Abstract
Diabetic peripheral neuropathy (DPN) is one of the most common diabetic complications. Mechanisms underlying nerve damage and sensory loss following metabolic dysfunction remain largely unclear. Recently, hyperglycemia-induced mitochondrial dysfunction and the generation of reactive oxygen species (ROS) have gained attention as possible mechanisms of organ damage in diabetes. Hypoxia-inducible factor 1 (HIF1α) is a key transcription factor activated by hypoxia, hyperglycemia, nitric oxide as well as ROS, suggesting a fundamental role in DPN susceptibility. We analyzed regulation of HIF1α in response to prolonged hyperglycemia. Genetically modified mutant mice, which conditionally lack HIF1α in peripheral sensory neurons (SNS-HIF1α−/−), were analyzed longitudinally up to 6 months in the streptozotocin (STZ) model of type1 diabetes. Behavioral measurements of sensitivity to thermal and mechanical stimuli, quantitative morphological analyses of intraepidermal nerve fiber density, measurements of ROS, ROS-induced cyclic GMP-dependent protein kinase 1α (PKG1α), and levels of vascular endothelial growth factor (VEGF) in sensory neurons in vivo were undertaken over several months post-STZ injections to delineate the role of HIF1α in DPN. Longitudinal behavioral and morphological analyses at 5, 13, and 24 weeks post-STZ treatment revealed that SNS-HIF1α−/− developed stronger hyperglycemia-evoked losses of peripheral nociceptive sensory axons associated with stronger losses of mechano- and heat sensation with a faster onset than HIF1αfl/fl mice. Mechanistically, these histomorphologic, behavioral, and biochemical differences were associated with a significantly higher level of STZ-induced production of ROS and ROS-induced PKG1α dimerization in sensory neurons of SNS-HIF1α−/− mice as compared with HIF1αfl/fl. We found that prolonged hyperglycemia induced VEGF expression in the sciatic nerve which is impaired in SNS-HIF1α mice. Our results indicate that HIF1α is as an upstream modulator of ROS in peripheral sensory neurons and exerts a protective function in suppressing hyperglycemia-induced nerve damage by limiting ROS levels and by inducing expression of VEGF which may promote peripheral nerve survival. Our data suggested that HIF1α stabilization may be thus a new strategy target for limiting sensory loss, a debilitating late complication of diabetes.
Key messages
• Impaired hypoxia-inducible factor 1α (HIF1α) signaling leads to early onset of STZ-induced loss of sensation in mice.
• STZ-induced loss of sensation in HIF1α mutant mice is associated with loss of sensory nerve fiber in skin.
• Activation of HIF1α signaling in diabetic mice protects the sensory neurons by limiting ROS formation generated due to mitochondrial dysfunction and by inducing VEGF expression.



Similar content being viewed by others
Abbreviations
- HIF1α:
-
Hypoxia-inducible factor 1α
- ROS:
-
Reactive oxygen species
- STZ:
-
Streptozotocin
- DPN:
-
Diabetic peripheral neuropathy
- DRG:
-
Dorsal root ganglia
- SNS:
-
Sensory neuron-specific
References
Mathers CD, Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3(11):e442
Duby JJ, Campbell RK, Setter SM, White JR, Rasmussen KA (2004) Diabetic neuropathy: an intensive review. Am J Health Syst Pharm 61:160–173
Colloca L, Ludman T, Bouhassira D, Baron R, Dickenson AH, Yarnitsky D, Freeman R, Truini A, Attal N, Finnerup NB, Eccleston C, Kalso E, Bennett DL, Dworkin RH, Raja SN (2017) Neuropathic pain. Nat Rev Dis Primers 3:17002
Callaghan BC, Cheng HT, Stables CL, Smith AL, Feldman EL (2012) Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol 11(6):521–534
Vincent AM, Callaghan BC, Smith AL, Feldman EL (2011) Diabetic neuropathy: cellular mechanisms as therapeutic targets. Nat Rev Neurol 7(10):573–583
Oates PJ (2002) Polyol pathway and diabetic peripheral neuropathy. Int Rev Neurobiol 50:325–392
Du XL, Edelstein D, Rossetti L, Fantus IG, Goldberg H, Ziyadeh F et al (2000) Hyperglycemia-induced mitochondrial superoxide overproduction activates the hexosamine pathway and induces plasminogen activator inhibitor-1 expression by increasing Sp1 glycosylation. Proc Natl Acad Sci U S A 97(22):12222–12226
Eichberg J (2002) Protein kinase C changes in diabetes: is the concept relevant to neuropathy? Int Rev Neurobiol 50:61–82
