulation of macrophages in adipose tissue in obese humans [6]. In search of genetic factors that affect insulin resistance, we investigated the role of the common MCP-1 A–2518G polymorphism, which may regulate MCP-1 expression at the transcriptional level [22, 25, 26]. In a large cohort of Caucasians with a high prevalence of cardiovascular risk factors, we found decreased plasma MCP-1 levels and a decreased prevalence of insulin resistance and Type 2 diabetes in carriers of the G allele compared with subjects homozygous for the frequent A allele. A protective role for this genetic variant is supported by the finding that, among obese patients, the frequency of G allele carriers was increased in those with preserved insulin sensitivity. In multivariate analysis, the G allele remained significantly and negatively correlated with insulin resistance and diabetes after correction for risk factors identified by univariate analysis (including CAD). The decrease in G allele frequency was more pronounced among insulin-treated patients than among non-insulin-treated diabetic patients, suggesting that the role of the gene polymorphism may become more manifest at later stages of the disease.
Our findings of decreased plasma MCP-1 levels in carriers of the G allele are in agreement with data in patients with lupus nephritis [25]. In the present study, plasma MCP-1 levels were significantly and positively correlated with markers of the metabolic syndrome, such as insulin resistance, Type 2 diabetes, hypertension, obesity, WHR, high triglycerides and low HDL cholesterol, according to univariate analysis. These results are consistent with previous data in patients with Type IIa and IIb hyperlipoproteinaemia [35]. Moreover, we observed increased plasma MCP-1 levels in patients with Type 2 diabetes, corroborating previous data from the Orbofiban in Patients With Unstable Coronary Syndromes—Thrombolysis In Myocardial Infarction (OPUS-TIMI) 16 trial and from a cohort of women with glucose intolerance [36, 37]. Conversely, another study showed that insulin infusion results in decreased plasma MCP-1 levels in obese subjects [38].
Macrophage accumulation in human subcutaneous adipose tissue increases with increasing obesity and adipocyte size [6]. In obesity, infiltrating macrophages account for almost all TNF-α expression and a significant proportion of the expression of other inflammatory mediators in adipose tissue [6]. Interestingly, the epicardial adipose tissue of patients with CAD produces increased amounts of MCP-1, TNF-α, IL-1β, and IL-6 compared with epicardial adipose tissue of subjects without CAD, suggesting that regional adipose tissue may be a source of atherogenic proinflammatory molecules [39].
The molecular mechanism by which the polymorphism regulates MCP-1 gene transcription is unclear. Although it is located in the distal regulatory region of the gene that contains two NF-κB binding sites essential for cytokine-stimulated gene transcription [24], the polymorphism does not alter the sequence of the NF-κB sites. Electrophoretic mobility shift assays have suggested that the binding site for an as yet unidentified transcription factor might be altered [22]. We propose that decreased MCP-1 expression in carriers of the G allele may prevent the pathogenic vicious circle by which MCP-1 expression promotes macrophage accumulation in adipose tissue, TNF-α release by macrophages, TNF-α-stimulated MCP-1 expression and MCP-1-mediated antagonism of insulin activities in this tissue. Similarly, a single-nucleotide polymorphism in the promoter of the gene encoding resistin, an adipocyte-secreted hormone, has been linked to insulin resistance in humans [40].
In conclusion, we have reported, for the first time, that the MCP-1 G–2518 allele is significantly and negatively correlated with circulating MCP-1 levels, insulin resistance and Type 2 diabetes. Replication of the reported genetic associations in independent cohorts are needed to validate the role of the polymorphism in the development of insulin resistance.
