Abstract
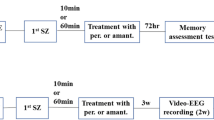
Status epilepticus (SE) is a life-threatening condition characterized by ongoing seizure activity which can lead to severe brain damage and death if not treated properly. Recent work suggests that alterations in blood-brain barrier (BBB) function and subsequent cortical exposure to coagulation factors may initiate, promote, and/or sustain SE. This suggestion is based on the observation that the serine protease thrombin, which plays a fundamental role in the blood coagulation cascade, increases neural excitability through the activation of protease-activated receptor 1 (PAR1). However, it remains unclear whether systemic inhibition of thrombin asserts “anti-epileptic” effects in vivo. We here used the pilocarpine model of SE in adult 3-month-old male mice to address the question whether intraperitoneal injection of the thrombin inhibitor α-NAPAP (0.75 mg/kg) counters SE. Indeed, pharmacological inhibition of thrombin ameliorates the behavioral outcome of pilocarpine-induced SE. Similar results are obtained when the thrombin receptor PAR1 is pharmacologically blocked using intraperitoneal injection of SCH79797 (25 μg/kg) prior to SE induction. Consistent with these results, an increase in thrombin immunofluorescence is detected in the hippocampus of pilocarpine-treated animals. Moreover, increased hippocampal serine protease activity is detected 90 min after SE induction, which is not observed in animals treated with α-NAPAP prior to SE induction. Together, these results corroborate and extend recent studies suggesting that novel oral anticoagulants which target thrombin (and PAR1) may assert anti-epileptic effects in vivo.
Key messages
-
Systemic thrombin/PAR1-inhibition ameliorates anticoagulants behavioral seizures.
-
Status epilepticus increases thrombin levels in the hippocampus.
-
Increased serine protease activity in the hippocampus after status epileptic.
-
Anti-epileptic potential of clinically used anticoagulants must be evaluated.



Similar content being viewed by others
References
Seinfeld S, Goodkin HP, Shinnar S (2016) Status epilepticus. Cold Spring Harb Perspect Med 6(3):a022830
Bell B, Lin JJ, Seidenberg M, Hermann B (2011) The neurobiology of cognitive disorders in temporal lobe epilepsy. Nat Rev Neurol 7(3):154–164
Trinka E, Brigo F, Shorvon S (2016) Recent advances in status epilepticus. Curr Opin Neurol. 29(2):189–198
Walker MC (2018) Pathophysiology of status epilepticus. Neurosci Lett. 667:84–91
Bar-Klein G, Lublinsky S, Kamintsky L, Noyman I, Veksler R, Dalipaj H et al (2017) Imaging blood-brain barrier dysfunction as a biomarker for epileptogenesis. Brain. 140(6):1692–1705
Gorter JA, van Vliet EA, Aronica E (2015) Status epilepticus, blood-brain barrier disruption, inflammation, and epileptogenesis. Epilepsy Behav. 49:13–16
Friedman A (2011) Blood-brain barrier dysfunction, status epilepticus, seizures, and epilepsy: a puzzle of a chicken and egg. Epilepsia 52(Suppl 8):19–20
Ruber T, David B, Luchters G, Nass RD, Friedman A, Surges R et al (2018) Evidence for peri-ictal blood-brain barrier dysfunction in patients with epilepsy. Brain. 141(10):2952–2965
Isaeva E, Hernan A, Isaev D, Holmes GL (2012) Thrombin facilitates seizures through activation of persistent sodium current. Ann Neurol 72(2):192–198
Maggio N, Cavaliere C, Papa M, Blatt I, Chapman J, Segal M (2013) Thrombin regulation of synaptic transmission: implications for seizure onset. Neurobiol Dis. 50:171–178
Maggio N, Shavit E, Chapman J, Segal M (2008) Thrombin induces long-term potentiation of reactivity to afferent stimulation and facilitates epileptic seizures in rat hippocampal slices: toward understanding the functional consequences of cerebrovascular insults. J Neurosci. 28(3):732–736
