Abstract
It has long been assumed that children develop natural immunity to pneumococci via the acquisition of anticapsular antibodies, which confers serotype-specific immunity to the organism. This view has been further reinforced by the recent success of capsular polysaccharide conjugate vaccines in children in reducing colonization and disease caused by vaccine-type strains. Less clear, however, is whether this mechanism is responsible for the age-related gradual increased resistance to pneumococcal carriage and disease. Recent epidemiologic and experimental evidence point to the possibility that another mechanism may be involved. Here, an alternative possibility is presented, whereby it is proposed that acquired immunity to this common human pathogen is derived not only from natural acquisition of antibodies (capsular and noncapsular) that provides protection against invasive disease but also from the development of pneumococcus-specific CD4+ TH17 cells that reduces the duration of carriage and may also impact mucosal disease. This review focuses on the experimental and clinical evidence in support of this hypothesis. The implications for future vaccine development against Streptococcus pneumoniae are also discussed.
Similar content being viewed by others
Introduction
Almost one million children in the developing world die of pneumococcal infections each year [1]. The two existing pneumococcal vaccines are based on injected mixtures of capsular polysaccharides, of which there are at least 92 different serotypes. Plain (unconjugated) polysaccharide vaccines are not efficacious in children less than 2 years old and therefore, fail to protect those at highest risk. Protein-conjugated polysaccharide vaccine protects infants [2] but is very difficult to manufacture (which has resulted in severe shortages until recently) is expensive, needs refrigeration, requires multiple injections, and does not include many of the capsular serotypes that cause pneumococcal disease in the developing world. Furthermore, serotype replacement [3] whereby pneumococcal serotypes not included in the conjugate vaccine become more prevalent causes of colonization and disease has already been observed in epidemiologic studies following implementation of conjugate vaccine immunization programs [4]. Although data are still being analyzed, there are important early signs to suggest that the impressive efficacy of the conjugate vaccine in the US may not have been reproduced in other countries that have implemented universal immunization [5]. Therefore, despite the success of the conjugate vaccine, alternative strategies are urgently needed.
In order to develop a more successful vaccine strategy, a better understanding is required of the mechanisms of immunity to pneumococcal colonization, the first and necessary step that leads to invasive disease [6]. A challenge, of course, is that it is unclear whether humans ever become completely immune to this organism: while certain risk groups can clearly be defined on the basis of age, immune deficiency, or other predisposing factors, it is an unavoidable reality that this essentially human pathogen can colonize and cause disease at all ages and in the absence of any currently known or identifiable risk factors. The focus of this review is to discuss aspects of acquired immunity to this pathogen and review data in favor of a novel mechanism of protection based on recent data derived from studies in animal models and humans.
Role of antibodies in protection against invasive pneumococcal disease
The success of capsular polysaccharide-based serotherapy and plain polysaccharide and polysaccharide conjugate vaccines has led to the inference that natural protection against invasive pneumococcal disease is largely conferred by anticapsular antibody. It is still believed by many that systemic antibodies to the capsular polysaccharide primarily determine antipneumococcal immunity. In fact, whereas it has been well demonstrated (by both passive and active immunization studies in humans) that antibodies to the capsule are clearly sufficient to protect against invasive pneumococcal disease, it is less clear whether they are necessary or they constitute the primary mechanism of natural development of resistance to pneumococcal infection. An examination of age-specific incidence of pneumococcal disease in the US prior to the introduction of the conjugate vaccine reveals that the disease incidence for all serogroups peaks between 9 and 15 months of age and falls in approximately parallel fashion for all serogroups thereafter [7]. By age 24 months, the incidence is approximately one half of that in the peak age group. The consistency of the pattern for all serogroups argues for a common mechanism rather than for independent acquisition of immunity to each serogroup. Moreover, the disease incidence declines approximately 2 years prior to the age at which unimmunized children exhibit a substantial rise in serum concentrations of natural anticapsular antibody: in most unimmunized children in the US at age 36 months, the anticapsular antibody concentrations have not yet risen to the putative protective level of 0.35 µg/ml, yet disease from serogroups 6 and 14 is almost tenfold lower at 36 months than at 12 months [8, 9]. These findings suggest that natural pneumococcal immunity may originate through factors other than capsular antibodies.
