Abstract
Introduction
Damage control laparotomy (DCL) and the open abdomen have been well accepted following either severe abdominal trauma or emergency surgical disease. As DCL is increasingly utilized as a therapeutic option, appropriate management of the post-DCL patient is important. Early caloric support by enteral nutrition (EN) in the critically ill patient improves wound healing and decreases septic complications, lung injury, and multi-system organ failure. However, following DCL, nutritional strategies can be challenging and, at times, even daunting.
Conclusions
Even though limited data exist, the use of early EN following DCL seems safe, provided that the patient is not undergoing active resuscitation or the bowel is not in discontinuity. It is unknown as to whether EN in the open abdomen reduces septic complications, prevents enterocutaneous fistula (ECF), or alters the timing of definitive abdominal wall closure. Future investigation in a prospective manner may help elucidate these important questions.
Similar content being viewed by others
Introduction
In the last two decades, the role of damage control laparotomy (DCL) following severe abdominal trauma has been intensely studied. Appropriate indications, including severe intraoperative coagulopathy, prolonged metabolic acidosis, and abnormal coagulation profiles, seem to improve overall mortality, decrease blood transfusions, and decrease intensive care unit (ICU) length of stay and complications [1, 2]. The indications for DCL have broadened outside of abdominal trauma, in particular, to treat the consequences of abdominal compartment syndrome (ACS) and abdominal hypertension, leading to the concept of decompressive laparotomy [3, 4]. ACS may result from massive fluid resuscitation, severe burns, septic and hemorrhagic shock, mesenteric ischemia, vascular emergencies, acute pancreatitis, or even retroperitoneal space-occupying lesions, such as tumors or acute hemorrhage [5–7]. Recently, Miglietta et al. [8] have even advocated the use of DCL to treat refractory intracranial hypertension following traumatic brain injury. Therefore, with DCL increasing as a therapeutic option, appropriate management of the post-DCL patient is imperative. Indeed, several challenges exist in managing the open abdomen [9–11]. These challenges include:
-
1.
Timing of abdominal wall closure and methods of temporary closure.
-
2.
Assessment of volume loss and fluid replacement strategies.
-
3.
Appropriate concomitant medications such as antibiotics and paralytic agents.
-
4.
Optimal nutritional support.
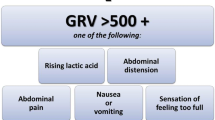
Despite being seemingly unrelated, these strategies are clinically interwoven and must be managed collectively. It has been well established that early caloric support by enteral nutrition (EN) in the critically ill patient improves wound healing, decreases septic complications, lung injury, and multi-system organ failure (MSOF) [12–15]. In this review, we will focus on the strategies and importance of nutritional support in the open abdomen following DCL (Fig. 1).
Schematic for nutritional support in the open abdomen following damage control laparotomy (DCL). When possible, enteral nutrition (EN) should be implemented as soon as resuscitation and physiologic stability has occurred. Total parenteral nutrition (TPN) should only be utilized in cases of bowel discontinuity or proximal enterocutaneous fistula (ECF)
Physiologic considerations of the open abdomen
Specific physiologic alterations following DCL depend greatly on the indications surrounding the original operation. Patients undergoing DCL following severe abdominal trauma often have ongoing metabolic alterations, including persistent acidosis, hypocoagulability, and significant electrolyte abnormalities [16, 17]. Most patients require continuing resuscitation with blood products and crystalloid in combination with vasopressor support to maintain adequate central perfusion pressure. Patients often have significant bowel wall and mucosal edema, with some requiring small or large bowel resection, where the bowel may be left in discontinuity [18]. Aggressive abdominal packing is commonly performed not only in the outer quadrants of the abdomen, but also within the small bowel mesentery or the retroperitoneum. Open abdomens exude protein-rich fluid, exacerbating nitrogenous losses. In a prospective study of 20 open abdomens following DCL, a mean loss of 2 g nitrogen/1 L of abdominal fluid was extrapolated over 3 days, with an average of 7 L of total abdominal fluid collected [19]. Furthermore, DCL patients are hypermetabolic with increased circulating inflammatory cytokines, which can lead to significant end-organ dysfunction, including pulmonary failure and renal insufficiency [20]. Definitive closure of an open abdomen, if achievable, varies and is highly dependent on the original etiology and ongoing patient physiologic status. In a large review of 276 patients surviving original DCL, 65 % were able to be definitively closed primarily, with 29 % undergoing temporizing closure [11]. These studies, and others, have shown that the longer the delay in abdominal closure, the more likely the development of complications, including wound infection, intraabdominal abscess, and, most ominous, enterocutaneous fistula (ECF) [21].
