Abstract
Background
Given the reduction in death from breast cancer, as well as improvements in overall survival, adjuvant radiotherapy is considered the standard treatment for breast cancer. However, left-sided breast irradiation was associated with an increased rate of fatal cardiovascular events due to incidental irradiation of the heart. Recently, considerable efforts have been made to minimize cardiac toxicity of left-sided breast irradiation by new treatment methods such as deep-inspiration breath-hold (DIBH) and new radiation techniques, particularly intensity modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT). The primary aim of this study was to evaluate the effect of DIBH irradiation on cardiac dose compared with free-breathing (FB) irradiation, while the secondary objective was to compare the advantages of IMRT versus VMAT plans in both the FB and the DIBH position for left-sided breast cancer.
Methods
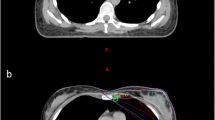
In all, 25 consecutive left-sided breast cancer patients underwent CT simulation in the FB and DIBH position. Five patients were excluded with no cardiac displacement following DIBH-CT simulation. The other 20 patients were irradiated in the DIBH position using respiratory gating. Four different treatment plans were generated for each patient, an IMRT and a VMAT plan in the DIBH and in the FB position, respectively. The following parameters were used for plan comparison: dose to the heart, left anterior descending coronary artery (mean dose, maximum dose, D25% and D45%), ipsilateral, contralateral lung (mean dose, D20%, D30%) and contralateral breast (mean dose). The percentage in dose reduction for organs at risk achieved by DIBH for both IMRT and VMAT plans was calculated and compared for each patient by each treatment plan.
Results
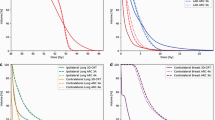
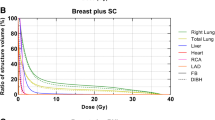
DIBH irradiation significantly reduced mean dose to the heart and left anterior descending coronary artery (LADCA) using both IMRT (heart –20%; p = 0.0002, LADCA –9%; p = 0.001) and VMAT (heart –23%; p = 0.00003, LADCA –16%; p = 0.01) techniques as compared with FB radiation. There were no significant changes in left lung dose by IMRT; however, with VMAT planning, mean dose to the left lung was reduced by –4% (p = 0.0004). In addition, DIBH significantly increased the mean dose to the contralateral breast with IMRT (+14%, p = 0.002) and significantly reduced the dose to the contralateral breast with VMAT planning (–9%, p = 0.003) compared with the FB position. Additionally, in comparison with VMAT, the IMRT technique reduced mean heart dose both in the FB and the DIBH-position by –30% (p = 0.0004) and –26% (p = 0.002), respectively. Furthermore, IMRT increased the mean dose to the left lung in both the FB and the DIBH position (+5%, p = 0.003, p = 0.006), respectively. There were no significant changes in dose to the right lung and contralateral breast either in the FB or DIBH position between IMRT and VMAT techniques.
Conclusion
Left-sided breast irradiation is best performed in the DIBH position, since a considerable dose sparing to the heart and LADCA can be achieved by using either IMRT or VMAT techniques. A significant additional decrease in heart and LADCA dose by IMRT in both FB and DIBH irradiation was seen compared with VMAT.
Zusammenfassung
Hintergrund
Auf der Basis von Metaanalysen, die eine signifikante Verbesserung der Lokalrezidivraten, aber auch des Überlebens zeigten, gilt die adjuvante Radiotherapie heute als Standardbehandlung nach brusterhaltender Therapie des Mammakarzinoms. Beim linksseitigen Mammakarzinom wurde allerdings eine erhöhte Rate fataler kardiovaskulärer Ereignisse infolge einer Exposition des Herzens mit ionisierender Strahlung ermittelt. Es besteht die Hypothese, dass diese kardiale Toxizität minimiert werden kann, und zwar durch die Bestrahlung in tiefer Inspiration (DIBH) und die Anwendung aktueller Techniken, insbesondere der intensitätsmodulierten Radiotherapie (IMRT) und der volumetrischen Rotationsbestrahlung (VMAT). Primäre Zielsetzung dieser Studie war, beim linksseitigen Mammakarzinom den Effekt der Radiotherapie in tiefer Inspiration auf die Herzbelastung im Vergleich zur freien Atmung zu zeigen. Des Weiteren sollten die Techniken der IMRT und der VMAT mit und ohne tiefe Inspiration verglichen werden.
