Abstract
Haemoglobin A1c (HbA1c) or glycohaemoglobin is one of the most important parameters in the management of patients with diabetes mellitus, but to date there is no international standard for determining HbA1c. Most of the routine HbA1c assays are standardised against one of the local standardisation schemes like the NGSP (USA) and other schemes (Japan, Sweden). Still, results of HbA1c tests diverge considerably, as do the accompanying clinical decision limits.
The IFCC Working Group on HbA1c Standardisation has developed a reference method and also set up a reference system for HbA1c, in which the analyte is defined as β-N-glycated haemoglobin. This reference system consists of a network of reference laboratories that uses the reference methods and certified reference materials for optimal measurement of HbA1c in human blood. The main task of the network is to assign values to secondary reference materials, to be used by manufacturers of routine HbA1c assays to calibrate their assays. The high specificity of the reference method results in lower HbA1c values in blood samples, since the unspecific components falsely identified as HbA1c in routine methods are not measured by the reference method. The reference range for the new reference method was determined as 3 to 4% and the clinical decision limits were translated from existing guidelines: goal of treatment 5% HbA1c, change of therapy advised at HbA1c greater than 6%. Despite these lower values, worldwide implementation of the IFCC reference system for HbA1c is recommended, in order to end the great divergence in HbA1c results, with which physicians and patients are confronted today.
Similar content being viewed by others
Introduction
In diabetes mellitus, haemoglobin A1c (HbA1c) or glycohaemoglobin is the most important parameter in monitoring the degree of metabolic control obtained by patients [1, 2]. The amount of HbA1c reflects the mean glucose concentration over the previous two to three months and is as such an independent parameter of carbohydrate metabolism. Reproducibility, that is long-term comparability of the values within one individual patient, is therefore an absolute necessity. After publication of the Diabetes Complications and Control Trial (DCCT) [3] and the United Kingdom Prospective Study of Diabetes (UKPDS) [4] HbA1c was introduced as a risk parameter for monitoring the potential development of late diabetic complications. It was in that context that accuracy became important to permit the use of HbA1c as a treatment target in diabetes management.
At present, more than 20 different HbA1c methods are in use, based on three different assay principles (cation exchange chromatography, affinity chromatography and immune turbidimetry), and all yielding different HbA1c results. Harmonisation, comparability and standardisation of HbA1c results have therefore become an issue, mostly covered by local initiatives.
The three major HbA1c harmonisation schemes include: the National Glycohemoglobin Standardisation Program (NGSP) in the United States, the scheme of the Japanese Diabetes Society (JDS) and the MonoS-method (Sweden), with considerable divergence still existing between HbA1c results [1].
The International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) has therefore installed a Working Group on HbA1c Standardisation, and developed an international reference system for HbA1c [5]. The introduction of this reference system worldwide should result in the same HbA1c values all over the world. The HbA1c values in the IFCC reference system are, however, lower than the results clinicians are using today. The worldwide implementation of the IFCC reference system is recommended, in order to establish international compatibility of data, but doing this will make it necessary to define new clinical decision limits.
Methods for HbA1c determination
The basis for the first commercial methods of measuring HbA1c was the method described by Trivelli et al. [6]. They used the resin Bio-Rex 70 (BioRad Laboratories, Hercules, Calif., USA) to separate HbA1c from HbA0 by cation exchange chromatography. HbA1c, a peak in the chromatogram, was later defined as the adduct of glucose and the N-terminal amino acid valine of the β-chain of haemoglobin A0 [7]. This glycation process (old term glycosylation) is a non-enzymatic reaction. Glycation of the N-terminal valine of the β-chain of haemoglobin results in a very small change in the iso-electric point of this modified haemoglobin (HbA1c) so that separation between HbA1c and the non-glycated haemoglobin (HbA0) is possible.
