Abstract
Purpose
Frailty is known to increase vulnerability to stressful factors, and motivate a higher morbidity and mortality in several health conditions. However, long-term impact of frailty after surgical procedures remains unclear. The purpose of this study was to evaluate the relationship between frailty and long-term clinical outcomes after emergency surgery.
Methods
Prospective cohort study in patients older than 70 years undergoing emergency procedures. A total of 82 patients (mean age 78.5 years, 53.3% women) were consecutively enrolled. Data on demographics, surgical procedures, complications after 30 postoperative days, and frailty according to the clinical frailty scale, Triage Risk Screening Tool (TRST), and FRAIL scale were recorded. Readmission, mortality, and transition to frailty rates were analyzed at 6 and 18 months postoperatively.
Results
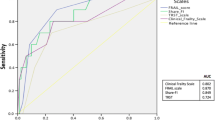
The prevalence of frailty ranged between 14.6 and 29.6% depending on the scale used. The overall mortality rate at 18 months was 19.5% (16 patients), and the survival curves demonstrated a significant difference in mortality between frail and non-frail patients assessed using the FRAIL scale and TRST (p = 0.049 and p = 0.033, respectively), with a hazard ratio of 2.28 (95% confidence interval 1.24–6.44). Logistic regression analysis showed that diabetes (p = 0.013) was an independent risk factor for transition to frailty, and antidepressant drug use was close to statistical significance (p = 0.08).
Conclusion
Frailty is a predictive marker of long-term mortality in patients undergoing emergency procedures. Diabetes and depression may represent independent risk factors for transition to frailty over time.


Similar content being viewed by others
References
Hogan DB, Maxwell CJ, Afilalo J, Arora RC, Bagshaw SM, Basran J, et al. A scoping review of frailty and acute care in middle- aged and older individuals with recommendations for future research. Can Geriatr J. 2017;20:22.
Rockwood K, Stadnyk K, MacKnight C, McDowell I, Hébert R, Hogan DB. A brief clinical instrument to classify frailty in elderly people. Lancet. 1999;353:205–6.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–156156.
Khan M, Jehan F, Zeeshan M, et al. Failure to rescue after emergency general surgery in geriatric patients: does frailty matter? J Surg Res. 2019;233:397–402.
Joseph B, Pandit V, et al. Emergency general surgery in the elderly: too old or too frail? J Am Coll Surg. 2016;222(5):805–13.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol Ser A Biol Sci Med Sci. 2004;59:M255–263263.
Cigolle CT, Ofstedal MB, Tian Z, Blaum CS. Comparing models of frailty: the health and retirement study. J Am Geriatr Soc. 2009;57:830–9.
Abizanda P, Romero L, Sánchez-Jurado PM, Martínez-Reig M, Gómez-Arnedo L, Alfonso SA. Frailty and mortality, disability and mobility loss in a Spanish cohort of older adults: the FRADEA study. Maturitas. 2013;74:54–60.
Woo J, Yu R, Wong M, Yeung F, Wong M, Lum C. Frailty screening in the community using the FRAIL scale. J Am Med Dir Assoc. 2015;16:412–9.
Carpenter CR, Shelton E, Fowler S, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med. 2015;22:1–21.
Rodríguez-queraltó O, Formiga F, López-palop R, et al. FRAIL scale also predicts long-term outcomes in older patients with acute coronary syndromes. J Am Med Dir Assoc. 2019;21:683–7.
Buurman BM, van den Berg W, Korevaar JC, Milisen K, de Haan RJ, de Rooij SE. Risk for poor outcomes in older patients discharged from an emergency department: feasibility of four screening instruments. Eur J Emerg Med. 2011;18(4):215–20.
Ethun CG, Bilen MA, Jani AB, Maithel SK, Ogan K, Master VA. Frailty and cancer: Implications for oncology surgery, medical oncology, and radiation oncology. CA Cancer J Clin. 2017;67:362–77.
Alonso Salinas GL, Sanmartin M, Pascual Izco M, Rincon LM, Pastor Pueyo P, Marco del Castillo A, et al. Frailty is an independent prognostic marker in elderly patients with myocardial infarction. Clin Cardiol. 2017;40:925–31.
Robinson TN, Wu DS, Stiegmann GV, Moss M. Frailty predicts increased hospital and 6-month healthcare cost following colorectal surgery in older adults. Am J Surg. 2011;202:511–4.
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath F-A. Laparoscopic colorectal surgery confers lower mortality in the elderly: a systematic review and meta-analysis of 66,483 patients. Surg Endosc. 2015;29:322–33.
Tan HL, Theng S, Chia X, Nadkarni NV, Ang SY. Frailty and functional decline after emergency abdominal surgery in the elderly: a prospective cohort study. World J Emerg Surg. 2019;14:1–7.
Murphy PB, Savage SA, Zarzaur BL. Impact of patient frailty on morbidity and mortality after common emergency general surgery operations. J Surg Res. 2019;247:95–102.
Arteaga SA, Aguilar LT, Tinoco JG, Ciuró FP, Ruiz JP. Impact of frailty in surgical emergencies. A comparison of four frailty scales. Eur J Trauma Emerg Surg. 2020;47:1613–9.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Mei F, Gao Q, Chen F, et al. Frailty as a predictor of negative health outcomes in chronic kidney disease: a systematic review and meta-analysis. J Am Med Dir Assoc. 2020. (Published online ahead of print, 2020 Nov 17).
Lee KC, Streid J, Sturgeon D, Lipsitz S, Weissman JS, Rosenthal RA, et al. The impact of frailty on long-term patient oriented outcomes after emergency general surgery: a retrospective cohort study. J Am Geriatr Soc. 2020;68(5):1037–43.
Maxwell CA, Mion LC, Mukherjee K, et al. Preinjury physical frailty and cognitive impairment among geriatric trauma patients determine postinjury functional recovery and survival. J Trauma Acute Care Surg. 2016;80(2):195–203.
Hajek A, Brettschneider C, Posselt T, et al. Predictors of frailty in old age - results of a longitudinal study. J Nutr Health Aging. 2016;20(9):952–7.
Lee JS, Auyeung TW, Leung J, Kwok T, Woo J. Transitions in frailty states among community-living older adults and their associated factors. J Am Med Dir Assoc. 2014;15(4):281–6.
Acknowledgements
Authors acknowledge the contribution of the Gastrointestinal Surgery Department at University Hospital Virgen del Rocío, for support and full collaboration during the whole study period.
Funding
The authors declare that no funding was received in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest in relation to this article.
Ethical approval
The study was approved by the Ethics Committee of Hospital Universitario Virgen del Rocío. All participants granted their consent to participate in the study. All of the authors have confirmed the preservation of confidentiality and respect of patients’ rights in the document of author responsibilities, publication agreement and transfer of rights to the European Journal of Trauma and Emergency Surgery.
Additional information
The present work was carried out in the Universitary Hospital Virgen del Rocío, Seville, Spain.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sánchez Arteaga, A., Tinoco González, J., Tallón Aguilar, L. et al. Long-term influence of frailty in elderly patients after surgical emergencies. Eur J Trauma Emerg Surg 48, 3855–3862 (2022). https://doi.org/10.1007/s00068-021-01818-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01818-6