In addition to their serotype-specific polysaccharides, pneumococci express “species” antigens, i.e., found in all or most serotypes that lie beneath or are interspersed within the capsular polysaccharide. Many of these species antigens have been characterized, such as pneumococcal surface protein A (PspA), adhesin A (PsaA), the cholesterol-dependent cytolysin called pneumolysin, the teichoic acid “cell wall polysaccharide” (CWPS), and the structurally similar membrane-bound lipoteichoic acid (LTA). These pneumococcal components are immunogenic early in life, and antibodies against them can be elicited by mucosal colonization (carriage), otitis media, or invasive disease [10, 11]. In some studies, “species” antibodies have been shown to be induce protection against sepsis either by active parenteral and intranasal immunization with antigen or by passive parenteral immunization with antibody to these antigens [12]. While it is important to note that the efficacy of a vaccine strategy based on pneumococcal proteins has yet to be proven in humans to date, there are compelling data from animal studies that suggest that such an approach may be effective. Sera from humans who have been immunized with PspA confer passive immunity in murine pneumococcal sepsis models [13]. Murine [14] and human [15] antibodies to phosphocholine (a component of CWPS and LTA) can passively protect mice against pneumococci of certain serotypes. In general, species antigens appear less potent than capsular polysaccharide in vaccines when used individually but they are synergistic in combination [16].
More recently, potential vaccine candidates were identified by evaluating the antibody specificity of exposed but not infected individuals or convalescent patients [17]. This so-called ANTIGENome approach has led to the identification of several proteins, two of which, the serine/threonine protein kinase and protein required for cell wall separation of group B streptococcus [17], are currently undergoing Phase I clinical trials as an injectable vaccine consisting of these two proteins and PsaA.
Role of antibodies in protection against pneumococcal colonization
Pneumococcal colonization of the nasopharynx precedes and is a necessary precondition for the development of invasive disease [6]. Pneumococcal colonization is a common occurrence and occurs in most children several times in the first 2 years of life. Similar to what is observed with invasive disease, there is a reduction in the duration [18] and prevalence [19] of carriage in the first 2 years of life. Nasopharyngeal carriage can lead to the development of antibodies against specific capsular polysaccharide [20] and surface proteins [20, 21]. An analysis of longitudinal carriage data from Israeli children in daycare provided evidence for serotype-specific acquired immunity to pneumococcal carriage for some, albeit not all serotypes [22]. Taken together, these data make it reasonable to assume that the development of antibodies to capsular and noncapsular components of pneumococcus may contribute to the gradual resistance to colonization that is observed as children age. In addition, and perhaps most dramatically, the virtual elimination of vaccine-type colonizing strains in US children following implementation of the 7-valent conjugate vaccine strongly suggested that anticapsular antibodies are effective mediators of resistance to pneumococcal colonization [4].
It is less clear, however, whether these antibodies are necessary for protection against pneumococcal colonization or, to put it differently, whether this is the mechanism whereby children naturally become more resistant to pneumococcal carriage. As noted above, the reduction in susceptibility to carriage appears to precede the natural development of anticapsular antibodies in unimmunized children [7], suggesting that if antibodies are contributory, they are probably not targeting the capsular polysaccharide. A recent longitudinal study in Bangladeshi children under 1 year of age demonstrated a reduced rate of acquisition of colonization in a manner consistent with the induction of serotype-independent protective immunity [23]. At the same time, results of studies that evaluated the potential role of individual naturally acquired antibodies to a few conserved pneumococcal antigens have been mixed. In an experimental challenge model in humans, protection against carriage was reported to be associated with antibodies to a specific region of PspA [24]; however, in observational studies in children, no clear association between antibodies to certain conserved proteins and resistance to carriage could be demonstrated [10]. Thus, the role of antibodies, whether capsular or noncapsular, in the natural development of resistance of pneumococcal colonization, remains unclear. What other mechanisms may be playing a role?
A role of CD4+ IL-17A-producing T cells in the control of pneumococcal colonization
Clues to the possible existence of a second type of immunity to pneumococcal colonization were derived from an effort to develop an inexpensive species-specific vaccine. An initial motivation for the work in our laboratory was the wish to develop a mucosal, cross-serotype whole cell vaccine against pneumococcal colonization and disease. Our interest has been motivated by the desire to develop a vaccine whose properties would make it suitable for use in developing countries: low cost, no need for cold chain, mucosal administration (eliminating the need for sterile needles), and broad coverage. To this end, we began our studies with a genetically modified unencapsulated strain that has been inactivated and treated to express critical species components and given intranasally with a mucosal adjuvant to induce both local and systemic immunity. In animal models, intranasal immunization with this killed whole cell vaccine (WCV) with an adjuvant (cholera toxin or its nontoxic B subunit) provided excellent protection against both pneumococcal colonization and sepsis [25, 26].
