Abstract
Background
A stepwise multidisciplinary team (MDT) approach to the injured trauma patient has been reported to have an overall benefit, with reduction in mortality and improved morbidity. Based on clinical experience, we hypothesized that implementation of a dedicated Spinal Cord Injury Service (SCIS) would impact outcomes of a patient specific population on the trauma service.
Methods
The trauma center registry was retrospectively queried, from January 2011 through December 2015, for patients presenting with a spinal cord injury. In 2013, a twice weekly rounding SCIS MDT was initiated. This new multidisciplinary service, the post-SCIS, was compared to the 2011–2012 pre-SCIS. The two groups were compared across patient demographics, mechanism of injury, surgical procedures, and disposition at discharge. The primary outcome was mortality. Secondary endpoints also included the incidence of complications, hospital length of stay (HLOS), ICU LOS, ventilator free days, and all hospital-acquired infectious complications. Logistic regression and Student’s t test were used to analyze data.
Results
Ninety-five patients were identified. Of these patients, 41 (43%) pre-SCIS and 54 (57%) post-SCIS patients were compared. Mean age was 46.9 years and 79% male. Overall, adjusted mortality rate between the two groups was significant with the implementation of the post-SCIS (p = 0.033). In comparison, the post-SCIS revealed shorter HLOS (23 vs 34.8 days, p = 0.004), increased ventilator free days (20.2 vs 63.3 days, p < 0.001), and less nosocomial infections (1.8 vs 22%, p = 0.002). While the post-SCIS mean ICU LOS was shorter (12 vs 17.9 days, p = 0.089), this relationship was not significant.
Conclusions
The application of an SCIS team in addition to the trauma service suggests that a structured coordinated approach can have an expected improvement in hospital outcomes and shorter length of stays. We believe that this clinical collaboration provides distinct specialist perspectives and, therefore, optimizes quality improvement.
Level of evidence Epidemiologic study, level III.
Similar content being viewed by others
Introduction
Traumatic spinal cord injuries (TSCI) are associated with significant physical challenges and psychosocial illness. Organ system dysfunction, both acute and chronic, are expected, thereby increasing morbidity and worsening quality-of-life. TSCI, oftentimes devastating and life-altering, pose distinct challenges to the patient, family, and healthcare system. The National Spinal Cord Injury Statistical Center (NSCISC) published review series estimates in the United States (US) an incidence of 40 cases per million per year [1]. In 2012, approximately 276,000 individuals are living with SCI in the US [1].
A stepwise multidisciplinary team (MDT) approach to the injured trauma patient can have an overall benefit to patient outcomes, with improved morbidity and decreased in-hospital mortality [2–4]. A multidisciplinary approach to management during the acute phase of TSCI provides a fundamental understanding and goal-oriented strategy. The majority of reports on TSCI do not reflect a team-based approach. The objective of this study was to determine whether the implementation of a dedicated Spinal Cord Injury Service (SCIS) would impact overall outcomes of a patient specific population on the trauma service.
Methods
Between January 1, 2011 and December 31, 2015, all trauma patients presenting to Grand Strand Medical Center, a level II trauma center in Myrtle Beach, South Carolina, were retrospectively reviewed. Following institutional review board approval, the trauma registry was queried for all TSCIs with inclusion criteria met by the primary diagnosis established with the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes. The following ICD-9-CM codes were categorized by: fracture of vertebral column with spinal cord injury (806.00–806.9) and spinal cord injury without evidence of spinal bone injury (952.00–952.9). Exclusion criteria included all non-trauma-related SCIs, cerebral vascular accident-related deficits, and trauma patients with neurologic deficits which resolved, as well as those without radiographic evidence of spinal cord injury.
Those who met inclusion criteria had medical records reviewed by a single investigator. As such, the patient population included the following spinal injuries: anterior, posterior, and central cord syndromes, paraplegia, and quadriplegia/tetraplegia. Patients were then grouped into two distinct hospital admission time periods, January 2011–July 2012 (pre-SCIS) and August 2012–December 2015 (post-SCIS). The two groups were compared across patient demographics, mechanism of injury, surgical procedures, and disposition at discharge. The primary outcome between the two groups was mortality. Secondary outcome variables included all hospital-acquired infections, ventilator days, hospital length of stay (HLOS), intensive care unit (ICU) LOS, decubitus ulcer formation, and other unexpected complications.
