Abstract
Aims/hypothesis
We investigated the pharmacological properties of two novel ATP sensitive potassium (KATP) channel openers, 6-Chloro-3-isopropylamino-4H-thieno[3,2-e]-1,2,4-thiadiazine 1,1-dioxide (NNC 55-0118) and 6-chloro-3-(1-methylcyclopropyl)amino-4H-thieno[3,2-e]-1,2,4-thiadiazine 1,1-dioxide (NN414), on the cloned cardiac (Kir6.2/SUR2A), smooth muscle (Kir6.2/SUR2B) and pancreatic beta cell (Kir6.2/SUR1) types of KATP channel.
Methods
We studied the effects of these compounds on whole-cell currents through cloned KATP channels expressed in Xenopus oocytes or mammalian cells (HEK293). We also used inside-out macropatches excised from Xenopus oocytes.
Results
In HEK 293 cells, NNC 55-0118 and NN414 activated Kir6.2/SUR1 currents with EC 50 values of 0.33 µmol/l and 0.45 µmol/l, respectively, compared with that of 31 µmol/l for diazoxide. Neither compound activated Kir6.2/SUR2A or Kir6.2/SUR2B channels expressed in oocytes, nor did they activate Kir6.2 expressed in the absence of SUR. Current activation was dependent on the presence of intracellular MgATP, but was not supported by MgADP.
Conclusion/interpretation
Both NNC 55-0118 and NN414 selectively stimulate the pancreatic beta-cell type of KATP channel with a higher potency than diazoxide, by interaction with the SUR1 subunit. The high selectivity and efficacy of the compounds could prove useful for treatment of disease states where inhibition of insulin secretion is beneficial.
Similar content being viewed by others
Potassium (K+) channel openers are a structurally diverse group of compounds which share the common property that they are capable of activating potassium channels [1]. The most clinically important are those that are selective for the ATP-sensitive potassium (KATP) channel, which we refer to here as KCOs. The hallmark of the KATP channel is that it is inhibited by intracellular ATP and activated by MgADP, thus enabling it to couple the metabolic state of the cell to the membrane potential and electrical activity (by sensing changes in intracellular ATP and ADP). The KATP channel plays a key role in glucose-dependent insulin secretion from pancreatic beta cells [2]. KATP channels are open at low glucose concentrations, as metabolism is low, but shut when glucose uptake and metabolism are stimulated by an increase in the plasma glucose concentration. This leads to membrane depolarisation, activation of voltage-gated Ca2+ channels, Ca2+ influx and, in turn, insulin secretion. Activation of the KATP channel by KCOs hyperpolarizes the pancreatic beta cell and suppresses insulin secretion even in the presence of glucose.
Diazoxide is the best known KCO capable of opening pancreatic beta cell KATP channels and inhibiting insulin secretion [3]. It has also been reported to reduce weight gain in obese Zucker rats [4], prevent development of insulin resistance in a rat model [5], and preserve residual insulin secretion in Type 1 diabetic humans [6]. Potentially, therefore, KCOs selective for the pancreatic beta cell KATP channel could be of clinical value for treating disease states in which suppression of insulin secretion and beta-cell activity are beneficial.
KATP channels consist of pore-forming Kir6.x subunits that associate with different kinds of regulatory sulphonylurea receptor subunits: SUR1, SUR2A or SUR2B [7]. The beta-cell KATP channel is composed of Kir6.2 and SUR1 [8, 9], the cardiac type of Kir6.2 and SUR2A [10], and the vascular smooth muscle type of Kir6.1 and SUR2B [11]. It is believed that Kir6.2 and SUR2B make up some smooth muscle KATP channels [12], and that both Kir6.2/SUR1 and Kir6.2/SUR2B combinations are found in neurones [13]. SUR acts as a channel regulator, with the different SUR subtypes conferring differential sensitivity to the inhibitory effects of sulphonylurea drugs and the stimulatory actions of KCOs and MgADP [7, 14]. For example, diazoxide strongly activates beta cell and smooth muscle KATP channels but has only a weak stimulatory effect on cardiac KATP channels [15, 16, 17, 18].
