Abstract
Objective
To evaluate the effect of prophylactic cranial irradiation (PCI) on overall survival (OS) in patients with extensive small cell lung cancer (ESCLC).
Methods
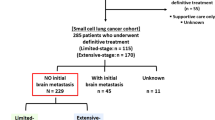
Between April 2005 and May 2014, 204 patients with ESCLC who had any response (according to RECIST 1.1) to initial chemotherapy were reviewed. All patients had undergone appropriate imaging tests to exclude brain metastases before initial chemotherapy. PCI was performed on 45 patients (22.1 %) and the remaining patients (77.9 %) received no such treatment (control group). Primary endpoint was OS. The incidence of brain metastases, brain metastases-free survival (BMFS), and adverse effects were also evaluated.
Results
Survival data of the 204 patients were analyzed statistically. PCI significantly prolonged median OS from 12.6 to 16.5 months as compared to the control group (hazard ratio, HR, 0.63; 95 % confidence interval, CI, 0.41 to 0.96; p = 0.033). PCI significantly lowered the risk of brain metastases (HR 0.48; 95 % CI 0.30 to 0.76; p = 0.001). The 1‑year incidence of brain metastases was 17.1 and 55.9 % in the PCI and control group, respectively. PCI significantly correlated with the increased median BMFS (p = 0.002). Additionally, multivariate analyses demonstrated that PCI was a favorable independent predictor of OS, BMFS, and the incidence of brain metastases. Acute and chronic adverse effects were generally low grade and well tolerated in patients receiving PCI.
Conclusion
PCI after any response to initial chemotherapy significantly improved OS of ESCLC patients analyzed in this study.
Zusammenfassung
Ziel
Beurteilung des Effekts der prophylaktischen kranialen Bestrahlung (PCI) auf das Gesamtüberleben (OS) bei Patienten mit ausgedehntem kleinzelligem Lungenkarzinom (ESCLC).
Methoden
Zwischen April 2005 und Mai 2014 wurden 204 Patienten mit ESCLC nach Ansprechen auf eine initiale Chemotherapie (gemäß RECIST 1.1) untersucht. Vor der Chemotherapie wurden bei allen Patienten Untersuchungen mit entsprechenden Bildgebungsverfahren durchgeführt, um Metastasen im Gehirn auszuschließen. 45 Patienten (22,1 %) wurden anschließend mit PCI behandelt, die übrigen (77,9 %) erhielten keine Behandlung (Kontrollgruppe). Der primäre Endpunkt der Studie war das OS. Ebenfalls beurteilt wurden das Auftreten von Hirnmetastasen, das hirnmetastasenfreie Überleben (BMFS) und Nebenwirkungen.
Ergebnisse
Die Daten zum Überleben der 204 Patienten wurden statistisch ausgewertet. Die PCI verlängerte das mittlere OS im Vergleich zur Kontrollgruppe signifikant von 12,6 Monaten auf 16,5 Monate (Hazard Ratio [HR]: 0,63; 95 %-Konfidenzintervall [KI]: 0,41–0,96; p = 0,033). Das Risiko von Hirnmetastasen wurde signifikant verringert (HR: 0,48; 95 %-KI: 0,30–0,76; p = 0,001). Die 1‑Jahres-Inzidenz von Hirnmetastasen betrug dabei 17,1 % in der PCI- und 55,9 % in der Kontrollgruppe. Zudem konnte ein signifikanter Zusammenhang zwischen PCI und dem mittleren BMFS festgestellt werden (p = 0,002). Multivariate Analysen zeigten zusätzlich, dass die PCI ein günstiger, unabhängiger Prädiktor für OS, BMFS und die Inzidenz von Hirnmetastasen ist. Akute und chronische Nebenwirkungen waren gering und wurden gut von den mit PCI behandelten Patienten vertragen.
Schlussfolgerungen
Das OS der in dieser Studie untersuchten Patienten mit ESCLC nach Ansprechen auf eine initiale Chemotherapie konnte durch PCI signifikant verbessert werden.