Lenz M, Ben Shimon M, Deller T, Vlachos A, Maggio N (2017) Pilocarpine-induced status epilepticus is associated with changes in the actin-modulating protein synaptopodin and alterations in long-term potentiation in the mouse hippocampus. Neural Plast 2017:2652560
Muller CJ, Bankstahl M, Groticke I, Loscher W (2009) Pilocarpine vs. lithium-pilocarpine for induction of status epilepticus in mice: development of spontaneous seizures, behavioral alterations and neuronal damage. Eur J Pharmacol. 619(1-3):15–24
Phelan KD, Shwe UT, Williams DK, Greenfield LJ, Zheng F (2015) Pilocarpine-induced status epilepticus in mice: a comparison of spectral analysis of electroencephalogram and behavioral grading using the Racine scale. Epilepsy Res 117:90–96
Racine RJ (1972) Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr Clin Neurophysiol 32(3):281–294
Luttjohann A, Fabene PF, van Luijtelaar G (2009) A revised Racine’s scale for PTZ-induced seizures in rats. Physiol Behav. 98(5):579–586
Kaiser B, Markwardt F (1986) Experimental studies on the antithrombotic action of a highly effective synthetic thrombin inhibitor. Thromb Haemost. 55(2):194–196
Shavit Stein E, Ben Shimon M, Artan Furman A, Golderman V, Chapman J, Maggio N (2018) Thrombin inhibition reduces the expression of brain inflammation markers upon systemic LPS treatment. Neural Plast 2018:7692182
Ahn HS, Foster C, Boykow G, Stamford A, Manna M, Graziano M (2000) Inhibition of cellular action of thrombin by N3-cyclopropyl-7-[[4-(1-methylethyl)phenyl]methyl]-7H-pyrrolo[3,2-f]quinazoline-1,3-diamine (SCH 79797), a nonpeptide thrombin receptor antagonist. Biochem Pharmacol. 60(10):1425–1434
Strehl A, Lenz M, Itsekson-Hayosh Z, Becker D, Chapman J, Deller T et al (2014) Systemic inflammation is associated with a reduction in synaptopodin expression in the mouse hippocampus. Exp Neurol. 261:230–235
Vlachos A, Ikenberg B, Lenz M, Becker D, Reifenberg K, Bas-Orth C et al (2013) Synaptopodin regulates denervation-induced homeostatic synaptic plasticity. Proc Natl Acad Sci U S A 110(20):8242–8247
Bushi D, Chapman J, Katzav A, Shavit-Stein E, Molshatzki N, Maggio N et al (2013) Quantitative detection of thrombin activity in an ischemic stroke model. J Mol Neurosci. 51(3):844–850
Stein ES, Itsekson-Hayosh Z, Aronovich A, Reisner Y, Bushi D, Pick CG et al (2015) Thrombin induces ischemic LTP (iLTP): implications for synaptic plasticity in the acute phase of ischemic stroke. Sci Rep 5:7912
Isaev D, Lushnikova I, Lunko O, Zapukhliak O, Maximyuk O, Romanov A et al (2015) Contribution of protease-activated receptor 1 in status epilepticus-induced epileptogenesis. Neurobiol Dis 78:68–76
Ben Shimon M, Lenz M, Ikenberg B, Becker D, Shavit Stein E, Chapman J et al (2015) Thrombin regulation of synaptic transmission and plasticity: implications for health and disease. Front Cell Neurosci 9:151
Dihanich M, Kaser M, Reinhard E, Cunningham D, Monard D (1991) Prothrombin mRNA is expressed by cells of the nervous system. Neuron. 6(4):575–581
Xi G, Reiser G, Keep RF (2003) The role of thrombin and thrombin receptors in ischemic, hemorrhagic and traumatic brain injury: deleterious or protective? J Neurochem. 84(1):3–9
McEwen BS, Bowles NP, Gray JD, Hill MN, Hunter RG, Karatsoreos IN et al (2015) Mechanisms of stress in the brain. Nat Neurosci. 18(10):1353–1363
Ludeman MJ, Kataoka H, Srinivasan Y, Esmon NL, Esmon CT, Coughlin SR (2005) PAR1 cleavage and signaling in response to activated protein C and thrombin. J Biol Chem. 280(13):13122–13128