The different composition, tissue expression patterns, and functional roles of the KATP channel subtypes suggests that KCOs might be useful in a broad spectrum of therapeutic applications [19]. However, very few KCOs are in clinical use today. Diazoxide is used to suppress excessive insulin secretion, such as that which occurs in congenital hyperinsulinism, but it has many undesired side-effects due to its action on cardiovascular KATP channels. Minoxidil sulphate is used to stimulate hair growth, and nicorandil is used in the treatment of angina. The clinical use of KCOs is limited by their relatively low affinity and lack of specificity, which results in diffuse side-effects in several tissues. It is therefore important to identify compounds that possess high affinity and selectivity for the different SUR subtypes.
In this paper, we report on the functional properties and selectivity of two new KCOs, the diazoxide analogues 6-chloro-3-isopropylamino-4H-thieno[3,2-e]-1,2,4-thiadiazine 1,1-dioxide (NNC 55-0118) and 6-chloro-3-(1-methylcyclopropyl)amino-4H-thieno[3,2-e]-1,2,4-thiadiazine 1,1-dioxide (NN414). Their chemical structures are compared to those of diazoxide and pinacidil in Fig. 1.
Materials and methods
Molecular biology
For excised patch studies, mouse Kir6.2 (Genbank D50581, [8, 9]), rat SUR1 (Genbank L40624; [20]), SUR2A (Genbank D83598, [10]) and SUR2B (Genbank D86038, [12]) cDNAs were cloned in the pBF vector. A truncated form of Kir6.2 (Kir6.2ΔC36), which lacks the C-terminal 36 amino acids and forms functional channels in the absence of SUR, was also prepared [21]. Experiments on intact oocytes were carried out using human clones of Kir6.2 (Genbank D50582), SUR2A (Genbank AF061323, [22]) and SUR2B (Genbank AF061324, [22]) which were all cloned at Novo Nordisk, and rat SUR1 as above. The amino acid sequence of the human clones differs by less than 4% from their rodent counterparts.
Capped mRNA was prepared using the mMESSAGE mMACHINE large scale in vitro transcription kit (Ambion, Austin, Tex., USA) or the mRNA capping kit (Stratagene, La Jolla, Calif., USA) [23].
Oocyte collection
Female Xenopus laevis were anaesthetized with MS222 (2 g/l added to the water). From each animal one ovary was removed via a mini-laparotomy, the incision sutured and the animal allowed to recover. Once the wound had completely healed, the second ovary was removed in a similar operation and the animal was then killed by decapitation whilst under anaesthesia. Immature stage V to VI oocytes were incubated for 60 min with 1.0 mg/ml collagenase (Sigma, type V) and manually defolliculated. Oocytes were either injected with about 1 ng Kir6.2ΔC36 mRNA or coinjected with about 0.1 ng Kir6.2 mRNA and about 2 ng of mRNA encoding wild-type or chimeric SUR. The final injection volume was 50 nl/oocyte. Isolated oocytes were maintained in Barth's solution and studied 1 to 7 days after injection [23].
Oocyte Electrophysiology: two electrode voltage clamp (TEVC)
Whole-cell currents were recorded at 20 to 24°C using a two-electrode voltage-clamp amplifier (Warner OC725) and analysed using in-house software [24]. Currents were filtered at 0.1 kHz and digitised at 0.24 kHz. TEVC electrodes were pulled from thin-walled borosilicate glass and had resistances between 0.4 and 1 MΩ when filled with 3 mol/l KCl. KATP currents were activated by metabolic inhibition with 3 mmol/l azide and currents were recorded in extracellular solution containing (mmol/l): KCl 90, MgCl2 2.5, HEPES 10 (pH 7.2 with KOH). The holding potential was set to the zero current potential (−10 or −20 mV). Hyperpolarizations of 10 or 20 mV amplitude of 3 s duration were applied every 30 s. NN414 and NNC 55-0118 were prepared as 200 mmol/l stock solutions in DMSO [25]. In control experiments, the maximal DMSO concentration applied (0.15%) was without effect on the KATP current.