In the course of these studies, our laboratory in collaboration with that of M. Lipsitch began to investigate the underlying mechanisms whereby this complex immunogen protects animals against pneumococcal infection, with a particular emphasis on protection against nasopharyngeal colonization. Early in our studies, we noted that protection against colonization could be conferred in a similar fashion with either repeated intranasal exposure to live pneumococci or with intranasal exposure to WCV with adjuvant [27]. Notably, protection did not appear to be dependent on the generation of anticapsular immunity: with WCV, this was obvious since the strain from which the vaccine is derived is unencapsulated; similarly, with live exposure to pneumococcus, equal protection was noted following exposure to homologous or heterologous capsular serotypes [28]. Furthermore, we noted that protection against colonization by either of these two exposures in animals appeared to reflect what was observed as children age [18, 26]—a reduction in the duration of carriage rather than a true resistance to initial colonization.
These observations led us to evaluate the possibility that protection against carriage conferred either by the WCV or by intranasal exposure to live organisms was occurring via an antibody-independent mechanism. Experiments in genetically modified mice by our group and another confirmed that protection by WCV [28] or live exposure to pneumococcus [29, 30] did not depend on antibody; instead, protection was critically dependent on CD4+ T cells as pneumococcus-specific effector cells that would protect when adoptively transferred to RAG-deficient mice [26, 28]. Further studies implicated CD4+ T cells of the IL-17A lineage, as IL-17A receptor-deficient or neutrophil-depleted mice were not protected by the WCV [26]. The IL-17A pathway was also subsequently shown by others to contribute to the monocyte/macrophage-derived clearance of primary pneumococcal infection in mice as well [31].
Similar mechanisms of protection have been shown to mediate protection against colonization from immunogens far less complex than the WCV. Using either the conserved zwitterionic polysaccharide CWPS [32] or a mixture of pneumococcal surface proteins [33, 34], we showed that significant CD4+ T cell-dependent reduction in colonization could be achieved with these defined antigens as well. More recent unpublished data from our laboratory support the view that, although IL-17A responses can be generated against several pneumococcal proteins, not all antigens are created equal and some are significantly more able to confer protection against colonization than others (Moffitt, Lu and Malley, unpublished data). Overall, these data led us to develop the hypothesis that, in humans, protection against pneumococcal colonization (and possibly also mucosal disease) may derive, at least in part, from the development of CD4+ IL-17A producing T cells that recognize pneumococcal antigens that are expressed in the course of colonization. Secretion of IL-17A from these cells may thus recruit professional phagocytes (neutrophils or macrophages) to the site of colonization and help reduce the duration of carriage. The identification of putative protective pneumococcal T cell antigens is the subject of active investigation via a program funded by PATH.
The results in mice are consistent with epidemiologic data and experimental findings from several studies in humans. With the advent of the HIV epidemic, it became evident that CD4+ T cells may play a role in mediating resistance to respiratory infections. Infected individuals have a dramatically increased risk of infections with opportunistic pulmonary pathogens such as Mycobacterium tuberculosis or Pneumocystis jiroveci, and this risk is inversely related to the number of circulating CD4+ T cells [35, 36]. For Streptococcus pneumoniae, HIV infection confers a 50-fold increased risk of infection, which is also inversely related to CD4+ T cell count [37]. Most recently, a study in Zambian mothers has demonstrated that HIV infection is associated with a significantly increased risk of colonization and reduced time to new colonization [38]. While one could hypothesize that, in children, this defect is due to the inability to generate a robust primary antipneumococcal antibody response in the absence of functional T cells [39], such an argument is less convincing to explain this dramatically increased susceptibility in adults. While various hypotheses have been advanced to explain why CD4+ T cell deficiency is associated with such a high risk of infection in adults, such as reduced opsonic activity of anticapsular antibodies [40], loss of memory B cells [41], and alteration of innate pulmonary immunity [42], it is fair to state that this susceptibility remains largely unexplained. The data presented here suggest that a loss of TH17 cells may also contribute to this increased susceptibility.