With the growing interest in HbA1c as a parameter of glycaemic control, the number of assays and methods increased. Ion exchange high-performance liquid chromatography (HPLC) systems were the first automated systems totally dedicated to HbA1c determination and newly developed assays were frequently calibrated to methods already in use in clinical laboratories. However, these early ion exchange HPLC methods were no ‘gold standards’, although they paved the way for further development.
Progress in the composition of the resins used for ion exchange chromatography has led to the development of far more specific resins (less interfering substances under the HbA1c peak) and better separation of HbA1c and HbA0. Examples are the MonoS resin [8] (strong methyl sulphonate cation exchanger on monobeads, Amersham Bioscience, Uppsala, Sweden) used as the reference method in Sweden and the KO500 high-resolution ion exchange chromatography method [9] developed by the Japanese Society of Clinical Chemistry (JSCC).
Next to the development of more precise ion exchange chromatographic methods, immune turbidimetric assays were also developed [10], with the same glycation at the β-terminal of haemoglobin as the antigenic property. Although most immune turbidimetric assays were more specific in nature, the lack of primary or even secondary reference materials meant that they had to be calibrated back to unspecific cation exchange HPLC systems.
A third group of assays is based on the principle of specific and reversible binding of the 1,2-cis diol groups of glycated haemoglobin to immobilised boronate; this is called affinity separation [11]. The most frequently used form is affinity chromatography, both manual chromatography and affinity HPLC. As affinity chromatography in principle measures not only the specific glycation on the β-N-terminal, but also on the α-N-terminal and ε-residues of the total haemoglobin molecule, the end-result is total glycated haemoglobin or glycohaemoglobin. Normally, the measurement of glycohaemoglobin results in a higher value than the specific measurement of HbA1c. Nevertheless, results of glycohaemoglobin are very frequently converted to and presented as ‘HbA1c’.
Standardisation of HbA1c assays
HbA1c was first used as an independent parameter of glycaemic control, therefore reproducibility was more important than accuracy. However, after publication of several clinical studies, individual numbers became important and thus harmonisation became an important analytical issue.
To standardise results of different assays of the same analyte, three approaches can be used:
-
1.
Harmonisation-by-calibration: a single sample, with an assigned value, is used to recalibrate all routine assays with much less divergence in results than without calibration. In the case of HbA1c such a single sample with assigned values doesn’t exist.
-
2.
Harmonisation-by-method comparison: a so called designated comparison method (DCM) is introduced, to which all other assays are recalibrated by means of extensive method comparison and regression analysis. Use of DCMs for standardisation is specially recommended if the analyte to be measured, like HbA1c, is heterogenous, is measured by different methodologies through different properties of the molecule and if reference materials are not available.
-
3.
Standardisation by introduction of a reference system: in the reference systems, secondary reference materials are produced, to be used by all manufacturers of routine assays to calibrate their own methods. In the case of HbA1c, the introduction of the reference system included the definition of the analyte to be measured, the preparation of reference materials, the development of a reference method and the validation of the system through a network of reference laboratories.
Harmonisation-by-calibration has not gained much support, although good results have been found. The standardisation system of the Japanese Diabetes Society (JDS) uses a set of calibrators to harmonise results in Japan. All other known local standardisation schemes (NGSP in the US and the Swedish system) are based on the harmonisation-by-method comparison. The challenge of international standardisation was taken by the IFCC Working Group on HbA1c Standardisation, who developed a reference system for HbA1c.
The NGSP standardisation scheme
The NGSP [12] was established in the USA in 1994 after the publication of the results of the DCCT study, which showed the curve-linear relationship between HbA1c and risks for development and/or progression of diabetic complications. The implementation of treatment goals based on the results of the DCCT in clinical settings made it necessary to harmonise HbA1c results.