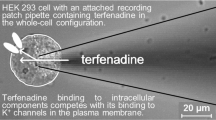
Electrophysiology: mammalian cells
Currents from HEK293 cells stably expressing human (hu) SUR1 and huKir6.2 were recorded and digitized using an EPC9 patch-clamp amplifier (List Electronik, Darmstadt, Germany) and Pulse+PulseFit v.8.07 Software (HEKA Elektronik, Lambrecht/Pfalz, Germany) on a Macintosh computer. Cells were dialyzed with intracellular solution containing: (in mmol/l): KCl 120, CaCl2 2, MgCl2 1, HEPES 20, EGTA 5 and K2ATP 0.3 (pH 7.3 with KOH). The bath solution contained (in mmol/l): NaCl 140, KCl 5, CaCl2 1.8, MgCl2 1, HEPES 10 and mannitol 20 (pH 7.4 with NaOH). The cells were clamped at −70 mV and currents were evoked by repetitive 250 ms, 10 mV depolarizing voltage steps. Drugs were applied by a gravity-driven perfusion system placed less than 75 µm from the clamped cell.
Ocyte Electrophysiology: macropatches
Patch pipettes were pulled from thick-walled borosilicate glass and had resistances of 250 to 500 kΩ when filled with pipette solution. Macroscopic currents were recorded from giant excised inside-out patches at a holding potential of 0 mV and at 20 to 24°C [23]. Currents were evoked by repetitive 3 s voltage ramps from −110 mV to +100 mV and recorded using an EPC7 patch-clamp amplifier (List Electronik, Darmstadt, Germany). They were filtered at 0.2 kHz, digitised at 0.4 kHz using a Digidata 1200 Interface and analysed using pClamp software (Axon Instruments, Foster City, Calif., USA).
The pipette (external) solution contained (mmol/l): 140 KCl, 1.2 MgCl2, 2.6 CaCl2, 10 HEPES (pH 7.4 with KOH). The intracellular (bath) solution contained (mmol/l): 110 KCl, 1.4 MgCl2, 10 EGTA, 10 HEPES (pH 7.2 with KOH; final [K+] ~140 mmol/l). Solutions containing ATP or ADP were made up fresh each day. The pH of the solution was readjusted after addition of the drug and/or nucleotide. Rapid exchange of solutions was achieved by positioning the patch in the mouth of one of a series of adjacent inflow pipes placed in the bath.
Data analysis
Concentration–response data were fit to the following equation:
where I is the current amplitude in the presence of the drug; Imax is the current in the absence of drug (for inhibitory responses) or the current in the presence of a saturating drug concentration (for activation responses); [drug] is the concentration of NNC55-0118 or NN414; X is the drug concentration that causes half maximal activation (EC50) or inhibition (IC50), h is the Hill coefficient (slope factor), L is the maximum activation (for activation) or zero (for inhibition). Data were fit using Microcal Origin software.
The slope conductance for macropatches was measured by fitting a straight line to the current-voltage relation between −20 mV and −100 mV. Conductance was measured from an average of five consecutive ramps in each solution. Responses to NNC 55-0118, NN414 or nucleotides (G) were expressed as a fraction of that in control solution (GC) without added drugs or nucleotides.
All data are shown as mean ±1 standard error of the mean. Statistical significance was tested using Students t test. A p value of less than 0.05 was considered to be statistically significant.
Results
Effects on pancreatic beta-cell type KATP channels (Kir6.2/SUR1)
NN414 potently activates an outward current in HEK293 cells stably expressing the pancreatic beta-cell type of KATP channel, Kir6.2/SUR1 (Fig. 2A). This current was blocked by glibenclamide, indicating that it flows through the KATP channel. Similar results were observed with NNC 55-0118 (data not shown). Both NN414 and NNC 55-0118 were considerably more potent than diazoxide: the EC 50 for NNC 55-0118 was 0.33±0.04 µmol/l (n=4), for NN414 was 0.45±0.1 µmol/l (n=3) and for diazoxide was 31±5 µmol/l, n=3) (Fig. 2B).