Abbreviations
- CAD:
-
coronary artery disease
- HOMAIR :
-
homeostasis model assessment of insulin resistance
- MCP-1:
-
monocyte chemoattractant protein-1
- MIP-1α:
-
macrophage inflammatory protein-1α
- NF-κB:
-
nuclear factor-κB
- PAI-1:
-
plasminogen-activator inhibitor-1
References
Zimmet P, Alberti KG, Shaw J (2001) Global and societal implications of the diabetes epidemic. Nature 414:782–787
Grundy SM, Brewer HB, Cleeman JI, Smith SC, Lefant C (2004) Definition of metabolic syndrome. Circulation 109:433–438
Alexander CM, Landsman PB, Teutsch SM, Haffner SM (2003) NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes 52:1210–1214
Dandona P, Aljada A, Bandyopadhyay A (2004) Inflammation: the link between insulin resistance, obesity and diabetes. Trends Immunol 25:4–7
Wellen KE, Hotamisligil GS (2003) Obesity-induced inflammatory changes in adipose tissue. J Clin Invest 112:1785–1788
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr (2003) Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 112:1796–1808
Xu H, Barnes GT, Yang Q et al. (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112:1821–1830
Uysal KT, Wiesbrock SM, Marino MW, Hotamisligil GS (1997) Protection from obesity-induced insulin resistance in mice lacking TNF-α function. Nature 389:610–614
Mohamed-Ali V, Goodrick S, Rawesh A et al. (1997) Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab 82:4196–4200
Sartipy P, Loskutoff DJ (2003) Monocyte chemoattractant protein 1 in obesity and insulin resistance. Proc Natl Acad Sci USA 100:7265–7270
Takahashi K, Mizuarai S, Araki H et al. (2003) Adiposity elevates plasma MCP-1 levels leading to increased CD11b-positive monocytes in mice. J Biol Chem 278:46654–46660
Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V (2000) Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis 148:209–214
Gerhardt CC, Romero IA, Cancello R, Camoin L, Strosberg AD (2001) Chemokines control fat accumulation and leptin secretion by cultured human adipocytes. Mol Cell Endocrinol 175:81–92
Juhan-Vague I, Alessi MC, Mavri A, Morange PE (2003) Plasminogen activator inhibitor-1, inflammation, obesity, insulin resistance and vascular risk. J Thromb Haemost 1:1575–1579
Yamauchi T, Kamon J, Waki H et al. (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 7:941–946
Steppan CM, Bailey ST, Bhat S et al. (2001) The hormone resistin links obesity to diabetes. Nature 409:307–312
Bruun JM, Pedersen SB, Kristensen K, Richelsen B (2002) Effects of pro-inflammatory cytokines and chemokines on leptin production in human adipose tissue in vitro. Mol Cell Endocrinol 190:91–99
Rollins BJ (1996) Monocyte chemoattractant protein 1: a potential regulator of monocyte recruitment in inflammatory disease. Mol Med Today 2:198–204
Takaishi H, Taniguchi T, Takahashi A, Ishikawa Y, Yokoyama M (2003) High glucose accelerates MCP-1 production via p38 MAPK in vascular endothelial cells. Biochem Biophys Res Comm 305:122–128
Shanmugam N, Reddy MA, Guha M, Natarajan R (2003) High glucose-induced expression of proinflammatory cytokine and chemokine genes in monocytic cells. Diabetes 1256–1264
Sartipy P, Loskutoff DJ (2003) Expression profiling identifies genes that continue to respond to insulin in adipocytes made insulin-resistant by treatment with tumor necrosis factor-alpha. J Biol Chem 278:52298–52306
Rovin BH, Lu L, Saxena R (1999) A novel polymorphism in the MCP-1 gene regulatory region that influences MCP-1 expression. Biochem Bioph Res Comm 259:344–348
Sylvester I, Suffredini AF, Boujoukos AJ et al. (1993) Neutrophil attractant protein-1 and monocyte chemoattractant protein-1 in human serum. Effects of intravenous lipopolysaccharide on free attractants, specific IgG autoantibodies and immune complexes. J Immunol 151:3292–3298
Ueda A, Okuda K, Ohno S, Shirai A, Igarashi T, Matsunaga K (1994) NF-kappa B and Sp1 regulate transcription of the human monocyte chemoattractant protein-1 gene. J Immunol 153:2052–2063