Misur I, Zarković K, Barada A, Batelja L, Milicević Z, Turk Z (2004) Advanced glycation endproducts in peripheral nerve in type 2 diabetes with neuropathy. Acta Diabetol 41(4):158–166
Miyauchi Y, Shikama H, Takasu T, Okamiya H, Umeda M, Hirasaki E, Ohhata I, Nakayama H, Nakagawa S (1996) Slowing of peripheral motor nerve conduction was ameliorated by aminoguanidine in streptozocin-induced diabetic rats. Eur J Endocrinol 134(4):467–473
van der Vlies D, Makkinje M, Jansens A, Braakman I, Verkleij AJ, Wirtz KW et al (2003) Oxidation of ER resident proteins upon oxidative stress: effects of altering cellular redox/antioxidant status and implications for protein maturation. Antioxid Redox Signal 5(4):381–387
Fiorentino TV, Prioletta A, Zuo P, Folli F (2013) Hyperglycemia-induced oxidative stress and its role in diabetes mellitus related cardiovascular diseases. Curr Pharm Des 19(32):5695–5703
Catrina SB, Okamoto K, Pereira T, Brismar K, Poellinger L (2004) Hyperglycemia regulates hypoxia-inducible factor-1alpha protein stability and function. Diabetes 53(12):3226–3232
Masoud GN, Li W (2015) HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharm Sin B 5(5):378–389
Wang GL, Jiang BH, Rue EA, Semenza GL (1995) Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci U S A 92(12):5510–5514
Salceda S, Caro J (1997) Hypoxia-inducible factor 1alpha (HIF-1alpha) protein is rapidly degraded by the ubiquitin-proteasome system under normoxic conditions. Its stabilization by hypoxia depends on redox-induced changes. J Biol Chem 272(36):22642–22647
Iwai K, Yamanaka K, Kamura T, Minato N, Conaway RC, Conaway JW, Klausner RD, Pause A (1999) Identification of the von Hippel-Lindau tumor-suppressor protein as part of an active E3 ubiquitin ligase complex. Proc Natl Acad Sci U S A 96(22):12436–12441
Kanngiesser M, Mair N, Lim HY, Zschiebsch K, Blees J, Häussler A, Brüne B, Ferreiròs N, Kress M, Tegeder I (2014) Hypoxia-inducible factor 1 regulates heat and cold pain sensitivity and persistence. Antioxid Redox Signal 20(16):2555–2571
Agarwal N, Offermanns S, Kuner R (2004) Conditional gene deletion in primary nociceptive neurons of trigeminal ganglia and dorsal root ganglia. Genesis 38(3):122–129
Simonetti M, Agarwal N, Stösser S, Bali KK, Karaulanov E, Kamble R, Pospisilova B, Kurejova M, Birchmeier W, Niehrs C, Heppenstall P, Kuner R (2014) Wnt-Fzd signaling sensitizes peripheral sensory neurons via distinct noncanonical pathways. Neuron 83(1):104–121
Guo BL, Sui BD, Wang XY, Wei YY, Huang J, Chen J, Wu SX, Li YQ, Wang YY, Yang YL (2013) Significant changes in mitochondrial distribution in different pain models of mice. Mitochondrion 13(4):292–297
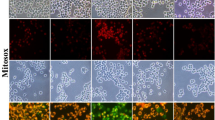
Cottet-Rousselle C, Ronot X, Leverve X, Mayol JF (2011) Cytometric assessment of mitochondria using fluorescent probes. Cytometry A 79(6):405–425
Hsieh YL, Lin CL, Chiang H, Fu YS, Lue JH, Hsieh ST (2012) Role of peptidergic nerve terminals in the skin: reversal of thermal sensation by calcitonin gene-related peptide in TRPV1-depleted neuropathy. PLoS One 7(11):e50805
Koulmanda M, Qipo A, Chebrolu S, O'Neil J, Auchincloss H, Smith RN (2003) The effect of low versus high dose of streptozotocin in cynomolgus monkeys (Macaca fascilularis). Am J Transplant 3:267–272
Yorek MA (2016) Alternatives to the streptozotocin-diabetic rodent. Int Rev Neurobiol 127:89–112
Lenzen S (2008) The mechanisms of alloxan- and streptozotocin-induced diabetes. Diabetologia 51:216–226
Korngut L, Ma CH, Martinez JA, Toth CC, Guo GF, Singh V et al (2012) Overexpression of human HSP27 protects sensory neurons from diabetes. Neurobiol Dis 47(3):436–443
Murakami T, Iwanaga T, Ogawa Y, Fujita Y, Sato E, Yoshitomi H, Sunada Y, Nakamura A (2013) Development of sensory neuropathy in streptozotocin-induced diabetic mice. Brain Behav 3:35–41
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414(6865):813–820
Catrina SB, Okamoto K, Pereira T, Brismar K, Poellinger L (2004) Hyperglycemia regulates hypoxia-inducible factor-1alpha protein stability and function. Diabetes 53(12):3226–3232
Bullock JJ, Mehta SL, Lin Y, Lolla P, Li PA (2009) Hyperglycemia-enhanced ischemic brain damage in mutant manganese SOD mice is associated with suppression of HIF-1alpha. Neurosci Lett 456(2):89–92