Effects of NNC 55-0118, NN414 and diazoxide on whole cell K+ currents in a HEK293 cell line stably expressing the pancreatic beta cell type of KATP channel, Kir6.2/SUR1. (A) Whole-cell currents recorded from an HEK293 cell stably expressing Kir6.2/SUR1. Currents were evoked by 10 mV depolarizing steps from a holding potential of −70 mV every 10 s. Horizontal bars indicate application of NNC 55-0118 (10 µmol/l), diazoxide (300 µmol/l) and glibenclamide (5 µmol/l). (B) Concentration-activation curves for NN414, NNC 55-0118 and diazoxide. The whole-cell current evoked by a 10 mV step in the presence of the drug (I) is expressed as a fraction of the current at the maximal concentration of the drug (Imax). The lines are the best fit to equation 1 (Methods) with: NNC 55-0118, EC 50 = 330±40 nmol/l, h=1.9±0.4 (n=3); NN414, EC 50 =450±100 nmol/l, h=1.5±0.4 (n=4); and diazoxide, EC 50 =31±5 µmol/l, h=1.5±0.3 (n=4)
Activation of Kir6.2/SUR1 currents was analyzed in more detail in giant inside-out patches excised from Xenopus oocytes co-expressing Kir6.2 and SUR1, or expressing a truncated form of Kir6.2 (Kir6.2ΔC36) that is able to express independently of SUR. As KCOs usually require MgATP to support their action, we tested the effects of NNC 55-0118 and NN414 in the presence of 100 µmol/l MgATP. This ATP concentration blocked Kir6.2ΔC36 currents by 43±3% (n=16) and Kir6.2/SUR1 currents by 83% ± 2% (n=16). Both NNC 55-0118 and NN414 rapidly and reversibly activated Kir6.2/SUR1 currents pre-blocked with 100 µmol/l MgATP (Fig. 3A,B left). However, neither drug was able to activate Kir6.2ΔC36 currents (Fig. 3A,B right), indicating that SUR1 is necessary for the action of the drug. Mean data are given in Fig. 3C,D.
Effect of NNC 55-0118 and NN414 on Kir6.2Δ36 and Kir6.2/SUR1 currents. (A, B) Macroscopic currents recorded from inside-out patches in response to a series of voltage ramps from −110 mV to +100 mV from oocytes co-expressing Kir6.2 and SUR1 or expressing Kir6.2ΔC36. MgATP and NNC 55-0118 (A) or NN414 (B) were added to the intracellular solution as indicated by the horizontal bars. The dashed horizontal line indicates the zero current level. (C) Mean macroscopic slope conductances (G) in the presence of: 100 µmol/l NNC 55-0118 and no nucleotide (white columns); 100 µmol/l MgATP (vertically striped columns); 100 µmol/l MgATP +100 µmol/l NNC 55-0118 (black columns); 100 µmol/l MgADP (horizontally striped columns) or 100 µmol/l MgADP +100 µmol/l NNC 55-0118 (grey columns). Data are expressed as a fraction of the mean slope conductance in control solution (no additions) (GC). The vertical bars indicate 1 SEM and the dashed line indicates the conductance in control solution (no additions). n=5–16 in each column. *p<0.01, NNC 55-0118 vs control and **p<0.001, MgATP + NNC 55-0118 vs MgATP. (D) Mean macroscopic slope conductances (G) in the presence of: 100 µmol/l NN414 and no nucleotide (white columns); 100 µmol/l MgATP (vertically striped columns); 100 µmol/l MgATP +100 µmol/l NN414 (black columns); 100 µmol/l MgADP (horizontally striped columns) or 100 µmol/l MgADP +100 µmol/l NN414 (grey columns). Data are expressed as a fraction of the mean slope conductance in control solution (no additions) (GC). The vertical bars indicate 1 SEM and the dashed line indicates the conductance in control solution (no additions). n=5–11 in each column. *p<0.001, MgATP + NN414 vs MgATP
We next explored whether MgADP was necessary for the activation of Kir6.2/SUR1 currents by NNC 55-0118 and NN414, by testing the efficacy of the drug in the absence of added nucleotide or in the presence of 100 µmol/l MgADP. The drugs failed to activate in the absence of nucleotide and did not increase the current further in the presence of MgADP (Fig. 3C,D). This is in contrast to what is observed for the "classical" KCO diazoxide, which is able to activate Kir6.2/SUR1 and Kir6.2/SUR2A currents in the presence of MgADP [16, 26, 27]. These data suggest that the drugs interact directly with the SUR1 subunit of the KATP channel to activate the hyperpolarizing K+ current leading to decreased beta-cell electrical activity and insulin secretion.
