Abstract
Background
Two-tier trauma team activation (TTA)—protocols often fail to safely identify severely injured patients. A possible amendment to existing triage scores could be the measurement of serum lactate. The aim of this study was to determine the ability of the combination of serum lactate and age to predict severe injuries (ISS > 15).
Methods
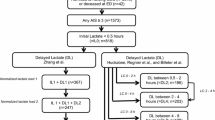
We conducted a retrospective cohort study in a single level one trauma center in a 20 months study-period and analyzed every trauma team activation (TTA) due to the mechanism of injury (MOI). Primary endpoint was the correlation between serum lactate (and age) and ISS and mortality. The validity of lactate (LAC) and lactate contingent on age (LAC + AGE) were assessed using the area under the curve (AUC) of the receiver operating characteristics (ROC) curve. We used a logistic regression model to predict the probability of an ISS > 15.
Results
During the study period we included 325 patients, 75 met exclusion criteria. Mean age was 43 years (Min.: 11, Max.: 90, SD: 18.7) with a mean ISS of 8.4 (SD: 8.99). LAC showed a sensitivity of 0.82 with a specificity of 0.62 with an optimal cutoff at 1.72 mmol/l to predict an ISS > 15. The AUC of the ROC for LAC was 0.764 (95% CI: 0.67–0.85). The LAC + AGE model provided a significantly improved predictive value compared to LAC (0.765 vs. 0.828, p < 0.001).
Conclusions
The serum lactate concentration is able to predict injury severity. The prognostic value improves significantly taking the patients age into consideration. The combination of serum lactate and age could be a suitable Ad-on to existing two-tier triage protocols to minimize undertriage.
Level of evidence: Level IV, retrospective cohort study.


Similar content being viewed by others
Availability of data and materials
The data set generated and analyzed during the current study is not publicly accessible but is available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Newgard CD, Staudenmayer K, Hsia RY, Mann NC, Bulger EM, Holmes JF, et al. The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health Aff (Millwood). 2013;32:1591–9. https://doi.org/10.1377/hlthaff.2012.1142.
Newgard CD, Yang Z, Nishijima D, McConnell KJ, Trent SA, Holmes JF, et al. Cost-effectiveness of field trauma triage among injured adults served by emergency medical services. J Am Coll Surg. 2016;222:1125–37. https://doi.org/10.1016/j.jamcollsurg.2016.02.014.
Linder F, Holmberg L, Eklöf H, Björck M, Juhlin C, Mani K. Better compliance with triage criteria in trauma would reduce costs with maintained patient safety. Eur J Emerg Med. 2019;26:283–8. https://doi.org/10.1097/MEJ.0000000000000544.
Jenkins P, Rogers J, Kehoe A, Smith JE. An evaluation of the use of a two-tiered trauma team activation system in a UK major trauma centre. Emerg Med J. 2015;32:364–7. https://doi.org/10.1136/emermed-2013-203402.
MacKenzie E, Weir S, Rivara F, et al. The value of trauma center care. J Trauma. 2010;69:1–10. https://doi.org/10.1097/TA.0B013E3181E03A21.
Scott M, Abouelela W, Blitzer D, Murphy W. Trauma service utilization increases cost but does not add value for minimally injured patients. Value Health. 2020;23:705–9. https://doi.org/10.1016/J.JVAL.2020.02.009.
van der Sluijs R, Fiddelers A, Waalwijk J, Reitsma J. The impact of the trauma triage app on pre-hospital trauma triage: design and protocol of the stepped-wedge, cluster-randomized TESLA trial. Diagnostic Progn Res. 2020. https://doi.org/10.1186/S41512-020-00076-1.
Linder F, Holmberg L, Bjorck M, Juhlin C, Thorbjornsen K, Wisinger J, et al. A prospective stepped wedge cohort evaluation of the new national trauma team activation criteria in Sweden—the TRAUMALERT study. Scand J Trauma Resusc Emerg Med. 2019;27:1–10. https://doi.org/10.1186/s13049-019-0619-1.
Davis T, Dinh M, Roncal S, Byrne C, Petchell J, Leonard E, et al. Prospective evaluation of a two-tiered trauma activation protocol in an Australian major trauma referral hospital. Injury. 2010;41:470–4. https://doi.org/10.1016/j.injury.2010.01.003.
Voskens FJ, Van Rein EAJ, Van Der Sluijs R, Houwert RM, Lichtveld RA, Verleisdonk EJ, et al. Accuracy of prehospital triage in selecting severely injured trauma patients. JAMA Surg. 2018;153:322–7. https://doi.org/10.1001/jamasurg.2017.4472.