Statistical analysis
The major endpoint during this retrospective review was mortality. Secondary endpoints also included the incidence of complications, HLOS, ICU LOS, ventilator free days and all hospital-acquired infectious complications [urinary tract infection (UTI), ventilator-associated pneumonia (VAP), and surgical wounds]. Continuous data were compared with unpaired Student’s t tests and categorical proportions with χ 2 analysis or Fisher’s exact test, as appropriate. Logistic regression was used to examine the independent associations of several demographic and injury related factors. p values less than 0.05 were considered statistically significant. Statistical analysis was performed with the QI Macros © software (KnowWare International Inc., CO, USA).
Results
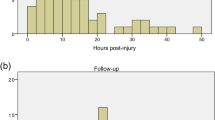
During the 72-month review, 95 patients were identified with TSCI. The mean (±SD) age was 46.9 ± 19.0 (range 19–103 years) and 76.8% (n = 73) male. Table 1 demonstrates the comparative demographics between the two TSCI groups, 41 (43%) patients in pre-SCIS group versus (vs) 54 (57%) post-SCIS group. Injury resulted from blunt (86.3%) vs penetrating (13.7%) trauma. The most common type of mechanism overall resulted from falls (45.3%), followed by motor vehicle collision (18.9%). Table 2 defines all TSCI types encountered on admission. Central cord syndrome (54.7%) and paraplegia (26.3%) were the most common types of TSCI in the study population. The majority of the injuries were to the cervical region (72%). In total, 63.2% had neurosurgical spine stabilization, with a mean of 3 days for both TSCI groups.
On performing multivariate analysis between the two groups, the post-SCIS group had an overall shorter HLOS (23.0 vs 34.8 days, p = 0.004). While the mean ICU LOS of post-SCIS implementation was shorter than the pre-SCIS (11.9 vs 17.9 days, p = 0.089), this relationship was not significant. Shorter ventilator days (20.2 vs 63.3 days, p < 0.001) and less nosocomial infections (1.9% vs 22.0%, p = 0.002) were also observed in the post-SCIS (Table 3). Patients were more likely to be discharged to a specialized spinal rehabilitation facility in the post-SCIS (29.6%) group (p = 0.023). Final discharge disposition is summarized in Table 4.
The overall mortality rate was 5.3% among the two groups. (Table 3) One death did occur on the post-SCIS as a result of a withdraw of care. On further analysis of the pre-SCIS mortality rate, the pre-SCIS was 5.7 times more likely to expire (odds ratio 5.73; 95% confidence interval 0.62–53.4; p = 0.087). The adjusted mortality rate when excluding the isolated post-SCIS death revealed statistical significance (p = 0.033).
Discussion
TSCIs are devastating life-changing events, and while relatively uncommon, represent a major health care burden. Since the 1920s, the American College of Surgeons has developed and dedicated efforts to improve quality of care to the injured. Specialized centers have traditionally maintained comprehensive integrated teams and healthcare delivery models to enhance care with clinical team decision-making, the mainstay of developing an MDT. Our study reports the benefit of the MDT approach to a patient specific trauma population, which can potentially benefit all hospital trauma systems.
To improve patient outcomes, several hospital specialties have implemented multidisciplinary in-hospital teams with improvement in patient outcomes [5–10]. Approximately 80% of cancer patients in England are assessed by an MDT, compared to 20% 10 years prior [10]. Carling et al. series instituted similar principles and practices with a multidisciplinary antibiotic management program to help minimize their inappropriate use and thereby decrease nosocomial infections and resistance [7]. The concept of multidisciplinary cancer conferences (MCC) was also designed to enhance patient management and to optimize outcomes through inter- and intra-disciplinary discussions similar to that of the MDT approach [6]. The common conclusion interpreted by Croke et al. was that multidisciplinary clinics, conferences, and MDTs are associated with improved survival [6].