Studies of adenoidal tissue in pneumococcus-colonized vs. -noncolonized children point to a potential contribution of pneumolysin-specific CD4+ T cells in the prevention of colonization [43]. We also found that much of the WCV-induced IL-17A responses in adenoidal tissues of children could be attributed to pneumolysin since responses were significantly reduced when cells were stimulated with a pneumolysin-negative whole cell antigen [26]. Analysis of immune responses in adults with chronic obstructive disease (COPD) also suggest that antibodies may not be primarily responsible for resistance to colonization [44]. When analyzed over a 2-year period, COPD patients colonized with pneumococcus did not, on average, have lower concentration of antibodies to capsular or noncapsular components or lower serum opsonophagocytic ability than noncolonized COPD patients. In fact, the risk of acquisition of new pneumococcal strains in adults with COPD was associated with higher preacquisition concentrations of anticapsular and noncapsular pneumococcal antibodies. These results suggest that in this population, antipneumococcal antibodies are markers of prior exposure and perhaps greater susceptibility rather than predictors of protection. In contrast, preliminary data from this patient population suggest that IL-17 and IL-22 responses may be reduced in COPD patients that are frequently colonized with pneumococcus (Gross, Lu, Sethi, Murphy and Malley, unpublished). Finally, the recent discovery that patients with autosomal dominant hyper-IgE syndrome (HIES, Job’s syndrome), a disease characterized with recurrent pulmonary infections due to Staphylococcus aureus and S. pneumoniae, have mutations in the gene encoding STAT3 and an inability to produce TH17 cells, provides further support for the hypothesis that this particular arm of the acquired immune response may be playing an important role in prevention of respiratory infections, and with pneumococcus in particular [45].
Implications for future vaccine development
The spectacular success of the universal pneumococcal immunization program in the US and the results from clinical trials in South Africa and The Gambia [46, 47] understandably led to the inference that, given enough serotype coverage with future generation conjugate vaccines, pneumococcal disease could be significantly controlled, if not eradicated, in both developed and developing countries. The emergence of serotypes not included in the first generation 7-valent conjugate vaccine [48] and the demonstration that these strains are important causes of disease, morbidity, and mortality [49, 50] has somewhat tempered this enthusiasm. While current efforts to promote the use of appropriately broad pneumococcal conjugate vaccines in developed and developing countries are continuing, the need for alternative approaches to vaccination against pneumococcus remains urgent. In particular, the development and implementation of clinical trials of species-specific pneumococcal vaccines should be a priority. In this regard, it is somewhat sobering that while the proposal to use protein-based pneumococcal vaccines is not new (reviewed in [51]), no such vaccine has made it beyond Phase I clinical trials to date. Furthermore, it is clear that such an approach faces several important hurdles for development and licensure, including, but not limited to, the choice of study population, endpoints and ascertainment of efficacy, comparisons to currently approved pneumococcal vaccines, route of administration, and potential need for adjuvants for optimal stimulation of mucosal immunity.
The hypothesis presented here offers both further challenges and promises for the development of a broad pneumococcal vaccine. We propose that naturally acquired immunity to pneumococcus be viewed as (at least) a two-pronged mechanism: antibody (capsular and noncapsular)-mediated protection against invasive disease as well as colonization and CD4+ IL-17A-mediated protection against colonization and possibly also mucosal disease (see Table 1). Optimal strategies for prevention of pneumococcal disease and generation of herd immunity by vaccination may require the stimulation of both arms of the immune response. While there are numerous vaccines that generate potent antibody responses to bacterial or other antigens, relatively little is known regarding the requirements for the development of IL-17A responses in humans. The use of adjuvants, alternative nonparenteral routes of immunization, and the chemical modification of antigens for parenteral administration are all options that are being considered for the development of vaccines that elicit cell-mediated and/or mucosal immunity [34, 52–54].
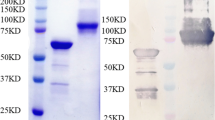
Among the many approaches that are being considered, the WCV represents an attempt to harness both forms of acquired immune responses. When injected parenterally in alum into mice or rabbits, the WCV induces high levels of antibodies directed against noncapsular pneumococcal antigens and protects mice against fatal pneumococcal pneumonia or sepsis following intraperitoneal injection (unpublished). In addition, CD4+ TH17 responses are also elicited in mice and these confer significant protection against pneumococcal colonization. Good Manufacturing Practice lots have been made by Instituto Butantan (Sao Paolo, Brazil) and shown to be effective in mouse models. Preparations are underway to seek approval for Phase I clinical trials in adults. It remains to be seen, of course, whether the efficacy of this vaccine in mouse models will translate to the prevention of pneumococcal disease in humans, but it is hoped that the clinical evaluation of this candidate will answer many of the remaining questions in pneumococcal pathogenesis and prevention.