Effects on cardiac (Kir6.2/SUR2A) and smooth muscle (Kir6.2/SUR2B) type KATP channels
We then explored the effect of NNC 55-0118 and NN414 on Kir6.2/SUR2A (cardiac type) or Kir6.2/SUR2B (smooth muscle type) KATP channels expressed in Xenopus oocytes, initially by TEVC in intact oocytes (Fig. 4). Kir6.2/SUR2B currents were robustly activated by 3 mmol/l azide. The current amplitude elicited by a +10 mV step from −10 mV was 550±61 nA (n=15) and 25±2 for uninjected oocytes. Kir6.2/SUR2A currents were not activated by 3 mmol/l azide (n=12, data not shown), and 1 µmol/l of the potassium channel opener P1075 was therefore also added. Interestingly, NN414 inhibited both Kir6.2/SUR2A and Kir6.2/SUR2B currents pre-activated in this way (Fig. 5A). Concentration-inhibition curves gave IC 50 values of 10±2 µmol/l and 7.1±0.8 µmol/l for Kir6.2/SUR2A (n=4) and Kir6.2/SUR2B (n=4), respectively (Fig. 5B).
NNC 55-0118 and NN414 fail to activate KATP currents in oocytes expressing either Kir6.2/SUR2A or Kir6.2/SUR2B. Whole-cell currents recorded in TEVC from oocytes co-expressing Kir6.2 with SUR2A (left) or SUR2B (right) at a holding potential of −10 mV. NNC 55-0118 (1 or 100 µmol/l, A) and NN414 (1 or 100 µmol/l, C) fail to activate Kir6.2/SUR2A, whereas P1075 (10 µmol/l) induced a large current. All drugs were applied in the presence of 3 mmol/l azide. Likewise, neither NNC 55-0118 (1 or 100 µmol/l, B) nor NN414 (1 or 100 µmol/l, D) activates Kir6.2/SUR2B currents but P1075 (10 µmol/l) does activate the channel
NN414 potently antagonizes whole-cell currents from oocytes expressing Kir6.2/SUR2A or Kir6.2/SUR2B. (A) Representative time course of NN414 induced block of Kir6.2/SUR2B current activated by Na-azide. Currents were evoked by 10 mV hyperpolarizing steps from a holding potential of −10 mV every 30 s. (B) Concentration-response relationships for the effect of NN414 on whole-cell KATP currents recorded in TEVC from oocytes expressing Kir6.2/SUR2A or Kir6.2/SUR2B. KATP currents were activated by 3 mmol/l azide and 1 µmol/l P1075 (Kir6.2/SUR2A) or by 3 mmol/l azide alone (Kir6.2/SUR2B). The whole-cell current in the presence of NN414 is expressed as a percentage of that in its absence. The lines are the best fit to equation 1 (Methods) with: for Kir6.2/SUR2A, IC 50 =10±2 µmol/l, h =0.7±0.09 (n=4); and for Kir6.2/SUR2B: IC 50 =7.1±0.8 µmol/l, h =0.8±0.07 µmol/l (n=3)
We next examined the effects of NNC 55-0118 and NN414 on Kir6.2/SUR2A and Kir6.2/SUR2B channels in inside-out membrane patches. Neither NNC 55-0118 nor NN414 had any effect on Kir6.2/SUR2A and Kir6.2/SUR2B channels pre-blocked by 100 µmol/l MgATP (Fig. 6A,B). Mean data are given in Fig. 6C,D, which show that in the presence of 100 µmol/l MgATP these drugs have neither a stimulatory nor an inhibitory effect. Likewise, when Kir6.2/SUR2A or SUR2B KATP channels were pre-activated by 100 µmol/l MgADP no significant (p>0.05) change in current amplitude was observed with either 100 µmol/l NNC 55-0118 or NN414.