Hirota K, Semenza GL (2001) Rac1 activity is required for the activation of hypoxia-inducible factor 1. J Biol Chem 276(24):21166–72
Gough DR, Cotter TG (2011) Hydrogen peroxide: a Jekyll and Hyde signalling molecule. Cell Death Dis 6(2):e213
Dengler VL, Galbraith M, Espinosa JM (2014) Transcriptional regulation by hypoxia inducible factors. Crit Rev Biochem Mol Biol 49(1): 1–15 49:1–15
Xiao H, Gu Z, Wang G, Zhao T (2013) The possible mechanisms underlying the impairment of HIF-1α pathway signaling in hyperglycemia and the beneficial effects of certain therapies. Int J Med Sci 10(10):1412–1421
Yagihashi S, Mizukami H, Sugimoto K (2011) Mechanism of diabetic neuropathy: where are we now and where to go? J Diabetes Investig 2(1):18–32
Pabbidi RM, Yu SQ, Peng S, Khardori R, Pauza ME, Premkumar LS (2008) Influence of TRPV1 on diabetes-induced alterations in thermal pain sensitivity. Mol Pain 1(4):9
Andersson DA, Gentry C, Light E, Vastani N, Vallortigara J, Bierhaus A, Fleming T, Bevan S (2013) Methylglyoxal evokes pain by stimulating TRPA1. PLoS One 8(10):e77986
Bohuslavova R, Cerychova R, Nepomucka K, Pavlinkova G (2017) Renal injury is accelerated by global hypoxia-inducible factor 1 alpha deficiency in a mouse model of STZ-induced diabetes. BMC Endocr Disord 17(1):48
Botusan IR, Sunkari VG, Savu O, Catrina AI, Grünler J, Lindberg S et al (2008) Stabilization of HIF-1alpha is critical to improve wound healing in diabetic mice. Proc Natl Acad Sci U S A 105(49):19426–19431
Bonello S, Zähringer C, BelAiba RS, Djordjevic T, Hess J, Michiels C et al (2007) Reactive oxygen species activate the HIF-1alpha promoter via a functional NFkappaB site. Arterioscler Thromb Vasc Biol 27(4):755–761
Zhang Q, Fang W, Ma L, Wang ZD, Yang YM, Lu YQ (2018) VEGF levels in plasma in relation to metabolic control, inflammation, and microvascular complications in type-2 diabetes: a cohort study. Medicine (Baltimore) 97(15):e0415
Schratzberger P, Walter DH, Rittig K, Bahlmann FH, Pola R, Curry C, Silver M, Krainin JG, Weinberg DH, Ropper AH, Isner JM (2001) Reversal of experimental diabetic neuropathy by VEGF gene transfer. J Clin Invest 107(9):1083–1092
Dengler VL, Galbraith M, Espinosa JM (2014) Transcriptional regulation by hypoxia inducible factors. Crit Rev Biochem Mol Biol 49(1):1–15
Kim HK, Par SK, Zhou JL, Taglialatela G, Chung K, Coggeshall RE et al (2004) Reactive oxygen species (ROS) play an important role in a rat model of neuropathic pain. Pain 111(1–2):116–124
Yowtak J, Lee KY, Kim HY, Wang J, Kim HK, Chung K, Chung JM (2011) Reactive oxygen species contribute to neuropathic pain by reducing spinal GABA release. Pain 152(4):844–852
Murphy MP (2009) How mitochondria produce reactive oxygen species. Biochem J 417(1):1–13
Shah MS, Brownlee M (2016) Molecular and cellular mechanisms of cardiovascular disorders in diabetes. Circ Res 118(11):1808–1829
Acknowledgments
The authors thank Rose LeFaucheur for secretarial help, Dunja Baumgartl-Ahlert and Hans-Joseph Wrede for technical assistance, and Dr. Manuela Simonetti for help with i.t injections. This work was supported by a grant from the Deutsche Forschungsgemeinschaft (DFG) in the Collaborative Research Center 1118 (SFB1118 Project B06) to N.A. and R.K. We acknowledge support from the Interdisciplinary Neurobehavioral Core (INBC) for behavioral experiments.
Author information
Authors and Affiliations
Contributions
NA and RK designed the study; IT mated HIF1αfl/fl mice and SNS-Cre mice and gave general conceptual input; DRR performed and analyzed in vivo experiments; NA and DRR performed and analyzed in vitro experiments; NA and RK generated the SNS-Cre line and wrote the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
All animal experiments were done in accordance with ethical guidelines and approved by Regierungspräsidium Karlsruhe, Germany. The manuscript does not contain clinical studies or patient data.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Rojas, D.R., Tegeder, I., Kuner, R. et al. Hypoxia-inducible factor 1α protects peripheral sensory neurons from diabetic peripheral neuropathy by suppressing accumulation of reactive oxygen species.. J Mol Med 96, 1395–1405 (2018). https://doi.org/10.1007/s00109-018-1707-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-018-1707-9