Methoden
Insgesamt 25 konsekutiv eingeschlossene Patientinnen mit einem linksseitigen Mammakarzinom wurden nach brusterhaltender Operation einer CT-Simulation unterzogen. Datensätze in tiefer Inspiration und freier Atmung (Atemmittellage) wurden ermittelt. Fünf Patientinnen wurden wegen fehlender inspirationsabhängiger Beweglichkeit der ventralen Thoraxwand nach DIBH-CT-Stimulation ausgeschlossen. Die übrigen 20 Patientinnen erhielten eine normalfraktionierte Radiotherapie in DIBH-Technik. Für jede Patientin wurden vier verschiedene Bestrahlungspläne generiert, jeweils ein IMRT- und VMAT-Plan in DIBH-Technik und Atemmittellage. Folgende Parameter wurden für den Planvergleich herangezogen: Dosisbelastung von Herz und linker Koronararterie (LADCA; mittlere und maximale Dosis, D25% und D45%), der ipsilateralen und kontralateralen Lunge (mittlere Dosis, D20%, D30%) sowie der kontralateralen Mamma (mittlere Dosis). Die prozentualen Dosisreduktionen an den Risikoorganen infolge der DIBH-Technik wurden sowohl für IMRT- als auch für VMAT-Pläne kalkuliert und für jede individuelle Patientin zwischen den einzelnen Plänen verglichen.
Ergebnisse
Die DIBH-Bestrahlung führte zu einer signifikanten Reduktion der mittleren Dosis an Herz und LADCA, sowohl mit der IMRT- (Herz − 20 %, p = 0,0002; LADCA − 9 %, p = 0,001) als auch mit der VMAT-Technik (Herz − 23 %, p = 0,00003; LADCA − 16 %, p = 0,01) im Vergleich zur Bestrahlung in Atemmittellage. Die Dosis an der linken Lunge war durch die IMRT nicht signifikant verändert, bei VMAT-Planung war die mittlere Dosis jedoch um − 4% reduziert (p = 0,0004). Zusätzlich wurde infolge der DIBH-Bestrahlung im Vergleich zur Atemmittellage eine signifikant höhere Dosis an der kontralateralen Mamma mit der IMRT (+ 14 %, p = 0,002) gesehen, nach VMAT-Planung war die Dosis an der kontralateralen Brust signifikant verringert (− 9 %, p = 0,003). Zusätzlich reduzierte die IMRT-Technik im Vergleich zur VMAT die mittlere Herzdosis sowohl in Atemmittellage als auch nach DIBH-Positionierung um − 30 % (p = 0,0004) und − 26 % (p = 0,002). Im Vergleich zur VMAT führte die IMRT zu einer Dosiserhöhung an der linken Lunge, und zwar in Atemmittellage und DIBH-Position (+ 5 %, p = 0,003, p = 0,006). Die Dosis an der rechten Lunge und kontralateralen Mamma unterschied sich zwischen IMRT- und VMAT-Technik nicht, weder bei Atemmittellage noch bei DIBH-Positionierung.
Schlussfolgerung
Die Bestrahlung des linksseitigen Mammakarzinoms erfolgt am besten mithilfe der DIBH-Technik, zumal mit der IMRT wie auch mit der VMAT eine erhebliche Dosisreduktion an Herz und Koronararterien erreicht werden kann. Die IMRT kann im Vergleich zur VMAT-Bestrahlung eine zusätzliche Dosisreduktion an den genannten Risikoorganen sowohl in DIBH-Technik als auch in Atemmittellage erzielen.