Effect of NNC 55-0118 and NN414 on Kir6.2/SURA and Kir6.2/SUR2B currents. (A, B) Macroscopic currents recorded from inside-out patches in response to a series of voltage ramps from −110 mV to +100 mV from oocytes co-expressing Kir6.2 and either SUR2A or SUR2B. MgATP (100 µmol/l), NNC 55-0118 (100 µmol/l, A) and NN414 (100 µmol/l, B) were added to the intracellular solution as indicated by the horizontal bars. The dashed horizontal line indicates the zero current level. (C) Mean macroscopic slope conductances (G) in the presence of: 100 µmol/l NNC 55-0118 and no nucleotide (white columns); 100 µmol/l MgATP (vertically striped columns); 100 µmol/l MgATP +100 µmol/l NNC 55-0118 (black columns); 100 µmol/l MgADP (horizontally striped columns) or 100 µmol/l MgADP +100 µmol/l NNC 55-0118 (grey columns). Data are expressed as a fraction of the mean slope conductance in control solution (no additions) (GC). The vertical bars indicate 1 SEM and the dashed line indicates the conductance in control solution (no additions). n=5–11 in each column. *p<0.001, NNC 55-0118 vs control. (D) Mean macroscopic slope conductances (G) in the presence of: 100 µmol/l NN414 and no nucleotide (white columns); 100 µmol/l MgATP (vertically striped columns); 100 µmol/l MgATP +100 µmol/l NN414 (black columns); 100 µmol/l MgADP (horizontally striped columns) or 100 µmol/l MgADP +100 µmol/l NN414 (grey columns). Data are expressed as a fraction of the mean slope conductance in control solution (no additions) (GC). The vertical bars indicate 1 SEM and the dashed line indicates the conductance in control solution (no additions). n=5–11 in each column. *p<0.01, NN414 vs control
In contrast, we found that in the absence of added nucleotide, both drugs had a clear inhibitory effect on Kir6.2/SUR2A and Kir6.2/SUR2B currents (white bars, Fig. 6C,D). NNC 55-0118 (100 µmol/l) blocked Kir6.2/SUR2A currents by 35±6% (n=7) and Kir6.2/SUR2B currents by 29±6% (n=7); and NN414 (100 µmol/l) inhibited Kir6.2/SUR2A currents by 37±7% (n=9) and Kir6.2/SUR2B currents by 19±5% (n=7).
Discussion
The results presented here show that two novel KCOs, NNC 55-0118 and NN414, selectively activate Kir6.2/SUR1, the pancreatic beta-cell type of KATP channel. They are about 100-fold more potent than diazoxide when applied to HEK293 cells stably expressing the human beta cell KATP channel (Kir6.2/SUR1). When Kir6.2ΔC36 was expressed in the absence of SUR1 neither compound had any effect on the KATP current, suggesting that channel activation is mediated by interaction of the drug with SUR1. Activation of Kir6.2/SUR1 currents was dependent on intracellular MgATP, but in contrast to diazoxide, neither drug was effective in the presence of MgADP. The drugs were effective in both the whole-cell and inside-out configurations, and are thus able to reach their binding site when applied to either side of the membrane.
Neither compound-activated Kir6.2/SUR2A (cardiac type) or Kir6.2/SUR2B (smooth muscle type) KATP channels in intact oocytes. Instead, they inhibited Kir6.2/SUR2A and Kir6.2/SUR2B, with IC 50 values of 10 and 7 µmol/l, respectively. Interestingly, although both drugs were without effect on Kir6.2/SUR2A and Kir6.2/SUR2B currents in inside-out patches when examined in the presence of intracellular MgADP or MgATP, both compounds inhibited Kir6.2/SUR2A and Kir6.2/SUR2B currents in the absence of added nucleotide. The extent of this block was greater than that observed for Kir6.2ΔC36 expressed in the absence of SUR1, which suggests that both drugs do in fact interact with SUR2A and SUR2B.
One possible explanation of our findings is that the drugs have both stimulatory and inhibitory actions on SUR. In the absence of nucleotides, the inhibitory effect predominates, whereas in the presence of nucleotide both inhibitory and stimulatory actions coexist. In the case of SUR2, the stimulatory effect produced by the presence 100 µmol/l MgATP (or MgADP) is just sufficient to antagonise the inhibitory action of the drug, but not enough to produce an increase in channel activity. In the case of SUR1, however, the stimulatory effect is much greater and is able to cause a marked increase in current. Whatever, the molecular mechanism, the results suggest that action of the compounds will depend on the metabolic state of the cell as well as the SUR isoform. This might explain why whole-cell Kir6.2/SUR2A and Kir6.2/SUR2B currents were inhibited by NN414 in intact oocytes in which metabolism had been inhibited by 3 mmol/l azide. However, because Kir6.2/SUR2A channels were activated by both azide and P1075 we cannot rule out the possibility that the inhibitory effect of NN414 on Kir6.2/SUR2A channels is apparent rather than real, and due (in part) to displacement of P1075.