Mandates for multidisciplinary assessment exist in several healthcare models predominately with oncologic care. The Commission on Cancer of the American College of Surgeons makes MCCs mandatory for the accreditation of hospitals responsible for providing multidisciplinary cancer care [8]. At the same time, the UK National Institute for Health and Clinical Excellence (NICE) encourages the management of all cancer patients by specialty-specific multidisciplinary teams. Several studies clearly demonstrate improvement in outcomes with coordinated treatment plans associated with MDTs and cancer patients [5, 6, 8–10].
Although acute trauma care in the United States may not be labeled as MDTs, a daily collaborative team approach is observed between the trauma team leader who coordinates treatment among the nursing staff and subspecialties, such as interventional radiology, orthopedics, anesthesiology, and emergency medicine [11, 12]. Since 2012, 117 Level 1 and Level 2 trauma centers have opened in the U.S., bringing the total of such facilities to more than 520, according to the American Trauma Society [13]. The resources available at a trauma center can be costly, requiring continuous staffing regardless of patient volume [14]. The future viability of trauma centers is vulnerable to the escalating cost of care provided to uninsured patients [14]. The unfortunate reality for many trauma facilities in the United States is that resources remain limited primarily by rising healthcare cost which are often reflected by the lack of additional hospital personnel support.
A major drawback with the pre-SCIS era was the lack of stability by the frequent alternating staff which included the trauma surgeon, physician assistant, pharmacist, therapists, and nursing staff and in some cases due to lack of staffing. These inconsistencies fell far short of fitting any needs of the spinal cord injured patient as demonstrated in our series. The post-SCIS provided a permanent structured staff characterized by the same trauma attending, clinical pharmacist, rehabilitative therapists, and social worker. All staff volunteered to remain as permanent members of the SCIS MDT as budgeting included more staffing, our first step to a successful program. At the same time, our facility instituted computerized TSCI admission order sets which thereby eliminated any variability in treatment by the admission trauma surgeon.
According to the 2013 Healthcare Cost and Utilization Project Internet tool (HCUPnet), a mean charge for a spinal cord injury hospitalization totaled $189,354 [15]. Jain et al. proposed that no relationship was found between total charges and patient sex or age; however, a difference did exist with the type of cord injury treated [16]. At the same time, Baaj et al. when comparing SCI to a non-SCI group, there was approximately a threefold increase in hospital charges [17]. Our overall HLOS decreased by 11.8 days and ICU LOS by 6.0 days, with an average of 43.1 less ventilator days associated with SCIS implementation, an assumed total cost savings benefit to our institution. The Centers for Medicare and Medicaid Services (CMS) address no payment for treatment of hospital-acquired infections. Pressure ulcer stages III and IV, as well as, urinary and vascular-associated catheter infections are familiar problems in TSCI patients, potentially associated with lost payment claims for healthcare facilities. By CMS definition, our SCIS had less CMS reported events; therefore, appropriate payments were provided without consequence [18].
The integration of the SCIS extended our relationship to regional spinal rehabilitation centers, where 29.6% of those discharged to rehab were to spinal rehab centers, compared to 9.8% prior to its application. On the other hand, previous series report approximately 50% of patients with SCIs will still require continued care at a skilled nursing facility (SNF) after hospital discharge [19]. The inpatient hospital MDT model could conceivably stand promising in the post-hospital setting if similar principles are established and appropriate personnel available.
Despite progressive understanding of SCI and advances in surgical treatment, Baaj et al. address cervical spine injury patients with lack of improvement in status at discharge, resulting in no significant changes with LOS, in-hospital mortality rate, or need for SNF after discharge [17]. While no statistical significance was evident in our study regarding mortality, our single post-SCIS death resulted from a withdrawal of care at family’s request. The use of MDT limits adverse events, improves overall patient outcomes, and adds to patient and employee satisfaction [20–22]. The clinical application of an MDT to TSCI stems from the overall success experienced in other healthcare models. Our clinical performance improvement was directly related to the SCIS and the HLOS, ventilator free days, nosocomial infections, and overall mortality.