The NGSP was a follow-up of the American Association of Clinical Chemistry (AACC) Subcommittee on Glycohemoglobin Standardisation, which specifically tried to harmonise with regard to the DCCT results. In their final report however, the AACC Subcommittee stated that the method used in the DCCT study was not suitable as a primary reference method and that a purified standard for this method could not be prepared. Nevertheless, the results of the DCCT were transferable. So, a standardisation programme (NGSP) similar to the cholesterol network, was proposed as interim anchor, while investigations proceeded to prepare purified standards and to develop a primary reference method (in the IFCC Working Group on HbA1c Standardisation).
So the results of a clinical study, which in the original publication focussed on glucose as treatment goal and only later on specific HbA1c levels, were the starting point of an analytical harmonisation scheme. In the NGSP, the anchor is the very unspecific Bio-Rex 70 ion exchange HPLC in the Central Primary Reference Laboratory (CPRL) and the backup Primary Reference Laboratories (PRL). A network of so-called Secondary Reference Laboratories (SRL) was established to assist manufacturers with calibration to the DCCT value, as well as serving as comparison methods for NGSP certification. These SRLs use routine HbA1c methods of various method types (ion-exchange HPLC, affinity HPLC and immunoassay), which are convenient and robust, provide excellent analytical performance in these laboratories and are calibrated to the CPRL method. The Network Laboratories are monitored monthly by sample exchange with the CPRL [13]. Nevertheless, due to the design of the PRL-SRL structure, a significant difference exists between the results per SRL (±3% at 6% and 9% HbA1c) and thus in the results of the routine method adjusted to these particular SRL-values.
JDS/JSCC standardisation scheme
The basis of the JDS/JSCC standardisation scheme is a set of national calibrators [14]. In 1995 the JDS developed a first set of national calibrators, called JDS Calibrator lot 1, which was recommended to be used for the calibration of all routine HbA1c assays in Japan. The calibrator values were consensus values, assigned with the HPLC ion exchange chromatography methods of TOSOH and Kyoto Daiichi. In recent years, the Japanese standardisation scheme has further evolved. The JSCC developed a high-resolution ion exchange chromatography HPLC method named KO500 [9] and a second set of national calibrators (deep-frozen blood) called JDS/JSCC Calibrator lot 2. The KO500 method was used to assign target values to the lot 2 calibrators; in order to keep consistency in HbA1c values, the calibration of the KO500 method was adjusted to the first lot of JDS calibrators. The value assignment to the lot 2 calibrators was performed in the four Reference Laboratories of the JDS/JSCC.
Swedish standardisation scheme
The Swedish standardisation scheme uses the MonoS HPLC method as DCM for the harmonisation of HbA1c measurements [8]. Split samples of fresh EDTA blood are distributed once a month to 40 hospitals using different HPLC methods. Five of them are contracted to run the MonoS reference method in a national network. These laboratories are used for calibration of all hospital and point-of-care instruments in Sweden every second year.
The IFFC reference system for HbA1c
All national initiatives were important steps towards improving comparability of HbA1c results. However, national standardisation programmes based on different DCMs cannot replace uniform standardisation which is anchored in a metrologically sound international measurement system comprised of: (i) a clear definition of the analyte based on its molecular structure; (ii) a primary reference material containing the analyte in pure form; (iii) a validated reference method which specifically measures the analyte in human samples; (iv) a global network of reference laboratories to guarantee that the reference method is performed with the necessary analytical quality, and to assign values to matrix-based, secondary reference materials and calibrators.
The IFCC Working Group has developed such a reference system for HbA1c [5]. HbA1c is defined as the stable adduct of glucose to the N-terminal valine of the β-chain of haemoglobin. Primary reference materials of pure HbA1c and pure HbA0 have been prepared [15], and a reference method which specifically measures HbA1c has been developed [16].
The IFCC reference method is done in three steps. Firstly, haemoglobin from washed and lysed erythrocytes is cleaved into peptides by the proteolytic enzyme Endoprotease Glu-C, a serine protease which cleaves peptide bonds C-terminal at glutamic acid. Secondly, the resulting glycated and non-glycated N-terminal hexapeptides of the β-chain are separated from the crude peptide mixture by reversed phase HPLC. Thirdly, the glycated and non-glycated hexapeptides are quantified by mass spectrometry or by capillary electrophoresis with UV detection. The percentage of HbA1c is determined by the ratio of glycated to the sum of glycated and non-glycated β-N-terminal hexapeptides of haemoglobin.