Schweigkofler U, Sauter M, Wincheringer D, Barzen S, Hoffmann R. Emergency room activation due to trauma mechanism TT - Schockraumindikation nach Unfallhergang. Unfallchirurg. 2019. https://doi.org/10.1007/s00113-019-00733-1.
Van Rein EAJ, Houwert RM, Gunning AC, Lichtveld RA, Leenen LPH, Van Heijl M. Accuracy of prehospital triage protocols in selecting severely injured patients: a systematic review. J Trauma Acute Care Surg. 2017;83:328–39. https://doi.org/10.1097/TA.0000000000001516.
Martín-Rodríguez F, López-Izquierdo R, Medina-Lozano E, Ortega Rabbione G, del Pozo VC, Carbajosa Rodríguez V, et al. Accuracy of prehospital point-of-care lactate in early in-hospital mortality. Eur J Clin Invest. 2020. https://doi.org/10.1111/eci.13341.
Brown JB, Lerner EB, Sperry JL, Billiar TR, Peitzman AB, Guyette FX. Prehospital lactate improves accuracy of prehospital criteria for designating trauma activation level. J Trauma Acute Care Surg. 2016;81:445–52. https://doi.org/10.1097/TA.0000000000001085.
Baxter J, Cranfield KR, Clark G, Harris T, Bloom B, Gray AJ. Do lactate levels in the emergency department predict outcome in adult trauma patients? A systematic review. J Trauma Acute Care Surg. 2016;81:555–66. https://doi.org/10.1097/TA.0000000000001156.
Guyette FX, Meier EN, Newgard C, McKnight B, Daya M, Bulger EM, et al. A comparison of prehospital lactate and systolic blood pressure for predicting the need for resuscitative care in trauma transported by ground. J Trauma Acute Care Surg. 2015;78:600–6. https://doi.org/10.1097/TA.0000000000000549.
Hagebusch P, Faul P, Klug A, Gramlich Y, Hoffmann R, Schweigkofler U. Elevated serum lactate levels and age are associated with an increased risk for severe injury in trauma team activation due to trauma mechanism. Eur J Trauma Emerg Surg. 2021. https://doi.org/10.1007/S00068-021-01811-Z.
Raa A, Sunde GA, Bolann B, Kvåle R, Bjerkvig C, Eliassen HS, et al. Validation of a point-of-care capillary lactate measuring device (Lactate Pro 2). Scand J Trauma Resusc Emerg Med. 2020. https://doi.org/10.1186/s13049-020-00776-z.
Galvagno SM, Sikorski RA, Floccare DJ, Rock P, Mazzeffi MA, DuBose JJ, et al. Prehospital point of care testing for the early detection of shock and prediction of lifesaving interventions. Shock. 2020;54:710–6. https://doi.org/10.1097/SHK.0000000000001567.
Martín-Rodríguez F, López-Izquierdo R, Delgado Benito JF, Sanz-García A, del Pozo VC, Castro Villamor MÁ, et al. Prehospital point-of-care lactate increases the prognostic accuracy of national early warning score 2 for early risk stratification of mortality: results of a multicenter. Observ Study J Clin Med. 2020;9:1156. https://doi.org/10.3390/jcm9041156.
Wilson MS, Konda SR, Seymour RB, Karunakar MA. Early predictors of mortality in geriatric patients with trauma. J Orthop Trauma. 2016;30:e299-304. https://doi.org/10.1097/BOT.0000000000000615.
Hashmi A, Ibrahim-Zada I, Rhee P, Aziz H, Fain MJ, Friese RS, et al. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76:894–901. https://doi.org/10.1097/TA.0b013e3182ab0763.
Kodadek LM, Selvarajah S, Velopulos CG, Haut ER, Haider AH. Undertriage of older trauma patients: Is this a national phenomenon? J Surg Res. 2015;199:220–9. https://doi.org/10.1016/j.jss.2015.05.017.
Uribe-Leitz T, Jarman MP, Sturgeon DJ, Harlow AF, Lipsitz SR, Cooper Z, et al. National study of triage and access to trauma centers for older adults. Ann Emerg Med. 2020;75:125–35. https://doi.org/10.1016/j.annemergmed.2019.06.018.