Given these physiologic and anatomic complexities, it is important that nutritional support must not be neglected. However, even though the open abdomen may have signs of distention and dysfunction, the administration of total parenteral nutrition (TPN) instead of EN should not reflexively occur. Early studies have irrefutably shown the benefits of early EN in the acute trauma patient when compared to TPN, including decreasing ventilator days, sepsis, and MSOF [12, 14]. These benefits are perhaps best seen when nutrition is started within the first 48 h following admission [15]. As the continued hypermetabolic response to injury occurs, ongoing protein catabolism heightens the risk of malnutrition [22]. Complicating things further, open abdomens behave like a fluid, with the electrolytes and protein sump adding an additional 20–30 % increase in metabolic demands following an acute injury [23]. Given the clear benefits of early EN and the perceived obstacles of EN in the open abdomen, we approach the central question: Is it safe and effective to provide adequate EN in patients with an open abdomen?
Benefits of EN in the open abdomen
Adequately controlled Level I evidence does not exist discerning the safety and efficacy of EN in the open abdomen. Diaz et al. [10], in a well-researched analysis of managing the open abdomen patient, cited the lack of adequate studies guiding nutritional management following DCL. Therefore, intensivists often use individual or institutional experience of managing nutritional support in these patients. In an effort to simplify existing data, we will analyze the effect of EN following DCL and the open abdomen, quantifying four metrics:
-
1.
Adequate nutritional goals.
-
2.
Time to definitive closure.
-
3.
Development of ECF.
-
4.
Complications and mortality.
Adequate nutritional goals
The assessment of adequate nutritional goals must be performed on all patients requiring DCL [24]. Realistically, the initial period focuses on intense resuscitation and correction of metabolic and coagulation parameters. Once physiologic stabilization has ensued, caloric requirements should be calculated. It is important to remember that estimated basal energy expenditures may underestimate the amount of protein lost from an open abdomen given the previously stated leakage of protein-rich fluid from the abdominal cavity [19, 25, 26]. Standard nutritional measures, including serum pre-albumin, albumin, transferrin, and C-reactive protein, may confirm return to an anabolic profile, but do not represent short-term nor acute nutritional changes needed, especially during the first 2–5 days following injury. In a case report detailing nutritional support following DCL, McKibbin et al. [23] estimated that basal energy expenditure increased by 40 %. Despite TPN followed by EN, their patient only improved their serum pre-albumin to 11.0 mg/dL (from a baseline of 8.9 mg/dL) 24 days after admission. In this patient, nutrition was delayed 4 days following injury due to ongoing resuscitation and hemodynamic instability. In one of the first retrospective reports, Tsuei et al. [27] analyzed 14 patients (9 male and 5 female) requiring DCL who also received at least 4 days of EN prior to definitive facial closure. Nutritional goals were estimated by using the Harris–Benedict equation or by indirect calorimetry to calculate the predicted energy expenditure. EN was provided using a small-bore nasoduodenal catheter, although the exact tube feeding recommendation was not specified. In total, 57 % of patients received at least 80 % of their predicted energy expenditure during open abdominal feeding, with a mean serum prealbumin of 9.8 ± 6.3 mg/dL. The authors also reported a 64 % intolerance to EN, including diarrhea and gastric reflux. These issues were all transient, with diarrhea resolving by increased fiber and gastric reflux by catheter repositioning. In another study, Byrnes et al. [28] analyzed 23 patients undergoing DCL retrospectively. These patients were divided into two groups: Group I (n = 12) underwent EN before fascial closure and Group II (n = 11) underwent EN after fascial closure. Half of all patients were fed through surgical jejunostomy, 25 % via nasal-jejunal catheters, and 25 % via naso-gastric catheters. The authors did not report how nutritional goals were determined, but all patients were able to receive EN, with 66 % of patients tolerating the goal rates of their EN regimens. In one of the largest comparative studies from Vanderbilt University, Collier et al. [29] analyzed 78 patients following DCL and delineated these patients into two groups: initiation of EN within 4 days (n = 43) and initiation of EN after 4 days (n = 35). In general, nearly half of all patients studied met the nutritional goals of EN by postoperative day 6.