In 2001, the final method was unanimously accepted in a ballot by the national member societies of the IFCC as the “Approved IFCC Reference Method for the measurement of HbA1c in human blood” [17]. The reference system is supported by a global network of HbA1c Reference Laboratories from Europe, Japan and the US which have successfully established the reference method [18].
The high specificity of the reference method results in lower values for HbA1c in patient samples since the unspecific components measured as HbA1c in routine methods are not measured by the reference method. Consequently, the reference range for the new reference method for non-diabetic individuals had to be determined. Samples collected in the Danish Population Study (DiaRisk, Steno Diabetes Center, Copenhagen, Denmark) were analysed. The subjects were non-diabetic according to the current WHO and ADA criteria. The mean value was 3.3% HbA1c and the standard deviation 0.24%. From these data a 95% reference range of 2.84–3.81% (n=120) was then established.
Method comparison with DCMs and routine methods
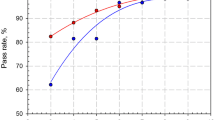
When using the IFCC Reference Method for the calibration of HbA1c routine methods, it is important to realise that the current interpretation of HbA1c results is based on data from tests which were calibrated to DCMs that were less specific than the IFCC Reference Method and therefore generate higher HbA1c values than those which will result if calibration is traced back to the IFCC Reference system. To understand the numerical relationship between the IFCC Reference Method and the DCMs used in the national standardisation schemes, five method-comparison studies were organised from 2001 to 2003 between the IFCC Network of HbA1c Reference Laboratories and the NGSP, JDS/JSCC and the Swedish system. Each study comprised five to eight (pooled) blood samples, and the regression lines between the IFCC and the various standardisation schemes were calculated for each intercomparison study. As no statistical difference between the correlations in the five intercomparison studies was found, all the results (n=28) were combined to calculate the overall regression [19]. This overall regression is called the Master Equation between IFCC and the DCM. The following Master Equations were established, and are depicted in Figure 1:
HbA1c values measured in the five inter-comparison studies by the IFCC Network of Reference Laboratories, the NGSP Network of Secondary Reference Laboratories, the JDS/JSCC Network of Reference Laboratories and the Swedish Reference Laboratory. The lines are the regression lines and the y=x line respectively. The regression lines are: for IFCC (x) vs NGSP (y): y=0.915x+2.15; for IFCC (x) vs JDS/JSCC (y): y=0.927x+1.72; for IFCC (x) vs Sweden/MonoS (y): y=0.989x+0.88. DCM, designated comparison method
-
1.
between IFCC and NGSP: y (NGSP)=0.915x(IFCC)+2.15
-
2.
between IFCC and JDS/JSCC: y (JDS/JSCC)=0.927x(IFCC)+1.724
-
3.
between IFCC and the Swedish MonoS: y (MonoS)=0.989x(IFCC)+0.884
The slope and the intercept of the equation IFCC versus NGSP deviate significantly from 1 and 0 respectively (p<0.001). However, the relationship between the two systems is linear, and there is very little dispersion of the measured values around the regression line. Also the JDS/JSCC-HbA1c values differ significantly from the IFCC-HbA1c values, but, as with the NGSP, a strong linear correlation exists between the two systems. In the Swedish system, only the intercept differs significantly from 0.