Nieman MT, Schmaier AH (2007) Interaction of thrombin with PAR1 and PAR4 at the thrombin cleavage site. Biochemistry 46(29):8603–8610
Semenikhina M, Bogovyk R, Fedoriuk M, Nikolaienko O, Al Kury LT, Savotchenko A et al (2019) Inhibition of protease-activated receptor 1 ameliorates behavioral deficits and restores hippocampal synaptic plasticity in a rat model of status epilepticus. Neurosci Lett. 692:64–68
Golderman V, Shavit-Stein E, Gera O, Chapman J, Eisenkraft A, Maggio N (2019) Thrombin and the protease-activated receptor-1 in organophosphate-induced status epilepticus. J Mol Neurosci. 67(2):227–234
Luo W, Wang Y, Reiser G (2007) Protease-activated receptors in the brain: receptor expression, activation, and functions in neurodegeneration and neuroprotection. Brain Res Rev. 56(2):331–345
Suzuki M, Ogawa A, Sakurai Y, Nishino A, Venohara K, Mizoi K et al (1992) Thrombin activity in cerebrospinal fluid after subarachnoid hemorrhage. Stroke. 23(8):1181–1182
Lee KR, Kawai N, Kim S, Sagher O, Hoff JT (1997) Mechanisms of edema formation after intracerebral hemorrhage: effects of thrombin on cerebral blood flow, blood-brain barrier permeability, and cell survival in a rat model. J Neurosurg. 86(2):272–278
Lee KR, Drury I, Vitarbo E, Hoff JT (1997) Seizures induced by intracerebral injection of thrombin: a model of intracerebral hemorrhage. J Neurosurg. 87(1):73–78
Bushi D, Ben Shimon M, Shavit Stein E, Chapman J, Maggio N, Tanne D (2015) Increased thrombin activity following reperfusion after ischemic stroke alters synaptic transmission in the hippocampus. J Neurochem. 135(6):1140–1148
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD et al (2014) Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 383(9921):955–962
Verheugt FW, Granger CB (2015) Oral anticoagulants for stroke prevention in atrial fibrillation: current status, special situations, and unmet needs. Lancet. 386(9990):303–310
Ferlazzo E, Gasparini S, Beghi E, Sueri C, Russo E, Leo A et al (2016) Epilepsy in cerebrovascular diseases: review of experimental and clinical data with meta-analysis of risk factors. Epilepsia. 57(8):1205–1214
Silverman IE, Restrepo L, Mathews GC (2002) Poststroke seizures. Arch Neurol. 59(2):195–201
Levesque M, Avoli M, Bernard C (2016) Animal models of temporal lobe epilepsy following systemic chemoconvulsant administration. J Neurosci Methods 260:45–52
Salar S, Maslarova A, Lippmann K, Nichtweiss J, Weissberg I, Sheintuch L et al (2014) Blood-brain barrier dysfunction can contribute to pharmacoresistance of seizures. Epilepsia. 55(8):1255–1263
Liu JY, Thom M, Catarino CB, Martinian L, Figarella-Branger D, Bartolomei F et al (2012) Neuropathology of the blood-brain barrier and pharmaco-resistance in human epilepsy. Brain. 135(Pt 10):3115–3133
Funding
The work was supported by German Israeli Foundation (GIF G-1317-418.13/2015 to AV and NM).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Animal handling was approved by the Institutional Animal Care and Use Committee at the Chaim Sheba Medical Center, which adheres to the national law and NIH rules (registration no.: 736/12).
Competing interests
The authors declare that there are no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Maximilian Lenz and Marina Ben Shimon are joint first authors.
Rights and permissions
About this article
Cite this article
Lenz, M., Shimon, M.B., Benninger, F. et al. Systemic thrombin inhibition ameliorates seizures in a mouse model of pilocarpine-induced status epilepticus. J Mol Med 97, 1567–1574 (2019). https://doi.org/10.1007/s00109-019-01837-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-019-01837-2