Similar content being viewed by others
References
Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans E et al (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366:2087–2106
Overgaard M, Jensen MB, Overgaard J, Hansen PS, Rose C, Andersson M et al (1999) Postoperative radiotherapy in high-risk postmenopausal breast-cancerpatients given adjuvant tamoxifen: Danish Breast Cancer Cooperative GroupDBCG 82c randomised trial. Lancet 353:1641–1648
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378:1707–1716
Darby SC, McGale P, Taylor CW, Peto R (2005) Long-term mortality from heart diseaseand lung cancer after radiotherapy for early breast cancer: prospective cohortstudy of about 300.000 women in US SEER cancer registries. Lancet Oncol 6:557–565
Cuzick J, Stewart H, Rutqvist L et al (1994) Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol 12:447–453
Hooning MJ, Botma A, Aleman BMP et al (2007) Long-term risk of cardiovasculardisease in 10-year survivors of breast cancer. J Natl Cancer Inst 99:365–375
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Bronnum D et al (2013) Risk of ischemic heart disease in women after radiotherapy for breastcancer. N Engl J Med 368:987–998
Nissen HD, Appelt AL (2013) Improved heart, lung and target dose with deepinspiration breath hold in a large clinical series of breast cancer patients. Radiother Oncol 106:28–32
Vikstrom J, Hjelstuen MH, Mjaaland I, Dybvik KI (2011) Cardiac and pulmonarydose reduction for tangentially irradiated breast cancer, utilizing deepinspiration breath-hold with audio-visual guidance, without compromisingtarget coverage. Acta Oncol 50:42–50
Pignol JP, Olivotto I, Rakovitch E et al (2008) A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol 26 13:2085–2092
Mukesh MB, Barnett GC, Wilkinson JS et al (2013) Randomized controlled trial of intensity-modulated radiotherapy for early breast cancer: 5‑year results confirm superior overall cosmesis. J Clin Oncol 31 36:4488–4495
Ha B, Suh HS, Lee J et al (2013) Long-term results of forward intensity-modulated radiation therapy for patients with early-stage breast cancer. Radiat Oncol J 31(4):191–198
Cozzi L, Fogliata A, Nicolini G, Bernier J (2005) Clinical experience in breast irradiation with intensity modulated photon beams. Acta Oncol 44:467–474. doi:10.1080/02841860510029879
Fong A, Bromley R, Beat M et al (2009) Dosimetric comparison of intensity modulated radiotherapy techniques and standard wedged tangents for whole breast radiotherapy. J Med Imaging Radiat Oncol 53:92–99. doi:10.1111/j.1754-9485.2009.02043.x
Nicolini G, Clivio A, Fogliata A et al (2009) Simultaneousintegrated boost radiotherapy for bilateral breast: a treatmentplanning and dosimetric comparison for volumetricmodulated arc and fixed field intensity modulated therapy. Radiat Oncol 4:27
Naqvi SA, Mohiuddin MM, Yu CX (2010) Comparing radiation treatments using intensity-modulated beams, multiplearcs and single arc. Int J Radiat Oncol Biol Phys 76(5):1554–1562
Rana S (2013) Intensity modulated radiation therapy versusvolumetric intensity modulated arc therapy. J Medicalradiation Sci 60:81–83
Swamy ST, Radha CA, Kathirvel M et al (2014) Feasibilitystudy of deep inspiration breath-hold based volumetricmodulated arc therapy for locally advanced left sided breastcancer patients. Asian Pac J Cancer Prev 15:9033–9038
Nielsen MH, Berg M, Pedersen AN, Andersen K, Glavicic V, Jakobsen EH et al (2013) Delineation of target volumes and organs at risk in adjuvantradiotherapy of early breast cancer: National guidelines and contouringatlas by the Danish Breast Cancer Cooperative Group. Acta Oncol 52:703–710
Radiation therapy oncology group (2009) Breast cancer atlas for radiation therapyplanning: consensus definitions. http://www.rtog.org/CoreLab/ContouringAtlases/BreastCancerAtlas.aspx. Accessed 27 July 2015
Feng M, Moran JM, Koelling T, Chughtai A, Chan JL, Freedman L et al (2011) Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancer. Int J Radiat Oncol Biol Phys 79:10–18
Mehta V (2005) Radiation pneumonitis and pulmonary fibrosis in non-small-cell lung cancer: pulmonary function, prediction, and prevention. Int J Radiat Oncol Biol Phys 63:5–24
Kwa SL, Lebesque JV, Theuws JC, Marks LB, Munley MT, Bentel G et al (1998) Radiation pneumonitis as a function of mean lung dose: an analysis of pooled data of 540 patients. Int J Radiat Oncol Biol Phys 42:1–9
Zürl B, Stranzl H, Winkler P, Kapp KS (2010) Quantitative assessment of irradiated lung volume and lung mass in breast cancer patients treated with tangential fields in combination with deep inspiration breath hold (DIBH). Strahlenther Onkol 186(3):157–162. doi:10.1007/s00066-010-2064-y