Considering the lack of specificity of the DCMs, it is not surprising that all three DCMs generate significantly higher results than the IFCC Reference Method, and that there are also significant differences between the results of the three DCMs. The NGSP generates the highest HbA1c values, because the HbA1c peak of the Bio-Rex 70 method, used as anchor of the NGSP, contains a high proportion of non-HbA1c substances (high intercept) and the peak is not clearly separated from the neighbouring HbA0 peak (slope approx. 0.9). The Japanese KO500 method is a very-high-resolution HPLC, but due to the calibration of this very specific method, with calibrators being assigned values that were assigned with the older HPLC methods from TOSOH and Kyoto Daiichi, the JDS/JSCC values reflect the low specificity of these methods. The results of the JDS/JSCC system are about 0.3% lower than those of the NGSP. The Swedish MonoS system generates the lowest HbA1c values. The HbA1c peak is very homogenous (slope ~1.0), but it contains some interfering substances, resulting in a positive intercept of 0.9 and somewhat higher HbA1c values than measured with the IFCC HbA1c system. In contrast to the DCM methods, new dedicated HPLC systems are presently eliminating many of these interfering adducts by using more modern chromatographic material and improved gradients, but sometimes 20 to 50% of the real measured value has to be added to come up with DCM aligned values.
As with the DCMs, two intensive comparison studies were also organised with all the manufacturers of routine HbA1c assays. In these studies it was shown that all methods, despite their different assay principle, could be standardised by the IFCC HbA1c Reference System, yielding comparable results for all routine methods. In the last years, the IFCC Network of HbA1c Reference Laboratories has made secondary reference material with assigned values available, to be used as IFCC calibrators for manufacturers’ methods. This enables the manufacturers to work within the requirements of the In-Vitro Diagnostic Directive of the European Union, which states that manufacturers have to trace back the calibration of their tests to reference methods or reference materials of higher metrological order if available. In the case of HbA1c, this is the IFCC Reference Method for HbA1c [20].
The DCMs used successfully for harmonising routine HbA1c methods cannot be used for global standardisation. The three different systems all use different, arbitrarily chosen, ion-exchange HPLC methods for comparison and define their own HbA1c as a peak in a chromatogram in a more or less unspecific fashion. Similarly, the Bio-Rex 70 method used as an accuracy base in the NGSP has to be regarded as outdated as its reproducibility is based on the long-term stability of different lots of haemolysates frozen at −80 °C and a temperature-controlled waterbath for the ion exchange HPLC. Despite the large scale use of DCCT-aligned values in the USA, individual values of laboratories participating in proficiency testing differ too much (range 0.4% at 5.0% HbA1c and 1.0% at 11.0% HbA1c), even if they use the same certified method.
The higher specificity of the IFCC reference method has also influenced the relationship between HbA1c and mean glycaemia in the DCCT study. This relationship can be described by a linear regression model: each 1% increase in HbA1c corresponds with an increase in mean plasma glucose of approximately 2 mmol/l plasma glucose. For the DCCT, the correlation is: y (mean glucose, mmol/l)=1.98x (% HbA1c)−4.29. For the IFCC method, the correlation is: y (mean glucose, mmol/l)=1.84x (% HbA1c)−0.01 [21].
Implementation of the IFCC HbA1c reference system
The IFCC Reference System for HbA1c [21] is now being implemented as anchor for the existing DCMs and for the calibration of all manufacturers methods for routine HbA1c assays. However, most routine HbA1c methods still report ‘old’ numbers by using ‘Master Equations’. Against that background, the introduction of the IFCC calibration principle will provide better comparability between routine methods.
For clinical implementation of the IFCC numbers, it is imperative to adopt a global approach, in which clinical diabetes organisations play a vital role. Introduction of IFCC HbA1c values has added value (lower uncertainty, better comparability, same numbers worldwide), but during the transition period, loss of clinical information should be avoided. All clinical trials and existing targets for diabetes treatment must therefore be translated into the new numbering system, yielding new reference ranges and new treatment goals. As the reference range in the IFCC HbA1c Reference System was calculated as 3 to 4 % HbA1c, new target values (Table 1) will have to be calculated.