References
WHO (1998) WHO meeting on maternal and neonatal pneumococcal immunization. Wkly Epidemiol Rec 73:187–188
Black SB, Shinefield HR, Hansen J, Elvin L, Laufer D, Malinoski F (2001) Postlicensure evaluation of the effectiveness of seven valent pneumococcal conjugate vaccine. Pediatr Infect Dis J 20:1105–1107
Lipsitch M (2001) Interpreting results from trials of pneumococcal conjugate vaccines: a statistical test for detecting vaccine-induced increases in carriage of nonvaccine serotypes. Am J Epidemiol 154:85–92
Huang SS, Hinrichsen VL, Stevenson AE, Rifas-Shiman SL, Kleinman K, Pelton SI, Lipsitch M, Hanage WP, Lee GM, Finkelstein JA (2009) Continued impact of pneumococcal conjugate vaccine on carriage in young children. Pediatrics 124:e1–e11
HPA (2009) Current epidemiology of Invasive pneumococcal disease. accessed at http://wwwhpaorguk/HPA/Topics/InfectiousDiseases/InfectionsAZ/1220341771909/
Austrian R (1986) Some aspects of the pneumococcal carrier state. J Antimicrob Chemother 18(Suppl A):35–45
Lipsitch M, Whitney CG, Zell E, Kaijalainen T, Dagan R, Malley R (2005) Age-specific incidence of invasive pneumococcal disease by serotype: are anticapsular antibodies the primary mechanism of protection against invasive disease? PLOS Medicine 2:e15
Black S, Shinefield H, Fireman B, Lewis E, Ray P, Hansen JR, Elvin L, Ensor KM, Hackell J, Siber G, Malinoski F, Madore D, Chang I, Kohberger R, Watson W, Austrian R, Edwards K (2000) Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Northern California Kaiser Permanente Vaccine Study Center Group. Pediatr Infect Dis J 19:187–195
Jodar L, Butler J, Carlone G, Dagan R, Goldblatt D, Kayhty H, Klugman K, Plikaytis B, Siber G, Kohberger R, Chang I, Cherian T (2003) Serological criteria for evaluation and licensure of new pneumococcal conjugate vaccine formulations for use in infants. Vaccine 21:3265–3272
Rapola S, Jantti V, Haikala R, Syrjanen R, Carlone GM, Sampson JS, Briles DE, Paton JC, Takala AK, Kilpi TM, Kayhty H (2000) Natural development of antibodies to pneumococcal surface protein A, pneumococcal surface adhesin A, and pneumolysin in relation to pneumococcal carriage and acute otitis media. J Infect Dis 182:1146–1152
Simell B, Korkeila M, Pursiainen H, Kilpi TM, Kayhty H (2001) Pneumococcal carriage and otitis media induce salivary antibodies to pneumococcal surface adhesin a, pneumolysin, and pneumococcal surface protein a in children. J Infect Dis 183:887–896
Briles DE, Tart RC, Swiatlo E, Dillard JP, Smith P, Benton KA, Ralph BA, Brooks-Walter A, Crain MJ, Hollingshead SK, McDaniel LS (1998) Pneumococcal diversity: considerations for new vaccine strategies with emphasis on pneumococcal surface protein A (PspA). Clin Microbiol Rev 11:645–657
Briles DE, Hollingshead SK, King J, Swift A, Braun PA, Park MK, Ferguson LM, Nahm MH, Nabors GS (2000) Immunization of humans with recombinant pneumococcal surface protein A (rPspA) elicits antibodies that passively protect mice from fatal infection with Streptococcus pneumoniae bearing heterologous PspA. J Infect Dis 182:1694–1701. doi:JID000388 [pii] 10.1086/317602
Briles DE, Forman C, Crain M (1992) Mouse antibody to phosphocholine can protect mice from infection with mouse-virulent human isolates of Streptococcus pneumoniae. Infect Immun 60:1957–1962
Goldenberg HB, McCool TL, Weiser JN (2004) Cross-reactivity of human immunoglobulin G2 recognizing phosphorylcholine and evidence for protection against major bacterial pathogens of the human respiratory tract. J Infect Dis 190:1254–1263
Ogunniyi AD, Folland RL, Briles DE, Hollingshead SK, Paton JC (2000) Immunization of mice with combinations of pneumococcal virulence proteins elicits enhanced protection against challenge with Streptococcus pneumoniae. Infect Immun 68:3028–3033