Even though the data are limited, two general themes prevail. First, patients with DCL have significantly elevated nutritional requirements and protein losses; therefore, consideration of these losses must be given when completing a nutritional assessment. Second, unless patients are requiring ongoing resuscitation, have bowel discontinuity, or have significant bowel ischemia and edema, EN seems to be reasonably well tolerated, with achievable nutritional goals. The evidence also suggests that distal feeding, via either nasal or surgically placed catheters, seem to be preferred over gastric feeding.
Time to definitive closure
Reticence to initiate EN may be the perceived risk of exacerbating bowel wall edema or exacerbation of postoperative ileus, hence, delaying and complicating definitive facial closure. Despite this clinical practice, the literature, mostly from observations and experiments in the critically ill patient, tend to favor early feeding, with improvement in bowel edema. In a rodent model, Kozar et al. [30] has shown that EN improves vascular flow to and from the bowel, promoting the movement of lymph, improving venous return, and, consequently, reducing bowel edema. In a classic study evaluating the post-surgical gut weight in rats, Zaloga et al. [31] showed that EN regimens significantly reduced the gut weight, presumably by improving efferent gut flow. Unfortunately, these experimental observations have not translated directly to experience in the open abdomen. In a retrospective study of 100 patients undergoing DCL, Dissanaike et al. [32] stratified patients into two groups: early EN within 36 h (n = 32) and a late EN after 36 h (n = 68). The late EN group started EN within a mean of 7.3 days. No differences in the Injury Severity Score (ISS), base deficit, crystalloid volume, blood transfusion, or vasopressor use existed between each group. In each group, nearly 94 % of patients had definitive closure; however, the early EN group trended towards earlier closure, with closure at 6.47 ± 0.83 days versus 8.55 ± 0.85 days. This difference did not meet statistical significance. Collier et al. [29] did find significance in their comparison. Again, the patient demographics were well matched in each group, including blood product resuscitation and initial base deficit. Early EN had 74 % of patients definitively closed in <8 days versus 49 % of patients receiving late EN. In either study, it was unclear as to whether the fascia was primarily juxtaposed or if mesh product was needed. Byrnes et al. [28] was able to achieve 100 % closure in all 23 patients, with 66 % having primary fascial closure and 35 % needing mesh components. However, early EN actually had a delay in definitive closure: 7 days versus 3.4 days in the late EN group.
Taken together, it is unclear as to whether the early initiation of EN will improve the time to perform definitive facial closure following DCL. It would be interesting to know if the authors noted any difference in bowel edema and, if so, to what degree between early and late EN groups. It would also be interesting to know the long-term results in terms of the incidence of incisional hernias and whether early EN may have had any effect in preventing the occurrence thereof. Finally, it is important to consider the frequency of operations following a DCL, since surgery is the most common reason to interrupt enteral nutrition in the ICU [33]. To date, there has been no data showing that discontinuing distal enteral feeds prevents aspiration in intubated patients; however, certain practice tendencies remain. Developing institutional protocols in conjunction with surgeons, intensivists, and anesthesiologists may prevent frequent feeding disruption and nutritional delay.