Wentling J, Krall SP, McNierney A, Dewey K, Richman PB, Blow O. Predictive value of point-of-care lactate measurement in patients meeting level II and III trauma team activation criteria that present to the emergency department: a prospective study. J Emerg Trauma Shock. 2019;12:203–8. https://doi.org/10.4103/JETS.JETS_120_18.
Martín-Rodríguez F, López-Izquierdo R, Castro Villamor MA, Mangas IM, Del Brío IP, Delgado Benito JF, et al. Prognostic value of lactate in prehospital care as a predictor of early mortality. Am J Emerg Med. 2019;37:1627–32. https://doi.org/10.1016/j.ajem.2018.11.028.
Magnusson C, Herlitz J, Höglind R, Wennberg P. Prehospital lactate levels in blood as a seizure biomarker: a multi-center observational study. Epilepsia. 2021;62:408–15. https://doi.org/10.1111/EPI.16806.
Baron BJ, Nguyen A, Stefanov D, Shetty A, Zehtabchi S. Clinical value of triage lactate in risk stratifying trauma patients using interval likelihood ratios. Am J Emerg Med. 2018;36:784–8. https://doi.org/10.1016/j.ajem.2017.10.015.
Bertil Bouillon, Pieper D. S3-Leitlinie Polytrauma / Schwerverletzten-Behandlung. AWMF Regist 2016.
Bolorunduro OB, Villegas C, Oyetunji TA, Haut ER, Stevens KA, Chang DC, et al. Validating the injury severity score (ISS) in different populations: ISS predicts mortality better among hispanics and females. J Surg Res. 2011;166:40–4. https://doi.org/10.1016/j.jss.2010.04.012.
Braken P, Amsler F, Gross T. Simple modification of trauma mechanism alarm criteria published for the TraumaNetwork DGU® may significantly improve overtriage—a cross sectional study. Scand J Trauma Resusc Emerg Med. 2018;26:1–10. https://doi.org/10.1186/s13049-018-0498-x.
Maliziola C, Frigerio S, Lanzarone S, Barale A. Sensitivity and specificity of trauma team activation protocol criteria in an Italian trauma center: a retrospective observational study. Int Emerg Nurs. 2019;44:20–4. https://doi.org/10.1016/J.IENJ.2019.02.002.
Stuke L, Duchesne J, Hunt J, Marr A, et al. Mechanism of injury is not a predictor of trauma center admission. Am Surg. 2013;79:1149–53.
Rotondo M, Cribari C, Smith R. Resources for optimal care of the traumatised patient. 6th ed. Chicago: American College of Surgeons; 2014.
Davis JW, Dirks RC, Kaups KL, Tran P. Base deficit is superior to lactate in trauma. Am J Surg. 2018;215:682–5. https://doi.org/10.1016/j.amjsurg.2018.01.025.
Gale SC, Kocik JF, Creath R, Crystal JS, Dombrovskiy VY. A comparison of initial lactate and initial base deficit as predictors of mortality after severe blunt trauma. J Surg Res. 2016;205:446–55. https://doi.org/10.1016/j.jss.2016.06.103.
Raux M, Le Manach Y, Gauss T, Baumgarten R, Hamada S, Harrois A, et al. Comparison of the prognostic significance of initial blood lactate and base deficit in trauma patients. Anesthesiology. 2017;126:522–33. https://doi.org/10.1097/ALN.0000000000001490.
Javali R, Ravindra P, Patil A, Srinivasarangan M. A clinical study on the initial assessment of arterial lactate and base deficit as predictors of outcome in trauma patients. Indian J Crit Care Med. 2017;21:719–25. https://doi.org/10.4103/IJCCM.IJCCM_218_17.
Swan KL, Keene T, Avard BJ. A 12-month clinical audit comparing point-of-care lactate measurements tested by paramedics with in-hospital serum lactate measurements. Prehosp Disaster Med. 2018;33:36–42. https://doi.org/10.1017/S1049023X17007130.
Ter Avest E, Griggs J, Wijesuriya J, Russell MQ, Lyon RM. Determinants of prehospital lactate in trauma patients: a retrospective cohort study. BMC Emerg Med. 2020. https://doi.org/10.1186/s12873-020-00314-1.
Dezman Z, Comer A, Smith G. Failure to clear elevated lactate predicts 24-hour mortality in trauma patients. J Trauma Acute Care Surg. 2015;79:580–5. https://doi.org/10.1097/TA.0000000000000810.