In the current literature, known determinants of rehabilitation outcomes in patients with SCI include: age, sex, race, neurological level and extent of the lesion, number of associated injuries, mechanical ventilation, and employment status and education level at time of injury [1, 23]. TSCIs at first impression to patients and families appear life-limiting. Development of the TSCI service provided an effective outlet for patients, families, and healthcare staff to express concerns while also providing psychosocial and informative support. Hwang et al. patient- and family-centered satisfaction survey displayed improvements by the availability of family meetings and physician communication [24]. Our study provides a unique experience and a relatively feasible project that involves already established specialties services, including: physical, occupational, and respiratory therapist, a nutritionist, pharmacist, neurosurgical and orthopedic services, a wound care specialist and dedicated case management. The key principles to our MDT biweekly SCI service include:
-
collaboration of surgical specialist and other allied healthcare professionals;
-
development and implementation of SCI bundle order sets for standardization of care;
-
coordination of operative interventions between surgical services;
-
patient care and family education: expected inpatient goals and mental health care needs;
-
social lifestyle changes at discharge: personal mobility and residential modifications.
Findings in our study should be interpreted in light of its limitations. Our study was retrospective in nature and utilized only the data from a single trauma center. We did not differentiate a cumulative summary of injuries, a factor that can lead to longer hospitalizations. The consistent use of a defined spinal injury classification systems such as the AOSpine fracture classification or the American Spinal Injury Association (ASIA) impairment scale for SCI impairment was not compared as the ASIA score was not utilized until the development of the SCIS. However, we believe that this was represented in our mean ISS (± SD) among the two groups: pre-SCIS ISS 18.5 ± 11.5 and post-SCIS ISS of 22.1 ± 9.1 (p = 0.097), which did not underestimate the severity of injury among the two groups (Table 1). The majority of our patient population consisted of young patients, which may not be a clear representation of other treating facilities. With an aging population, SCI incidence may increase among the elderly over time. This may warrant further prospective studies to reinforce the importance of an MDT approach to TSCI patients in both pre- and post-hospital settings.
In conclusion, our findings underline the need for a TSCI service at busy treating facilities. The application of a SCIS team, in addition to the trauma service, suggests that a structured coordinated approach to this injury specific patient population can have an expected improvement in hospital outcomes and shorter length of stays. We believe that this clinical collaboration provides distinct specialist perspectives and, therefore, optimizing quality improvement.
References
National Spinal Cord Injury Statistical Centre (NSCISC) Birmingham A. Spinal cord injury facts and figures at a glance. Alabama, 2012.
Tubb CC, Oh JS, DO NV, Tai NR, Meissel MP, Place ML. Trauma care at a multinational United Kingdom-led Role 3 combat hospital: resuscitation outcomes from a multidisciplinary approach. Mil Med. 2014;179(11):1258–62.
Bach JA, Leskovan JJ, Scharschmidt T, Boulger C, Papadimos TJ, Russell S, Bahner DP, Stawicki SP. The right team at the right time: multidisciplinary approach to multi-trauma patient with orthopedic injuries. OPUS 12 Sci. 2012;6(1):6–10.
Georgiou A, Lockey DJ. The performance and assessment of hospital trauma teams. Scan J Trauma Resusc Emerg Med. 2010;18:66.
Fleissig A. Multidisciplinary teams in cancer care: are they effective in the UK? Lancet Oncol. 2006;7(11):935–43.
Croke JM, El-Sayed S. Multidisciplinary management of cancer patients: chasing a shadow or real value? An overview of the literature. Curr Oncol. 2012;19(4):e232–e8.
Carling P. Favorable impact of a multidisciplinary antibiotic management program conducted during 7 years. Infect Control Hosp Epidemiol. 2003;24(9):699–706.