Enterocutaneous fistula
Perhaps the most dreaded complication from a DCL and open abdomen is the development of either single or multiple ECF. Much of the time, fistulae can actually form into the open abdomen itself and, hence, be classified as an enteroatmospheric fistula [34, 35]. The risk of fistulae formation is high given bowel exposure, highly hemodynamically unstable patients, and multiple abdominal explorations. Several series of DCL have reported the incidence of ECF to range from 5 to 20 % [11, 36]. Several protective measures can be utilized to prevent ECF, including early abdominal wall closure, protection of enteric contents, and appropriate and optimal dressings [35]. Similar to the worry over fascial closure, surgeons may be hesitant to begin EN due to the fear of promoting ECF formation, mostly from the perceived risks of increased intestinal edema and distention. However, the existing literature suggest that ECF in the open abdomen may be reduced with EN. In all 23 patients, Byrnes et al. [28] had no ECF complications. Interestingly, Collier et al. [29] showed a significant reduction in ECF formation when early EN was implemented. In their analysis, early EN had a 9 % rate of ECF versus 26 % in the late EN group. The classification, location, and duration of the ECF in this study is unknown, nor is the nutritional strategy implemented after the development of an ECF.
Once an ECF has developed, continued loss of volume, electrolyte abnormalities, and ongoing malnutrition further exacerbate the complexities of managing the open abdominal nutritional requirements. After appropriate resuscitation, anti-microbial therapy, and control of fistula effluent have been achieved, an attempt to discern the anatomic location of the fistula is important. In high-output fistula, most typically in the foregut and proximal midgut, TPN is often required [37]. In the distal ileum and colon however, EN can often still be implemented as long as the ECF output is carefully monitored, along with adjunctive nutritional profiles [38]. Definitive ECF closure and surgical correction should only be attempted during the latent phase of rehabilitation after nutritional parameters have been optimized.
Other complications and mortality
It stands to reason, based on the early work by Moore and Jones and Kudsk et al., that complications such as pneumonia, wound infections, and septic complications would also be decreased with early EN in the open abdomen population [12, 13]. In Collier et al.’s analysis, there was no difference between early or late EN in the development of empyema, bloodstream infections, wound infections, wound cellulitis, or urinary tract infections. There was also no difference in the hospital length of stay, ICU days, and mortality. Hospital costs in the early EN group were significantly lower, with a mean hospital charge of $122,283 in the early EN group versus $223,349 in the late EN group [29]. Interestingly, and in contrast to Moore and Jones, the rate of ventilator-associated pneumonia (VAP) was increased in early EN, with 67 % developing VAP compared to 49 % in the late EN group. It is not documented, however, as to how VAP was defined.
In contrast, Dissanaike et al. [32] showed a substantial decrease in VAP rates in the early EN group (43.8 %) versus the no EN group (72.1 %). Patients not receiving early EN also seemed to develop VAP at an earlier time point compared to those who received early EN. There was no statistical difference between ICU days, overall hospital length of stay, surgical wound infection, or bloodstream infection. Mortality trended to be less in the early EN group (12.5 %) versus the late EN group (23.5 %); however, this difference did not reach statistical significance. The authors noted that most cases of VAP seemed to be caused from enteric organisms (Escherichia coli, Klebsiella, and Enterobacter), suggesting that EN decreases the bacterial colonization of the gastrointestinal tract. Improvement in nutritional profiles between the groups did not seem to be the causative factor.
Final considerations
Given the paucity of literature and the retrospective nature of the current analyses, large, well conducted, prospective trials are clearly needed. Patients analyzed in the published studies are not randomized, and several confounding factors may exist. Nevertheless, certain recommendations can still be made:
-
1.
