Abstract
Background
The laryngeal tube (LT) is a recommended alternative to endotracheal intubation during advanced life support (ALS). Its insertion is relatively simple; therefore, it may also serve as an alternative to bag mask ventilation (BMV) for untrained personnel performing basic life support (BLS). Data support the influence of LT on the no-flow time (NFT) compared with BMV during ALS in manikin studies.
Methods
We performed a manikin study to investigate the effect of using the LT for ventilation instead of BMV on the NFT during BLS in a prospective, randomized, single-rescuer study. All 209 participants were trained in BMV, but were inexperienced in using LT; each participant performed BLS during a 4-min time period.
Results
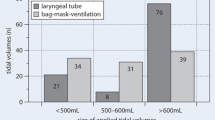
No significant difference in total NFT (LT: mean 81.1 ± 22.7 s; BMV: mean 83.2 ± 13.1 s, p = 0.414) was found; however, significant differences in the later periods of the scenario were identified. While ventilating with the LT, the proportion of chest compressions increased significantly from 67.2 to 73.2%, whereas the proportion of chest compressions increased only marginally when performing BMV. The quality of the chest compressions and the associated ventilation rate did not differ significantly. The mean tidal volume and mean minute volume were significantly lower when performing BMV.
Conclusions
The NFT was significantly shorter in the later periods in a single-rescuer, cardiac arrest scenario when using an LT without previous training compared with BMV with previous training. A possible explanation for this result may be the complexity and workload of alternating tasks (e.g., time loss when reclining the head and positioning the mask for each ventilation during BMV).
Zusammenfassung
Hintergrund
Der Larynxtubus (LT) ist eine empfohlene Alternative zur endotrachealen Intubation im Rahmen von erweiterten Reanimationsmaßnahmen (Advanced Life Support, ALS). Seine Insertion wird als einfach beschrieben, daher ist er auch eine vorstellbare Alternative zur Beutel-Masken-Beatmung (Beutel-Masken-Ventilation, BMV) für ungeübtes Personal im Rahmen von Basis-Reanimationsmaßnahmen (Basic Life Support, BLS). Studienergebnisse unterstützen einen positiven Einfluss des LT auf die No-Flow-Time (NFT) beim ALS in Manikin-Studien.
Material und Methoden
Wir führten eine prospektive, randomisierte Manikin-Studie durch, um den Einfluss des LT auf die NFT und die Qualität der Beatmung beim BLS im Vergleich zur BMV im Ein-Helfer-Modell zu untersuchen. Alle 209 Probanden waren in BMV ausgebildet, jedoch unerfahren in der Anwendung eines LT.
Ergebnisse
Es zeigte sich kein signifikanter Unterschied in der absoluten NFT (LT: durchschnittlich 81,1 ± 22,7 s; BMV: durchschnittlich 83,2 ± 13,1 s, p = 0,414); jedoch zeigten sich bei Betrachtung der späteren Zeitabschnitte des Reanimationsverlaufs signifikante Unterschiede. Bei Einsatz des LT stieg der zeitliche Anteil an Herzdruckmassage von 67,2 auf 73,2 % signifikant an, während sich bei Einsatz der BMV nur geringe Unterschiede zeigten. Die Qualität der Herzdruckmassage und die Beatmungsfrequenz unterschieden sich nicht signifikant. Die durchschnittlichen Tidal- sowie Atemminutenvolumina waren kleiner bei BMV.
Schlussfolgerungen
Die Anwendung des LT durch ungeübtes Personal im Rahmen des BLS im Ein-Helfer-Modell führt im Vergleich zur BMV durch geübtes Personal im Verlauf der Reanimation zu einer signifikanten Verkürzung der NFT. Eine mögliche Erklärung für dieses Ergebnis ist die Schwierigkeit der Maskenbeatmung und der damit verbundene, höhere Zeitaufwand (z. B. Zeitverlust durch Reklination des Kopfes und der Neupositionierung der Maske in jeder Beatmungspause) bei der BMV, die zu längeren Unterbrechungen ohne Herzdruckmassage führten.