NN414 and NNC 55-0118 are about 100-fold more potent than diazoxide on Kir6.2/SUR1 and do not open KATP channels containing SUR2 subunits. These properties could make them useful for treatment of disease states where inhibition of insulin secretion is beneficial, such as insulinoma and certain types of congenital hyperinsulinism [28]. Compounds that are able to suppress insulin secretion, like diazoxide, have been used therapeutically previously, but the side-effects on the cardiovascular system, such a marked fall in blood pressure, have proved difficult to manage. The present compounds offer the advantage that they do not activate Kir6.2/SUR2A and Kir6.2/SUR2B: because these compounds interact with the SUR subunit, they are also unlikely to activate Kir6.1/SUR2B channels. Thus, only Kir6.2/SUR1 channels will be opened. Although both drugs exert an inhibitory effect on Kir6.2/SUR2A and Kir6.2/SUR2B channels, this might not cause clinical problems because sulphonylureas such as glibenclamide (which block Kir6.2/SUR1, Kir6.2/SUR2A and Kir6.2/SUR2B) have been used for many years without marked side effects on the cardiovascular system. However, clinical trials would be required to confirm this idea.
Abbreviations
- KATP channel:
-
ATP-sensitive potassium channel
- SUR:
-
sulphonylurea receptor
- KCO:
-
K+ channel opener
- Kir:
-
inwardly rectifying K+ channel
- TEVC:
-
two electrode voltage clamp
- HEK293 cell:
-
Human Embryonic Kidney 293 cell
References
Coghlan MJ, Carroll WA, Gopalakrishnan M (2001) Recent developments in the biology and medicinal chemistry of potassium channel modulators: Update from a decade of progress. J Med Chem 44:1627–1653
Ashcroft FM, Rorsman P (1990) ATP-sensitive K+ channels: a link between β-cell metabolism and insulin secretion. Biochem Soc Trans 18:109–111
Trube G, Rorsman P, Ohno-Shosaku T (1996) Opposite effects of tolbutamide and diazoxide on the ATP-dependent K+ channel in mouse pancreatic beta cells. Pflugers Arch 407:493–499
Alemzadeh R, Slonim AE, Zdanowicz ML et al. (1993) Modification of insulin resistance by diazoxide in obese Zucker rats. Endocrinology 133:705–712
Aizawa T, Taguchi N, Sato Y et al. (1995) Prophylaxis of genetically determined diabetes by diazoxide: a study in a rat model of naturally occurring obese diabetes. J Pharmacol Exp Ther 275:194–199
Björk E, Berne C, Kampe O et al. (1996) Diazoxide treatment at onset preserves residual insulin secretion in adults with autoimmune diabetes. Diabetes 45:1427–1430
Seino S, Miki T (2003) Physiological and pathophysiological roles of ATP-sensitive K+ channels. Prog Biophys Mol Biol 81:133–176
Inagaki N, Gonoi T, Clement JP 4th et al. (1995) Reconstitution of I KATP: an inward rectifier subunit plus the sulfonylurea receptor. Science 270:1166–1170
Sakura H, Ämmälä C, Smith PA et al. (1995) Cloning and functional expression of the cDNA encoding a novel ATP-sensitive potassium channel subunit expressed in pancreatic β-cells, brain, heart and skeletal muscle. FEBS Lett 377:338–344
Inagaki N, Gonoi T, Clement JP 4th et al. (1996) A family of sulfonylurea receptors determines the pharmacological properties of ATP-sensitive K+ channels. Neuron 16:1011–1017
Miki T, Suzuki M, Shibasaki T et al. (2002) Mouse model of Prinzmetal angina by disruption of the inward rectifier Kir6.1. Nat Med 8:466–472
Isomoto S, Kondo C, Yamada M et al. (1996) A novel sulfonylurea receptor forms with BIR (Kir6.2) a smooth muscle type ATP-sensitive K+ channel. J Biol Chem 271:24321–24324