The initiation of early EN can be started following DCL if there is bowel continuity, adequate resuscitation and metabolic correction has been achieved, and hemodynamic lability has been stabilized. If bowel continuity is not achievable within 48 h, TPN should strongly be considered.
-
2.
Once EN is initiated, tight monitoring of nutritional profiles should occur to help guide caloric intake and assess protein balance.
-
3.
The concern over EN causing a delay in fascial closure does not seem warranted; however, EN improving the time to fascial closure is, as yet, uncertain.
-
4.
The development of ECF does not seem to be increased with early EN; however, protective measures should be optimized in order to prevent ECF occurrence.
-
5.
Early EN does not seem to decrease the length of hospital stay, wound infections, or mortality; however some evidence suggests that the incidence of VAP may be decreased, which may be by association and not causality.
DCL and the open abdomen will continue to be a challenging entity in any ICU. Nevertheless, aggressive nutritional support will, hopefully, prevent complications of the open abdomen and improve overall patient outcomes.
References
Rotondo MF, Schwab CW, McGonigal MD, et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35:375–82; discussion 382–3.
Waibel BH, Rotondo MF. Damage control in trauma and abdominal sepsis. Crit Care Med. 2010;38:S421–30.
Duchesne JC, Kimonis K, Marr AB, et al. Damage control resuscitation in combination with damage control laparotomy: a survival advantage. J Trauma. 2010;69:46–52.
Johnson JW, Gracias VH, Schwab CW, et al. Evolution in damage control for exsanguinating penetrating abdominal injury. J Trauma. 2001;51:261–69; discussion 269–71.
Cheatham ML. Intraabdominal pressure monitoring during fluid resuscitation. Curr Opin Crit Care. 2008;14:327–33.
Cheatham ML, Malbrain ML, Kirkpatrick A, et al. Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. II. Recommendations. Intensive Care Med. 2007;33:951–62.
Vidal MG, Ruiz Weisser J, Gonzalez F, et al. Incidence and clinical effects of intra-abdominal hypertension in critically ill patients. Crit Care Med. 2008;36:1823–31.
Miglietta MA, Salzano LJ, Chiu WC, et al. Decompressive laparotomy: a novel approach in the management of severe intracranial hypertension. J Trauma. 2003;55:551–54; discussion 554–5.
Dutton WD, Diaz JJ Jr, Miller RS. Critical care issues in managing complex open abdominal wound. J Intensive Care Med. 2012;27:161–71.
Diaz JJ Jr, Cullinane DC, Dutton WD, et al. The management of the open abdomen in trauma and emergency general surgery: part 1—damage control. J Trauma. 2010;68:1425–38.
Miller RS, Morris JA Jr, Diaz JJ Jr, et al. Complications after 344 damage-control open celiotomies. J Trauma. 2005;59:1365–71; discussion 1371–4.
Kudsk KA, Croce MA, Fabian TC, et al. Enteral versus parenteral feeding. Effects on septic morbidity after blunt and penetrating abdominal trauma. Ann Surg. 1992;215:503–11; discussion 511–3.
Moore EE, Jones TN. Benefits of immediate jejunostomy feeding after major abdominal trauma—a prospective, randomized study. J Trauma. 1986;26:874–81.
Moore FA, Moore EE, Jones TN, et al. TEN versus TPN following major abdominal trauma—reduced septic morbidity. J Trauma. 1989;29:916–22; discussion 922–3.
Heyland DK, Dhaliwal R, Drover JW, et al. Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN J Parenter Enteral Nutr. 2003;27:355–73.
Cohen MJ. Towards hemostatic resuscitation: the changing understanding of acute traumatic biology, massive bleeding, and damage-control resuscitation. Surg Clin North Am. 2012;92:877–91, viii.
Holcomb JB, Jenkins D, Rhee P, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62:307–10.
Ordoñez CA, Pino LF, Badiel M, et al. Safety of performing a delayed anastomosis during damage control laparotomy in patients with destructive colon injuries. J Trauma. 2011;71:1512–17; discussion 1517–8.