Similar content being viewed by others

References
Govindan R, Page N, Morgensztern D, Read W, Tierney R, Vlahiotis A et al (2006) Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol 24:4539–4544
Feld R, Pringle JF, Evans WK, Keen CW, Quirt IC, Curtis JE et al (1981) Combined modality treatment of small cell carcinoma of the lung. Arch Intern Med 141:469–473
Oberg K, Hellman P, Kwekkeboom D, Jelic S (2010) Neuroendocrine bronchial and thymic tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21(Suppl 5):v220–v222
Simon GR, Wagner H (2003) Small cell lung cancer. Chest 123:259S–271S
Socinski MA, Bogart JA (2007) Limited-stage small-cell lung cancer: the current status of combined-modality therapy. J Clin Oncol 25:4137–4145
Simon M, Argiris A, Murren JR (2004) Progress in the therapy of small cell lung cancer. Crit Rev Oncol Hematol 49:119–133
Chua YJ, Steer C, Yip D (2004) Recent advances in management of small-cell lung cancer. Cancer Treat Rev 30:521–543
Stupp R, Monnerat C, Turrisi AR, Perry MC, Leyvraz S (2004) Small cell lung cancer: state of the art and future perspectives. Lung Cancer 45:105–117
Schnabel T, Schmitt G (1993) The role of radiotherapy in the management of small cell lung cancer (SCLC). Strahlenther Onkol 169:329–338
Kurup A, Hanna NH (2004) Treatment of small cell lung cancer. Crit Rev Oncol Hematol 52:117–126
Seute T, Leffers P, Ten VG, Twijnstra A (2004) Neurologic disorders in 432 consecutive patients with small cell lung carcinoma. Cancer 100:801–806
Komaki R, Cox JD, Whitson W (1981) Risk of brain metastasis from small cell carcinoma of the lung related to length of survival and prophylactic irradiation. Cancer Treat Rep 65:811–814
Hardy J, Smith I, Cherryman G, Vincent M, Judson I, Perren T et al (1990) The value of computed tomographic (CT) scan surveillance in the detection and management of brain metastases in patients with small cell lung cancer. Br J Cancer 62:684–686
Arriagada R, Le Chevalier T, Riviere A, Chomy P, Monnet I, Bardet E et al (2002) Patterns of failure after prophylactic cranial irradiation in small-cell lung cancer: analysis of 505 randomized patients. Ann Oncol 13:748–754
Arriagada R, Le Chevalier T, Borie F, Riviere A, Chomy P, Monnet I et al (1995) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. J Natl Cancer Inst 87:183–190
Yang GY, Matthews RH (2000) Prophylactic cranial irradiation in small-cell lung cancer. Oncologist 5:293–298
Gregor A, Cull A, Stephens RJ, Kirkpatrick JA, Yarnold JR, Girling DJ et al (1997) Prophylactic cranial irradiation is indicated following complete response to induction therapy in small cell lung cancer: results of a multicentre randomised trial. United Kingdom Coordinating Committee for Cancer Research (UKCCCR) and the European Organization for Research and Treatment of Cancer (EORTC). Eur J Cancer 33:1752–1758
Auperin A, Arriagada R, Pignon JP, Le Pechoux C, Gregor A, Stephens RJ et al (1999) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic Cranial Irradiation Overview Collaborative Group. N Engl J Med 341:476–484
Meert AP, Paesmans M, Berghmans T, Martin B, Mascaux C, Vallot F et al (2001) Prophylactic cranial irradiation in small cell lung cancer: a systematic review of the literature with meta-analysis. BMC Cancer 1:5
Slotman B, Faivre-Finn C, Kramer G, Rankin E, Snee M, Hatton M et al (2007) Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med 357:664–672
Seto T, Takahashi T, Yamanaka T, Harada H (2014) Prophylactic cranial irradiation (PCI) has a detrimental effect on the overall survival (OS) of patients (pts) with extensive disease small cell lung cancer (ED-SCLC):Results of a Japanese randomized phase III trial [abstract. J Clin Oncol 32(Suppl 5):Abstract 7503 (http://meetinglibrary.asco.org/content/129034-144)
Seute T, Leffers P, Wilmink JT, Ten VG, Twijnstra A (2006) Response of asymptomatic brain metastases from small-cell lung cancer to systemic first-line chemotherapy. J Clin Oncol 24:2079–2083
Greenspoon JN, Evans WK, Cai W, Wright JR (2011) Selecting patients with extensive-stage small cell lung cancer for prophylactic cranial irradiation by predicting brain metastases. J Thorac Oncol 6:808–812
Kiricuta IC, Bohndorf W (1996) Adjuvant whole-brain irradiation in small-cell bronchial carcinoma. Strahlenther Onkol 172:553–558
Sas-Korczynska B, Korzeniowski S, Wojcik E (2010) Comparison of the effectiveness of “late” and “early” prophylactic cranial irradiation in patients with limited-stage small cell lung cancer. Strahlenther Onkol 186:315–319
Slotman BJ, van Tinteren H, Praag JO et al (2015) Use of thoracic radiotherapy for extensive stage small-cell lung cancer: a phase 3 randomised controlled trial. Lancet 385:36–42
Griesinger F (2014) ASCO 2014-Neues zu Lungentumoren. http://www.trillium.de/fileadmin/user_upload/Zeitschriften/Trillium_Krebsmedizin/Archiv/2014_2/asco_lungentumoren_griesinger.pdf. Accessed 21 May 2016
Acknowledgements
This work was jointly supported by the National Natural Science Foundation of China (11505012) and the Beijing Municipal Administration of Hospitals’ Youth Programme (QML20151004).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Chen, J. Li, Y. Hu, Y. Zhang, Z. Lin, Z. Zhao, and S. Jiao declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Yi Chen and Jinyu Li contributed equally to this work.
Rights and permissions
About this article
Cite this article
Chen, Y., Li, J., Hu, Y. et al. Prophylactic cranial irradiation could improve overall survival in patients with extensive small cell lung cancer. Strahlenther Onkol 192, 905–912 (2016). https://doi.org/10.1007/s00066-016-1038-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-1038-0