Giefing C, Meinke AL, Hanner M, Henics T, Bui MD, Gelbmann D, Lundberg U, Senn BM, Schunn M, Habel A, Henriques-Normark B, Ortqvist A, Kalin M, von Gabain A, Nagy E (2008) Discovery of a novel class of highly conserved vaccine antigens using genomic scale antigenic fingerprinting of pneumococcus with human antibodies. J Exp Med 205:117–131
Hogberg L, Geli P, Ringberg H, Melander E, Lipsitch M, Ekdahl K (2007) Age- and serogroup-related differences in observed durations of nasopharyngeal carriage of penicillin-resistant pneumococci. J Clin Microbiol 45:948–952
Bogaert D, Sluijter M, Toom NL, Mitchell TJ, Goessens WH, Clarke SC, de Groot R, Hermans PW (2006) Dynamics of pneumococcal colonization in healthy Dutch children. Microbiology 152:377–385
Goldblatt D, Hussain M, Andrews N, Ashton L, Virta C, Melegaro A, Pebody R, George R, Soininen A, Edmunds J, Gay N, Kayhty H, Miller E (2005) Antibody responses to nasopharyngeal carriage of Streptococcus pneumoniae in adults: a longitudinal household study. J Infect Dis 192:387–393
McCool TL, Cate TR, Tuomanen EI, Adrian P, Mitchell TJ, Weiser JN (2003) Serum immunoglobulin G response to candidate vaccine antigens during experimental human pneumococcal colonization. Infect Immun 71:5724–5732
Weinberger DM, Dagan R, Givon-Lavi N, Regev-Yochay G, Malley R, Lipsitch M (2008) Epidemiologic evidence for serotype-specific acquired immunity to pneumococcal carriage. J Infect Dis 197:1511–1518
Granat SM, Ollgren J, Herva E, Mia Z, Auranen K, Makela PH (2009) Epidemiological evidence for serotype-independent acquired immunity to pneumococcal carriage. J Infect Dis 200:99–106
McCool TL, Cate TR, Moy G, Weiser JN (2002) The immune response to pneumococcal proteins during experimental human carriage. J Exp Med 195:359–365
Malley R, Morse SC, Leite LCC, Mattos Areas AP, Ho PL, Kubrusly FS, Almeida IC, Anderson P (2004) Multi-serotype protection of mice against pneumococcal colonization of the nasopharynx and middle ear by killed nonencapsulated cells given intranasally with a non-toxic adjuvant. Infect Immun 72:4290–4292
Lu YJ, Gross J, Bogaert D, Finn A, Bagrade L, Zhang Q, Kolls JK, Srivastava A, Lundgren A, Forte S, Thompson CM, Harney KF, Anderson PW, Lipsitch M, Malley R (2008) Interleukin-17A mediates acquired immunity to pneumococcal colonization. PLoS Pathog 4:e1000159
Malley R, Lipsitch M, Stack A, Saladino R, Fleisher G, Pelton S, Thompson C, Briles D, Anderson P (2001) Intranasal immunization with killed unencapsulated whole cells prevents colonization and invasive disease by capsulated pneumococci. Infect Immun 69:4870–4873
Malley R, Trzcinski K, Srivastava A, Thompson CM, Anderson PW, Lipsitch M (2005) CD4+ T cells mediate antibody-independent acquired immunity to pneumococcal colonization. Proc Natl Acad Sci USA 102:4848–4853
Trzcinski K, Thompson C, Malley R, Lipsitch M (2005) Antibodies to conserved pneumococcal antigens correlate with, but are not required for, protection against pneumococcal colonization induced by prior exposure in a mouse model. Infect Immun 73:7043–7046
McCool TL, Weiser JN (2004) Limited role of antibody in clearance of streptococcus pneumoniae in a murine model of colonization. Infect Immun 72:5807–5813
Zhang Z, Clarke TB, Weiser JN (2009) Cellular effectors mediating Th17-dependent clearance of pneumococcal colonization in mice. Journal of Clinical Investigation 119:1899–1909
Malley R, Srivastava A, Lipsitch M, Thompson CM, Watkins C, Tzianabos A, Anderson PW (2006) Antibody-independent, interleukin-17A-mediated, cross-serotype immunity to pneumococci in mice immunized intranasally with the cell wall polysaccharide. Infect Immun 74:2187–2195
Basset A, Thompson CM, Hollingshead SK, Briles DE, Ades EW, Lipsitch M, Malley R (2007) Antibody-independent, CD4+ T-cell-dependent protection against pneumococcal colonization elicited by intranasal immunization with purified pneumococcal proteins. Infect Immun 75:5460–5464