Similar content being viewed by others
Literatur
Perkins GD, Handley AJ, Koster RW, Castrén M, Smyth MA, Olasveengen T, Monsieurs KG, Raffay V, Gräsner JT, Wenzel V, Ristagno G, Soar J (2015) European resuscitation council guidelines for resuscitation 2015 section 2. adult basic life support and use of automated external defibrillation. Resuscitation 95:81–99
Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P, Pellis T, Sandroni C, Skrifvars MB, Smith GB, Sunde K, Deakin CD (2015) European resuscitation council guidelines for resuscitation 2015 section 3. adult advanced life support. Resuscitation 95:100–149
Nordberg P, Hollenberg J, Herlitz J, Rosenqvist M, Svensson L (2009) Aspects on the increase in bystander CPR in Sweden and its association with outcome. Resuscitation 80:329–333
Wik L, Kramer-Johansen J, Myklebust H, Sorebo H, Svensson L, Fellows B, Steen PA (2005) Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA 293:299–304
Hallstrom A, Cobb L, Johnson E, Copass M (2000) Cardiopulmonary resuscitation by chest compression alone or with mouth-to-mouth ventilation. N Engl J Med 342:1546–1553
Hüpfl M, Selig HF, Nagele P (2010) Chest-compression-only versus standard cardiopulmonary resuscitation: a meta-analysis. Lancet 376:1552–1557
Deakin CD, O’Neill JF, Tabor T (2007) Does compression-only cardiopulmonary resuscitation generate adequate passive ventilation during cardiac arrest? Resuscitation 75:53–59
Iwami T, Kawamura T, Hiraide A, Berg RA, Hayashi Y, Nishiuchi T, Kajino K, Yonemoto N, Yukioka H, Sugimoto H, Kakuchi H, Sase K, Yokoyama H, Nonogi H (2007) Effectiveness of bystander-initiated cardiac-only resuscitation for patients with out-of-hospital cardiac arrest. Circulation 116:2900–2907
Lee HM, Cho KH, Choi YH, Yoon SY, Choi YH (2008) Can you deliver accurate tidal volume by manual resuscitator? Emerg Med J 25:632–634
Lockey D, Lossius HM (2014) Pre-hospital airway management: the data grows rapidly but controversy remains. Resuscitation 85:849–850
Asai T, Hidaka I, Kawachi S (2002) Efficacy of the laryngeal tube by inexperienced personnel. Resuscitation 55:171–175
Huter L, Schwarzkopf K, Rodiger J, Preussler NP, Schreiber T (2009) Students insert the laryngeal tube quicker and more often successful than the esophageal-tracheal combitube in a manikin. Resuscitation 80:930–934
Jokela J, Nurmi J, Genzwuerker HV, Castren M (2009) Laryngeal tube and intubating laryngeal mask insertion in a manikin by first-responder trainees after a short video-clip demonstration. Prehosp Disaster Med 24:63–66
Kurola J, Paakkonen H, Kettunen T, Laakso JP, Gorski J, Silfvast T (2011) Feasibility of written instructions in airway management training of laryngeal tube. Scand J Trauma Resusc Emerg Med 19:56
Lankimaki S, Alahuhta S, Kurola J (2013) Feasibility of a laryngeal tube for airway management during cardiac arrest by first responders. Resuscitation 84:446–449
Bernhard M, Beres W, Timmermann A, Stepan R, Greim CA, Kaisers UX, Gries A (2014) Prehospital airway management using the laryngeal tube. An emergency department point of view. Anaesthesist 63:589–596
Byhahn C, Schalk R, Russo SG (2014) Out-of-hospital airway management. Five scenes of a tragedy. Anaesthesist 63:543–545
Kette F, Reffo I, Giordani G, Buzzi F, Borean V, Cimarosti R, Codiglia A, Hattinger C, Mongiat A, Tararan S (2005) The use of laryngeal tube by nurses in out-of-hospital emergencies: preliminary experience. Resuscitation 66:21–25
Klaver NS, Kuizenga K, Ballast A, Fidler V (2007) A comparison of the clinical use of the laryngeal tube S and the proseal laryngeal mask airway by first-month anaesthesia residents in anaesthetised patients. Anaesthesia 62:723–727
Sunde GA, Brattebo G, Odegarden T, Kjernlie DF, Rodne E, Heltne JK (2012) Laryngeal tube use in out-of-hospital cardiac arrest by paramedics in Norway. Scand J Trauma Resusc Emerg Med 20:84
Wiese CH, Bahr J, Bergmann A, Bergmann I, Bartels U, Graf BM (2008) Reduction in no flow time using a laryngeal tube: comparison to bag-mask ventilation. Anaesthesist 57:589–596
Wiese CH, Bartels U, Bergmann A, Bergmann I, Bahr J, Graf BM (2008) Using a laryngeal tube during cardiac arrest reduces “no flow time” in a manikin study: a comparison between laryngeal tube and endotracheal tube. Wien Klin Wochenschr 120:217–223
Wiese CH, Bartels U, Schultens A, Steffen T, Torney A, Bahr J, Graf BM (2011) Using a laryngeal tube suction-device (LTS-D) reduces the “no flow time” in a single rescuer manikin study. J Emerg Med 41:128–134
Jensen JL, Walker M, LeRoux Y, Carter A (2013) Chest compression fraction in simulated cardiac arrest management by primary care paramedics: King laryngeal tube airway versus basic airway management. Prehosp Emerg Care 17:285–290
Adelborg K, Dalgas C, Grove EL, Jorgensen C, Al-Mashhadi RH, Lofgren B (2011) Mouth-to-mouth ventilation is superior to mouth-to-pocket mask and bag-valve-mask ventilation during lifeguard CPR: a randomized study. Resuscitation 82:618–622
Buck-Barrett I, Squire I (2004) The use of basic life support skills by hospital staff; what skills should be taught? Resuscitation 60:39–44
Elling R, Politis J (1983) An evaluation of emergency medical technicians’ ability to use manual ventilation devices. Ann Emerg Med 12:765–768
Schröder J, Bucher M, Meyer J (2015) Effect of the laryngeal tube on the no-flow-time in a simulated two rescuer basic life support setting with inexperienced users. Med Klin Intensiv Notfmed. doi:10.1007/s00063-015-0088-x
Rittenberger JC, Guimond G, Platt TE, Hostler D (2006) Quality of BLS decreases with increasing resuscitation complexity. Resuscitation 68:365–369
Acknowledgement
The manuscript was edited by an English language editing service to improve the linguistic quality.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
O. Meyer, M. Bucher, and J. Schröder state that there are no conflicts of interest.
The accompanying manuscript does not include studies on humans or animals.
Additional information
Authors’ contributions. OM designed the study, MB and JS helped to design and perform the study, and collected the data. OM and JS performed the statistical analysis. All authors participated in the writing process. All authors read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Meyer, O., Bucher, M. & Schröder, J. Effect of using a laryngeal tube on the no-flow time in a simulated, single-rescuer, basic life support setting with inexperienced users. Anaesthesist 65, 183–189 (2016). https://doi.org/10.1007/s00101-016-0140-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-016-0140-0