Cheatham ML, Safcsak K, Brzezinski SJ, et al. Nitrogen balance, protein loss, and the open abdomen. Crit Care Med. 2007;35:127–31.
Sido B, Teklote JR, Hartel M, et al. Inflammatory response after abdominal surgery. Best Pract Res Clin Anaesthesiol. 2004;18:439–54.
Ramsay PT, Mejia VA. Management of enteroatmospheric fistulae in the open abdomen. Am Surg. 2010;76:637–9.
Marik PE, Zaloga GP. Early enteral nutrition in acutely ill patients: a systematic review. Crit Care Med. 2001;29:2264–70.
McKibbin B, Cresci G, Hawkins M. Nutrition support for the patient with an open abdomen after major abdominal trauma. Nutrition. 2003;19:563–6.
Cothren CC, Moore EE, Ciesla DJ, et al. Postinjury abdominal compartment syndrome does not preclude early enteral feeding after definitive closure. Am J Surg. 2004;188:653–8.
Guillaume A, Seres DS. Safety of enteral feeding in patients with open abdomen, upper gastrointestinal bleed, and perforation peritonitis. Nutr Clin Pract. 2012;27:513–20.
Hourigan LA, Linfoot JA, Chung KK, et al. Loss of protein, immunoglobulins, and electrolytes in exudates from negative pressure wound therapy. Nutr Clin Pract. 2010;25:510–6.
Tsuei BJ, Magnuson B, Swintosky M, et al. Enteral nutrition in patients with an open peritoneal cavity. Nutr Clin Pract. 2003;18:253–8.
Byrnes MC, Reicks P, Irwin E. Early enteral nutrition can be successfully implemented in trauma patients with an “open abdomen”. Am J Surg. 2010;199:359–62; discussion 363.
Collier B, Guillamondegui O, Cotton B, et al. Feeding the open abdomen. JPEN J Parenter Enteral Nutr. 2007;31:410–5.
Kozar RA, Hu S, Hassoun HT, et al. Specific intraluminal nutrients alter mucosal blood flow during gut ischemia/reperfusion. JPEN J Parenter Enteral Nutr. 2002;26:226–9.
Zaloga GP, Black KW, Prielipp R. Effect of rate of enteral nutrient supply on gut mass. JPEN J Parenter Enteral Nutr. 1992;16:39–42.
Dissanaike S, Pham T, Shalhub S, et al. Effect of immediate enteral feeding on trauma patients with an open abdomen: protection from nosocomial infections. J Am Coll Surg. 2008;207:690–7.
Morgan LM, Dickerson RN, Alexander KH, et al. Factors causing interrupted delivery of enteral nutrition in trauma intensive care unit patients. Nutr Clin Pract. 2004;19:511–7.
Latifi R, Joseph B, Kulvatunyou N, et al. Enterocutaneous fistulas and a hostile abdomen: reoperative surgical approaches. World J Surg. 2012;36:516–23.
Friese RS. The open abdomen: definitions, management principles, and nutrition support considerations. Nutr Clin Pract. 2012;27:492–8.
Miller PR, Meredith JW, Johnson JC, et al. Prospective evaluation of vacuum-assisted fascial closure after open abdomen: planned ventral hernia rate is substantially reduced. Ann Surg. 2004;239:608–14; discussion 614–6.
Polk TM, Schwab CW. Metabolic and nutritional support of the enterocutaneous fistula patient: a three-phase approach. World J Surg. 2012;36:524–33.
Dubose JJ, Lundy JB. Enterocutaneous fistulas in the setting of trauma and critical illness. Clin Colon Rectal Surg. 2010;23:182–9.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bansal, V., Coimbra, R. Nutritional support in patients following damage control laparotomy with an open abdomen. Eur J Trauma Emerg Surg 39, 243–248 (2013). https://doi.org/10.1007/s00068-013-0287-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-013-0287-1