References
Sacks DB, Bruns DE, Goldstein DE, McLaren NK, McDonald JM, Parrott M (2002) Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem 48:436–472
ADA (2003) Clinical practice guidelines 2003. Diabetes Care 26 [Suppl 1]:S1–S156
The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
UK Prospective Diabetes Study Group (1998) Intensive blood-glucose control with sulfonylureas compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 35). Lancet 352:837–853
Hoelzel W, Miedema K (1996) Development of a reference system for the international standardisation of HbA1c/glycohemoglobin determinations. JIFCC 9:62–67
Trivelli LA, Ranney HM, Lai HT (1971) Hemoglobin components in patients with diabetes mellitus. N Engl J Med 284:353–357
McDonald MJ, Shapiro R, Bleichman M, Salway J, Bunn HF (1978) Glycosylated minor components of human adult haemoglobin: purification, identification and partial structural analysis. J Biol Chem 253:2327–2332
Jeppsson JO, Jerntorp P, Sundkvist G, Englund H, Nylund V (1986) Measurement of haemoglobin A1c by a new liquid chromatographic assay: methodology, clinical utility and relation to glucose tolerance evaluated. Clin Chem 32:1867–1872
Hoshino T, Nakayama T, Kuwa K et al. Reference Method for St-GHbA1c determination. Standard Operating Procedure Version 1.4-2000. JSCC Working Group on SOP for St-GHbA1c Determination
John WG, Gray MR, Bates DL, Beacham J (1993) Enzyme immunoassay: a new method for the estimation of haemoglobin A1c. Clin Chem 39:663–666
Mallia AK, Hermanson GJ, Krohn RI, Fujimoto EK, Smith PK (1981) Preparation and use of a boronic acid affinity support for separation and quantitation of glycosylated haemoglobin. Anal Lett 14:649–661
Little RR, Goldstein DE (1995) Endocrine standardization of glycohemoglobin measurements. Anal Chem 67:393R–397R
Little RR, Rohlfing CL, Wiedmeyer HM, Myers GL, Sacks DB, Goldstein DE (2001) The national glycohemoglobin standardization program: a five-year progress report. Clin Chem 47:1985–1992
Shima K, Endo J, Oimomi M et al. (1994) Inter-laboratory difference in HbA1c measurement in Japan. A report of the committee on inter-laboratory standardisation of HbA1c determinations, the Japan Diabetes Society. J Japan Diab Soc 37:855–864
Finke A, Kobold U, Hoelzel W, Weykamp C, Jeppsson JO, Miedema K (1998) Preparation of a candidate primary reference material for the international standardisation of HbA1c determinations. Clin Chem Lab Med 36:299–308
Kobold U, Jeppsson JO, Dülffer T, Hoelzel W, Miedema K (1997) Candidate reference methods for HbA1c based on peptide mapping. Clin Chem 43:1944–1951
Jeppsson JO, Kobold U, Miedema K et al. (2002) Approved IFCC reference method for the measurement of HbA1c in human blood. Clin Chem Lab Med 40:78–89
Jeppsson JO, Hoelzel W, Kobold U et al. (1998) International network of reference laboratories for the determination of HbA1c. Clin Chem 44 [S6]:A22 (Abstract)
Hoelzel W, Weykamp C, Jeppsson JO et al. (2004) The IFCC reference system for the measurement of HbA1c in human blood and the national standardization schemes in the USA, Japan and Sweden—a method comparison study. Clin Chem 50:166–174
Müller MM (2000) Implementation of reference systems in laboratory medicine. Clin Chem 46:1907–1909
Mosca A, John WG (2001) IFCC reference system for glycohaemoglobin/HbA1c standardisation. In: John WG (ed) Monitoring glycaemic control in the diabetic patient. Excerpta Medica, London, pp 123–140
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miedema, K. Towards worldwide standardisation of HbA1c determination. Diabetologia 47, 1143–1148 (2004). https://doi.org/10.1007/s00125-004-1453-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1453-0