Klein K, Lefering R, Jungbluth P, Lendemans S, Hussmann B. Is prehospital time important for the treatment of severely injured patients? A matched-triplet analysis of 13,851 patients from the TraumaRegister DGU®. Biomed Res Int. 2019. https://doi.org/10.1155/2019/5936345.
Jagan N, Morrow LE, Walters RW, Plambeck RW, Patel TM, Moore DR, et al. Sympathetic stimulation increases serum lactate concentrations in patients admitted with sepsis: implications for resuscitation strategies. Ann Intensive Care. 2021. https://doi.org/10.1186/s13613-021-00805-9.
Kushimoto S, Akaishi S, Sato T, Nomura R, Fujita M, Kudo D, et al. Lactate, a useful marker for disease mortality and severity but an unreliable marker of tissue hypoxia/hypoperfusion in critically ill patients. Acute Med Surg. 2016;3:293–7. https://doi.org/10.1002/ams2.207.
Cannon CM, Miller RT, Grow KL, Purcell S, Nazir N. Age-adjusted and expanded lactate thresholds as predictors of all-cause mortality in the emergency department. West J Emerg Med. 2020;21:1249. https://doi.org/10.5811/WESTJEM.2020.5.46811.
Salottolo KM, Mains CW, Offner PJ, Bourg PW, Bar-Or D. A retrospective analysis of geriatric trauma patients: venous lactate is a better predictor of mortality than traditional vital signs. Scand J Trauma Resusc Emerg Med. 2013. https://doi.org/10.1186/1757-7241-21-7.
Van Rein EAJ, Van Der Sluijs R, Voskens FJ, Lansink KWW, Houwert RM, Lichtveld RA, et al. Development and validation of a prediction model for prehospital triage of trauma patients. JAMA Surg. 2019. https://doi.org/10.1001/jamasurg.2018.4752.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
PH (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) is the corresponding author. PF (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) made substantial contributions to the conception, the design of the work, the acquisition, the analysis and interpretation of data and was a major contributor in writing the manuscript. CR (University Medical Center Mainz—Interdisciplinary Center Clinical Trials (IZKS)) made substantial contributions to the conception and the analysis and interpretation of data. PS (Hospital of the Goethe University Frankfurt /Main, Department of Trauma, Hand and Reconstructive Surgery) made substantial contributions to the conception and design of the work and substantively revised it. IM (Hospital of the Goethe University Frankfurt/Main, Department of Trauma, Hand and Reconstructive Surgery) made substantial contributions to the conception and design of the work and substantively revised it. RH (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) made substantial contributions to the conception and design of the work and substantively revised it. US (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) made substantial contributions to the conception, the design of the work, the acquisition, the analysis and interpretation of data and substantively revised it. YG (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) made substantial contributions to the conception, the design of the work, the acquisition, the analysis and interpretation of data and substantively revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors listed below declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Corresponding author Dr. Paul Hagebusch, MD. BG Unfallklinik Frankfurt am Main, Department of Trauma and Orthopedic Surgery. Dr. Philipp Faul, MD, BG Unfallklinik Frankfurt am Main, Department of Trauma and Orthopedic Surgery. Dr. Christian Ruckes, University Medical Center Mainz, Interdisciplinary Center Clinical Trials (IZKS). PD Dr. Philipp Störmann, MD, Hospital of the Goethe University Frankfurt/Main, Department of Trauma, Hand and Reconstructive Surgery. Prof. Dr. Ingo Marzi, MD, PhD, Hospital of the Goethe University Frankfurt/Main, Department of Trauma, Hand and Reconstructive Surgery. Prof. Dr. Dr. Reinhard Hoffmann, MD, PhD, BG Unfallklinik Frankfurt am Main, Department of Trauma and Orthopedic Surgery. PD Dr. Uwe Schweigkofler, MD, PhD, BG Unfallklinik Frankfurt am Main, Department of Trauma and Orthopedic Surgery. PD Dr. Yves Gramlich, MD, PhD, BG Unfallklinik Frankfurt am Main, Department of Trauma and Orthopedic Surgery.
Ethical approval
The protocol of investigation was checked and approved by the Regional Ethics Committee (2020-1746-evBO).
Consent to participate
The requirement for informed consent was waived due to the retrospective study design.
Rights and permissions
About this article
Cite this article
Hagebusch, P., Faul, P., Ruckes, C. et al. The predictive value of serum lactate to forecast injury severity in trauma-patients increases taking age into account. Eur J Trauma Emerg Surg (2022). https://doi.org/10.1007/s00068-022-02046-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-022-02046-2