Wright FC, De Vito C, Langer B, Hunter A. On behalf of the Expert Panel on Multidisciplinary Cancer Conference Standards Multidisciplinary cancer conferences: a systematic review and development of practice standards. Eur J Cancer. 2007;43:1002–10.
Stephens MR, Lewis WG, Brewster AE, et al. Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer. Dis Esophagus. 2006;19:164–71.
Griffith C, Turner J. United Kingdom National Health Service, Cancer Services Collaborative “Improvement Partnership”: redesign of cancer services, a national approach. Eur J Surg Oncol. 2004;30(suppl 1):1–86.
D’Amours SK, Rstogi P, Ball CG. Utility of simultaneous interventional radiology and operative surgery in a dedicated suite for seriously injured patients. Curr Opin Crit Care. 2013;19(6):587–93.
Cherry RA, King TS, Carney DE, Bryant P, Cooney RN. Trauma team activation and the impact on mortality. J Trauma. 2007;63:326–30.
American Trauma Society (ATS). Website: http://www.amtrauma.org. Accessed 21 Dec 2016.
Faul M, Sasser SM, Lairet J, Mould-Millman NK, Sugerman D. Trauma center staffing, infrastructure, and patient characteristics that influence trauma center need. West J Emerg Med. 2015;16(1):98–106.
U.S. Department of Health and Human Services. Healthcare Cost and Utilization Project Internet tool (HCUP). Facts and Figures: Statistics on Hospital-based Care in the United States. http://hcupnet.ahrq.gov. Accessed 12 Feb 2016.
Jain A, Brooks JT, Roa SS, Ain MC, Sponseller PD. Cervical fractures with associated spinal cord injury in children and adolescents: epidemiology, costs, and in-hospital mortality rates in 4418 patients. J Child Orthop. 2015;9:171–5.
Baaj AA, Uribe JS, Nichols TA, Theodore N, Crawford NR, Sonntag VK, Vale FL. Health care burden of cervical spine fractures in the United States: analysis of a nationwide database over a 10-year period. J Neurosurg Spine. 2010;13(1):61–6.
Peasah SK, McKay NL, Harman JS, Al-Amin M, Cook RL. Medicare non-payment of hospital-acquired: infection rates three years post implementation. Medicare Medicaid Res Rev. 2013;3(3):1–13.
Rick H. Spinal cord injury registry. Spinal cord injury facts and statistics. Vancouver, British Columbia, Canada 2006, 1–11.
Epstein NE. Multidisciplinary in-hospital teams improve patient outcomes: A review. Surg Neurol Int. 2014;5(Suppl 7):S295–303.
Kesson EM, Allardice GM, George WD, Burns HJ, Morrison DS. Effects of multidisciplinary team working on breast cancer survival: retrospective, comparative, interventional cohort study of 13 722 women. BMJ. 2012;344:e2718.
Boxer MM., Vinod SK, Shafiq J, Duggan KJ. Do multidisciplinary team meetings make a difference in the management of lung cancer? Cancer. 2011;117(22):5112–20.
Parent S, Dimar J, Dekutoski M, Roy-Beaudry M. Unique features of pediatric spinal cord injury. Spine (Phila Pa 1976). 2010;35(21 Suppl):S202–8.
Hwang DY, Yagoda D, Perrey HM, Tehan TM, Guanci M, Ananian L, Currier PF, Cobb JP, Rosand J. Assessment of satisfaction with care among family members of survivors in a neuroscience intensive care unit. J Neurosci Nurs. 2014;46:106–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest or funding reported by the above authors: Georgina Alizo MD, Jason D. Sciarretta MD, Stefanie Gibson AS, Keely Muertos MPH, Sharon Holmes BSN, Felicia Denittis PA-C, Joseph Cheatle MD, John Davis MD, and Antonio Pepe MD.
Rights and permissions
About this article
Cite this article
Alizo, G., Sciarretta, J.D., Gibson, S. et al. Multidisciplinary team approach to traumatic spinal cord injuries: a single institution’s quality improvement project. Eur J Trauma Emerg Surg 44, 245–250 (2018). https://doi.org/10.1007/s00068-017-0776-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0776-8