Korreman SS, Pedersen AN, Nøttrup TJ, Specht L, Nyström H (2005) Breathingadapted radiotherapy for breast cancer: comparison of free breathinggating with the breath-hold technique. Radiother Oncol 76:311–318
Pedersen AN, Korreman S, Nyström H, Specht L (2004) Breathing adaptedradiotherapy of breast cancer: reduction of cardiac and pulmonary dosesusing voluntary inspiration breath hold. Radiother Oncol 72:53–60
Remouchamps VM, Vicini FA, Sharpe MB, Kestin LL, Martinez AA, Wong JW (2003) Significant reductions in heart and lung doses using deep inspiration breathhold with active breathing control and intensity modulated radiationtherapy for patients treated with locoregional breast irradiation. Int J Radiat Oncol Biol Phys 55:392–406
Hayden A, Rains M, Tiver K (2012) Deep inspiration breath hold technique reduces heartdose from radiotherapy for left-sided breast cancer with deep breath-holding. J Med Imaging Radiat Oncol 56:464–472
Yeung R, Conroy L, Long K, Walrath D, Li H, Smith W, Hudson A, Phan T (2015) Cardiac dose reduction with deep inspiration breath hold for left-sided breast cancer radiotherapy patients with and without regional nodal irradiation. Radiat Oncol 10:200. doi:10.1186/s13014-015-0511-8
Joo JH, Kim SS, Ahn SD, Kwak J, Jeong C, Ahn SH, Son BH, Lee JW (2015) Cardiac dose reduction during tangential breast irradiation using deep inspiration breath hold: a dose comparison study based on deformable image registration. Radiat Oncol 10:264. doi:10.1186/s13014-015-0573-7
Schönecker S, Walter F, Freislederer P, Marisch C, Scheithauer H, Harbeck N, Corradini S, Belka C (2016) Treatment planning and evaluation of gated radiotherapy in left-sided breast cancer patients using the CatalystTM/SentinelTM system for deep inspiration breath-hold (DIBH). Radiat Oncol 11(1):143
Mast ME, Heijenbrok MW, van Kempen-Harteveld ML, Petoukhova AL, Scholten AN, Wolterbeek R, Schreur JH, Struikmans H (2016) Less increase of CT-based calcium scores of the coronary arteries: Effect three years after breast-conserving radiotherapy using breath-hold. Strahlenther Onkol 192(10):696–704. doi:10.1007/s00066-016-1026-4
Nemoto K, Ogushi M, Nakajima M, Kozuka T, Nose T, Yamashita T (2009) Cardiacsparingradiotherapy for left breast cancer with deep breath-holding. Jpn J Radiol 27:259–263
Bahrainy M, Kretschmer M, Jöst V, Kasch A, Würschmidt F, Dahle J, Lorenzen J (2016) Treatment of breast cancer with simultaneous integrated boost in hybrid plan technique: Influence of flattening filter-free beams. Strahlenther Onkol 192(5):333–341. doi:10.1007/s00066-016-0960-5
Becker-Schiebe M, Stockhammer M, Hoffmann W, Wetzel F, Franz H (2016) Does mean heart dose sufficiently reflect coronary artery exposure in left-sided breast cancer radiotherapy?: Influence of respiratory gating. Strahlenther Onkol 192(9):624–631. doi:10.1007/s00066-016-1011-y
Ibrahim EM, Abouelkhair KM, Kazkaz GA, Elmasri OA, Al-Foheidi M (2012) Risk of second breast cancer in female Hodgkin’s lymphoma survivors: a meta-analysis. BMC Cancer 12:197
Zürl B, Stranzl H, Winkler P, Kapp KS (2013) Quantification of contralateral breast dose and risk estimate of radiation-induced contralateral breast cancer among young women using tangential fields and different modes of breathing. Int J Radiat Oncol Biol Phys 85(2):500–505. doi:10.1016/j.ijrobp.2012.04.016
Dobler B, Maier J, Knott B, Maerz M, Loeschel R, Koelbl O (2016) Second cancer risk after simultaneous integrated boost radiation therapy of right sided breast cancer with and without flattening filter. Strahlenther Onkol 192(10):687–695. doi:10.1007/s00066-016-1025-5
Hepp R, Ammerpohl M, Morgenstern C, Nielinger L, Erichsen P, Abdallah A, Galalae R (2015) Deep inspiration breath-hold (DIBH) radiotherapy in left-sided breast cancer: Dosimetrical comparison and clinical feasibility in 20 patients. Strahlenther Onkol 191(9):710–716. doi:10.1007/s00066-015-0838-y
Acknowledgements
The present work was carried out by M.S. in fulfillment of the requirements for obtaining the degree “Dr. med.” awarded by the Friedrich Alexander University of Erlangen-Nürnberg (FAU), 91054 Erlangen, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sakka, M., Kunzelmann, L., Metzger, M. et al. Cardiac dose-sparing effects of deep-inspiration breath-hold in left breast irradiation. Strahlenther Onkol 193, 800–811 (2017). https://doi.org/10.1007/s00066-017-1167-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-017-1167-0
Keywords
- Breast cancer
- Breast irradiation
- Cardiotoxicity
- Intensity modulated radiotherapy
- Volumetric modulated arc therapy