Lu YJ, Forte S, Thompson CM, Anderson PW, Malley R (2009) Protection against Pneumococcal colonization and fatal pneumonia by a trivalent conjugate of a fusion protein with the cell wall polysaccharide. Infect Immun 77:2076–2083
Hoover DR, Saah AJ, Bacellar H, Phair J, Detels R, Anderson R, Kaslow RA (1993) Clinical manifestations of AIDS in the era of pneumocystis prophylaxis. Multicenter AIDS Cohort Study. N Engl J Med 329:1922–1926
Phair J, Munoz A, Detels R, Kaslow R, Rinaldo C, Saah A (1990) The risk of Pneumocystis carinii pneumonia among men infected with human immunodeficiency virus type 1. Multicenter AIDS Cohort Study Group. N Engl J Med 322:161–165
Dworkin MS, Ward JW, Hanson DL, Jones JL, Kaplan JE (2001) Pneumococcal disease among human immunodeficiency virus-infected persons: incidence, risk factors, and impact of vaccination. Clin Infect Dis 32:794–800
Gill CJ, Mwanakasale V, Fox MP, Chilengi R, Tembo M, Nsofwa M, Chalwe V, Mwananyanda L, Mukwamataba D, Malilwe B, Champo D, Macleod WB, Thea DM, Hamer DH (2008) Impact of human immunodeficiency virus infection on Streptococcus pneumoniae colonization and seroepidemiology among Zambian women. J Infect Dis 197:1000–1005
Wu ZQ, Vos Q, Shen Y, Lees A, Wilson SR, Briles DE, Gause WC, Mond JJ, Snapper CM (1999) In vivo polysaccharide-specific IgG isotype responses to intact Streptococcus pneumoniae are T cell dependent and require CD40- and B7-ligand interactions. J Immunol 163:659–667. doi:ji_v163n2p659 [pii]
Takahashi H, Oishi K, Yoshimine H, Kumatori A, Moji K, Watanabe K, Nalwoga H, Tugume SB, Kebba A, Mugerwa R, Mugyenyi P, Nagatake T (2003) Decreased serum opsonic activity against Streptococcus pneumoniae in human immunodeficiency virus-infected Ugandan adults. Clin Infect Dis 37:1534–1540
Titanji K, De Milito A, Cagigi A, Thorstensson R, Grutzmeier S, Atlas A, Hejdeman B, Kroon FP, Lopalco L, Nilsson A, Chiodi F (2006) Loss of memory B cells impairs maintenance of long-term serologic memory during HIV-1 infection. Blood 108:1580–1587
Gordon SB, Janoff EN, Sloper D, Zhang Q, Read RC, Zijlstra EE, Finn A, Molyneux ME (2005) HIV-1 infection is associated with altered innate pulmonary immunity. J Infect Dis 192:1412–1416
Zhang Q, Bagrade L, Bernatoniene J, Clarke E, Paton JC, Mitchell TJ, Nunez DA, Finn A (2007) Low CD4 T cell immunity to pneumolysin is associated with nasopharyngeal carriage of pneumococci in children. J Infect Dis 195:1194–1202
Malley R, Lipsitch M, Bogaert D, Thompson CM, Hermans P, Watkins AC, Sethi S, Murphy TF (2007) Serum antipneumococcal antibodies and pneumococcal colonization in adults with chronic obstructive pulmonary disease. J Infect Dis 196:928–935
Milner JD, Brenchley JM, Laurence A, Freeman AF, Hill BJ, Elias KM, Kanno Y, Spalding C, Elloumi HZ, Paulson ML, Davis J, Hsu A, Asher AI, O'Shea J, Holland SM, Paul WE, Douek DC (2008) Impaired T(H)17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature 452:773–776
Klugman KP, Madhi SA, Huebner RE, Kohberger R, Mbelle N, Pierce N (2003) A trial of a 9-valent pneumococcal conjugate vaccine in children with and those without HIV infection. N Engl J Med 349:1341–1348
Cutts FT, Zaman SM, Enwere G, Jaffar S, Levine OS, Okoko JB, Oluwalana C, Vaughan A, Obaro SK, Leach A, McAdam KP, Biney E, Saaka M, Onwuchekwa U, Yallop F, Pierce NF, Greenwood BM, Adegbola RA (2005) Efficacy of nine-valent pneumococcal conjugate vaccine against pneumonia and invasive pneumococcal disease in The Gambia: randomised, double-blind, placebo-controlled trial. Lancet 365:1139–1146
Hanage WP (2008) Serotype-specific problems associated with pneumococcal conjugate vaccination. Future Microbiol 3:23–30
Singleton RJ, Hennessy TW, Bulkow LR, Hammitt LL, Zulz T, Hurlburt DA, Butler JC, Rudolph K, Parkinson A (2007) Invasive pneumococcal disease caused by nonvaccine serotypes among alaska native children with high levels of 7-valent pneumococcal conjugate vaccine coverage. JAMA 297:1784–1792