Liss B, Bruns R, Roeper J (1999) Alternative sulfonylurea receptor expression defines metabolic sensitivity of K-ATP channels in dopaminergic midbrain neurons. EMBO J 18:833–846
Ashcroft FM, Gribble FM. (1998) Correlating structure and function in ATP-sensitive K+ channels. Trends Neurosci 21:288–294
D'hahan N, Jacquet H, Moreau C et al. (1999) A transmembrane domain of the sulfonylurea receptor mediates activation of ATP-sensitive K+ channels by K+ channel openers. Mol Pharmacol 56:308–315
D'hahan N, Moreau C, Prost A-L et al. (1999) Pharmacological plasticity of cardiac ATP-sensitive potassium channels toward diazoxide revealed by ADP. Proc Natl Acad Sci USA 96:12162–12167
Babenko AP, Gonzalez G, Bryan J (2000) Pharmaco-topology of sulfonylurea receptors. Separate domains of the regulatory subunits of KATP channel isoforms are required for selective interaction with K+ channel openers. J Biol Chem 275:717–720
Matsuoka T, Matsushita K, Katayama Y et al. (2000) C-terminal tails of sulfonylurea receptors control ADP-induced activation and diazoxide modulation of ATP-sensitive K(+) channels. Circ Res 87:873–880
Lawson K. (2000) Potassium channel openers as potential therapeutic weapons in ion channel disease. Kidney Int 57:838–845
Aguilar-Bryan L, Nichols CG, Wechsler SW et al. (1995) Cloning of the β-cell high-affinity sulphonylurea receptor: a regulator of insulin secretion. Science 268:423–425
Tucker SJ, Gribble FM, Zhao C et al. (1997) Truncation of Kir6.2 produces ATP-sensitive K-channels in the absence of the sulphonylurea receptor. Nature 387
Aguilar-Bryan L, Clement JP IV, Gonzalez G et al. (1998) Toward understanding the assembly and structure of KATP channels. Physiol Rev 78:227–245
Gribble FM, Ashfield R, Ämmälä C et al. (1997) Properties of cloned ATP-sensitive K-currents expressed in Xenopus oocytes. J Physiol 498:87–98
Wahl P, Anker C, Traynelis SF et al. (1998) Antagonist properties of a phosphonoisoxazole amino acid at glutamate R1–4 (R,S)-2-amino-3(3-hydroxy-5-methyl-4-isoxazolyl)-propionic acid receptor subtypes. Mol Pharmacol 53:590–596
Nielsen FE, Bodvarsdottir TB, Worsaae A et al. (2002) 6-Chloro-3-alkylamino-4H-thieno[3,2-e]-1,2,4-thiadiazine 1,1-dioxide derivatives potently and selectively activate ATP sensitive potassium channels of pancreatic beta cells. J Med Chem 45:4171–4187
Larsson O, Ammala C, Bokvist K et al. (1993) Stimulation of the KATP channel by ADP and diazoxide requires nucleotide hydrolysis in mouse pancreatic beta cells. J Physiol (Lond) 463:349–365
Gribble FM, Tucker SJ, Ashcroft FM (1997b) The essential role of the Walker A motifs of SUR1 in K-ATP channel activation by Mg-ADP and diazoxide. EMBO J 16:1145–1152
Glaser B, Thornton P, Otonkoski T et al. (2000) Genetics of neonatal hyperinsulinism. Arch Dis Child Fetal Neonatal Ed 82:F79–F86
Acknowledgements
We thank the Wellcome Trust for support. M.D. is a Robert Turner Visiting Scholar. F.M.A. is the Royal Society GlaxoSmithKline Research Professor.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dabrowski, M., Larsen, T., Ashcroft, F.M. et al. Potent and selective activation of the pancreatic beta-cell type KATP channel by two novel diazoxide analogues. Diabetologia 46, 1375–1382 (2003). https://doi.org/10.1007/s00125-003-1198-1
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-003-1198-1