Kim HL, Lee DS, Yang SH et al. (2002) The polymorphism of monocyte chemoattractant protein-1 is associated with the renal disease of SLE. Am J Kidney Dis 40:1146–1152
Muhlbauer M, Bosserhoff AK, Hartmann A et al. (2003) A novel MCP-1 gene polymorphism is associated with hepatic MCP-1 expression and severity of HCV-related liver disease. Gastroenterology 125:1085–1093
Szalai C, Duba J, Prohatzka Z et al. (2001) Involvement of polymorphisms in the chemokine system in the susceptibility for coronary artery disease (CAD). Coincidence of elevated Lp(a) and MCP-1–2518 G/G genotype in CAD patients. Atherosclerosis 158:233–239
Szalai C, Kozma GT, Nagy A et al. (2001) Polymorphism in the gene regulatory region of MCP-1 is associated with asthma susceptibility and severity. J Allergy Clin Immunol 108:375–381
Winkelmann BR, März W, Boehm BO et al.; LURIC Study Group (LUdwigshafen RIsk and Cardiovascular health) (2001) Rationale and design of the LURIC study—a resource for functional genomics, pharmacogenomics and long-term prognosis of cardiovascular disease. Pharmacogenomics 2 [Suppl 1]:S9–S73
Nakai Y, Fukushima M, Nakaishi S et al. (2002) The threshold value for insulin resistance on homeostasis model assessment of insulin sensitivity. Diabet Med 19:344–348
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2002) Report of the expert committee on the diagnosis and classification of diabetes mellitus [from the American Diabetes Association, ADA]. Diabetes Care 25 [Suppl 1]:S1–S20
World Health Organization (1999) Definition, diagnosis and classification of diabetes mellitus and its complications. Report of a WHO consultation. Part 1 Diagnosis and classification of diabetes mellitus WHO/NCD/NCS/99. World Health Organization, Geneva
Taubert G, Winkelmann BR, Schleiffer T et al. (2003) Prevalence, predictors, and consequences of unrecognized diabetes mellitus in 3266 patients scheduled for coronary angiography. Am Heart J 145:285–291
Kowalski J, Okopien B, Madej A et al. (2001) Level of sICAM-1, sVCAM-1 and MCP-1 in patients with hyperlipoproteinemia IIa and -IIb. Int J Clin Pharmacol Ther 39:48–52
Lemos JA de, Morrow DA, Sabatine MS et al. (2003) Association between plasma levels of monocyte chemoattractant protein-1 and long-term clinical outcomes with acute coronary syndromes. Circulation 107:690–695
Piemonti L, Calori G, Mercalli A et al. (2003) Fasting plasma leptin, tumor necrosis factor-α receptor 2, and monocyte chemoattractant protein 1 concentration in a population of glucose-tolerant and glucose intolerant women. Diabetes Care 26:2883–2889
Dandona P, Aljada A, Mohanty P et al. (2001) Insulin inhibits intranuclear nuclear factor kappaB and stimulates IkappaB in mononuclear cells in obese subjects: evidence for an anti-inflammatory effect? J Clin Endocrinol Metab 86:3257–3265
Mazurek T, Zhang L, Zalewski A et al. (2003) Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 108:2460–2466
Smith SR, Bai F, Charbonneau C, Janderova L, Argyropoulos G (2003) A promoter genotype and oxidative stress potentially link resistin to human insulin resistance. Diabetes 52:1611–1618
Acknowledgements
This study was supported by the Teo Rossi di Montelera Foundation, (Lausanne, Switzerland) and the Swiss Cardiology Foundation. E. Simeoni, M. M. Hoffmann and B. R. Winkelmann contributed equally to this work. G. Vassalli and S. Fleury were the recipients of grants from the Swiss National Science Foundation (grant numbers 632-058215 and 3100-64.834.01 respectively). B. O. Boehm was the recipient of a grant from the German Research Foundation (grant number SFB518).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simeoni, E., Hoffmann, M.M., Winkelmann, B.R. et al. Association between the A–2518G polymorphism in the monocyte chemoattractant protein-1 gene and insulin resistance and Type 2 diabetes mellitus. Diabetologia 47, 1574–1580 (2004). https://doi.org/10.1007/s00125-004-1494-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1494-4