Hsu HE, Shutt KA, Moore MR, Beall BW, Bennett NM, Craig AS, Farley MM, Jorgensen JH, Lexau CA, Petit S, Reingold A, Schaffner W, Thomas A, Whitney CG, Harrison LH (2009) Effect of pneumococcal conjugate vaccine on pneumococcal meningitis. N Engl J Med 360:244–256
Briles DE, Hollingshead S, Brooks-Walter A, Nabors GS, Ferguson L, Schilling M, Gravenstein S, Braun P, King J, Swift A (2000) The potential to use PspA and other pneumococcal proteins to elicit protection against pneumococcal infection. Vaccine 18:1707–1711
Cuburu N, Kweon MN, Song JH, Hervouet C, Luci C, Sun JB, Hofman P, Holmgren J, Anjuere F, Czerkinsky C (2007) Sublingual immunization induces broad-based systemic and mucosal immune responses in mice. Vaccine 25:8598–8610
Glenn GM, Kenney RT (2006) Mass vaccination: solutions in the skin. Curr Top Microbiol Immunol 304:247–268
Holmgren J, Czerkinsky C (2005) Mucosal immunity and vaccines. Nat Med 11:S45–S53
Austrian R (1984) Pneumococcal infections. In: Germanier R (ed) Bacterial vaccines. Academic, Orlando FL, pp 257–288
Austrian R (1977) Prevention of pneumococcal infection by immunization with capsular polysaccharides of Streptococcus pneumoniae: current status of polyvalent vaccines. J Infect Dis 136(Suppl):S38–S42
Eskola J, Kilpi T, Palmu A, Jokinen J, Haapakoski J, Herva E, Takala A, Kayhty H, Karma P, Kohberger R, Siber G, Makela PH (2001) Efficacy of a pneumococcal conjugate vaccine against acute otitis media. N Engl J Med 344:403–409
CDC (2005) Direct and indirect effects of routine vaccination of children with 7-valent pneumococcal conjugate vaccine on incidence of invasive pneumococcal disease—United States, 1998–2003. MMWR Morb Mortal Wkly Rep 54:893–897
Musher DM, Phan HM, Baughn RE (2001) Protection against bacteremic pneumococcal infection by antibody to pneumolysin. J Infect Dis 183:827–830
Briles DE, Hollingshead SK, Paton JC, Ades EW, Novak L, van Ginkel FW, Benjamin WH Jr (2003) Immunizations with pneumococcal surface protein A and pneumolysin are protective against pneumonia in a murine model of pulmonary infection with Streptococcus pneumoniae. J Infect Dis 188:339–348
Balachandran P, Brooks-Walter A, Virolainen-Julkunen A, Hollingshead SK, Briles DE (2002) Role of pneumococcal surface protein C in nasopharyngeal carriage and pneumonia and its ability to elicit protection against carriage of Streptococcus pneumoniae. Infect Immun 70:2526–2534
Briles DE, Ades E, Paton JC, Sampson JS, Carlone GM, Huebner RC, Virolainen A, Swiatlo E, Hollingshead SK (2000) Intranasal immunization of mice with a mixture of the pneumococcal proteins PsaA and PspA is highly protective against nasopharyngeal carriage of Streptococcus pneumoniae. Infect Immun 68:796–800
Acknowledgments
The author is deeply indebted to Porter Anderson whose active involvement, inspiration, and continued mentorship have made the work presented here possible. The author also thanks Marc Lipsitch, Claudette Thompson, the current and former members of both the Malley and Lipsitch laboratories, and Luciana Leite and her group at Instituto Butantan for their contributions to these studies. This work was supported by PATH, the Meningitis Research Foundation, the Pamela and Jack Egan Fund and the U.S. Public Health Service (grants AI067737 and AI066013).
Conflict of interest statement
The author is a member of the scientific advisory board of Genocea Biosciences, Cambridge, MA, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malley, R. Antibody and cell-mediated immunity to Streptococcus pneumoniae: implications for vaccine development. J Mol Med 88, 135–142 (2010). https://doi.org/10.1007/s00109-009-0579-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-009-0579-4