Abstract
Introduction
Inflammation has been reported to be associated with aortic dissection (AD), from the development to the prognosis of AD. In this study we aimed to find the role of the neutrophil-lymphocyte ratio (NLR) in the prediction of clinical events in patients with acute AD type A.
Patients and methods
The study comprised 37 patients who were hospitalized at our center between 2009 and 2013 with the diagnosis of acute AD type A.
Results
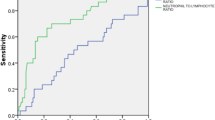
The mean NLR was significantly higher in patients with pericardial effusion than those without effusion (15.6 ± 11.4 vs. 7.5 ± 4.8, p = 0.005). An NLR value > 8.51 yielded an area under the curve (AUC) value of 0.829 [95 % confidence interval (CI) 0.674–0.984, p = 0.004], which demonstrated a sensitivity of 77 % and specificity of 74 % for the prediction of mortality.
Conclusions
The novel inflammatory marker NLR could be used to predict pericardial effusion and in-hospital mortality in patients with acute AD type A.
Zusammenfassung
Einleitung
Zum Zusammenhang von Inflammation und Aortendissektion (AD) ist publiziert worden, von ihrer Entwicklung einer AD bis zu ihrer Prognose. Ziel der Studie war es, die Rolle des Verhältnisses von Neutrophilen zu Lymphozyten („neutrophil/lymphocyte ratio“, NLR) in der Prädiktion von klinischen Ereignissen bei Patienten mit akuter AD vom Typ A zu eruieren.
Methoden
Die Studienpopulation bestand aus 37 Patienten, die zwischen 2009 und 2013 mit der Diagnose akute AD Typ A in unsere stationäre Behandlung aufgenommen worden waren.
Ergebnisse
Bei Patienten mit Pleuraerguss war die NLR signifikant höher als bei Patienten ohne Erguss (15,6 ± 11,4 vs. 7,5 ± 4,8, p = 0,005). Der NLR-Wert > 8,51 ergab einen AUC („area under the curve“)-Wert von 0,829 (95 %-KI 0,674–0,984; p = 0,004), entsprechend einer Sensitivität von 77 % und einer Spezifität von 74 % für die Prädiktion der Mortalität.
Fazit
Der neue Inflammationsmarker NLR ermöglicht bei akuter AD vom Typ A eine Prädiktion von Perikarderguss und stationärer Mortalität.




Similar content being viewed by others
References
Nienaber CA, Eagle KA (2003) Aortic dissection: new frontiers in diagnosis and management: part I: from etiology to diagnostic strategies. Circulation 108:628–635
Luo F, Zhou XL, Li JJ, Hui RT (2009) Inflammatory response is associated with aortic dissection. Ageing Res Rev 8:31–35
Suzuki T, Katoh H, Nagai R (1999) Biochemical diagnosis of aortic dissection: from bench to bedside. Jpn Heart J 40:527–534
Najjar SS, Scuteri A, Lakatta EG (2005) Arterial aging: is it an immutable cardiovascular risk factor? Hypertension 46:454–462
Isselbacher EM (2008) Diseases of the aorta. In: Libby P, Bonow R, Mann D, Zipes D (eds) Braunwald’s heart disease: a textbook of cardiovascular medicine, 8th edn. Elsevier Saunders, Philadelphia, p 1457e89
Allaire E, Schneider F, Saucy F et al (2009) New insight in aetiopathogenesis of aortic diseases. Eur J Vasc Endovasc Surg 37:531e7
He R, Guo DC, Estrera AL et al (2006) Characterization of the inflammatory and apoptotic cells in the aortas of patients with ascending thoracic aortic aneurysms and dissections. J Thorac Cardiovasc Surg 131:671–678
Li JJ, Fang CH (2004) C-reactive protein is not only an inflammatory marker but also a direct cause of cardiovascular diseases. Med Hypotheses 62:499–506
Papa A, Emdin M, Passino C et al (2008) Predictive value of elevated neutrophil-lymphocyte ratio on cardiac mortality in patients with stable coronary artery disease. Clin Chim Acta 395:27–31
Shen XH, Chen Q, Shi Y, Li HW (2010) Association of neutrophil/lymphocyte ratio with long-term mortality after ST elevation myocardial infarction treated with primary percutaneous coronary intervention. Chin Med J (Engl) 123:3438–3443
Tamhane UU, Aneja S, Montgomery D et al (2008) Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol 102:653–657
Hagan PG, Nienaber CA, Isselbacher EM et al (2000) The International Registry of Acute AD (IRAD): new insights into an old disease. JAMA 283:897–903
Imtiaz F, Shafique K, Mirza SS et al (2012) Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med 5:2
Folsom AR, Wu KK, Rosamond WD et al (1997) Prospective study of hemostatic factors and incidence of coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 96:1102–1108
Kuehl H, Eggebrecht H, Boes T et al (2008) Detection of inflammation in patients with acute aortic syndrome: comparison of FDG-PET/CT imaging and serological markers of inflammation. Heart 94:1472–1477
Reeps C, Essler M, Pelisek J et al (2008) Increased 18F-fluorodeoxyglucose uptake in abdominal aortic aneurysms in positron emission/computed tomography is associated with inflammation, aortic wall instability, and acute symptoms. J Vasc Surg 48:417–423 (discussion 424). doi:10.1016/j.jvs.2008.03.059
Isselbacher EM (2007) Epidemiology of thoracic aortic aneurysms, aortic dissection, intramural hematoma, and penetrating atherosclerotic ulcers. In: Baliga RR, Nienaber CA, Isselbacher EM, Eagle KA (eds) Aortic dissection and related syndromes. Springer Science, New York, p 3e15
Schillinger M, Domanovits H, Bayegan K et al (2002) C-reactive protein and mortality in patients with acute aortic disease. Intensive Care Med 28:740–745
Wen D, Wu HY, Jiang XJ et al (2011) Role of plasma C-reactive protein and white blood cell count in predicting in-hospital clinical events of acute type A aortic dissection. Chin Med J (Engl) 124:2678–2682
Sbarouni E, Georgiadou P, Marathias A et al (2007) D-dimer and BNP levels in acute aortic dissection. Int J Cardiol 122:170–172
Weber T, Hogler S, Auer J et al (2003) D-dimer in acute aortic dissection. Chest 123:1375–1378
Eggebrecht H, Naber CK, Bruch C et al (2004) Value of plasma fibrin D-dimer for detection of acute aortic dissection. J Am Coll Cardiol 44:804–809
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348:138–150
Bhutta H, Agha R, Wong J et al (2011) Neutrophil-lymphocyte ratio predicts medium-term survival following elective major vascular surgery: a cross-sectional study. Vasc Endovascular Surg 45:227–231. doi:10.1177/1538574410396590
Horne BD, Anderson JL, John JM et al (2005) Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol 45:1638–1643
Sarraf KM, Belcher E, Raevsky E et al (2009) Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg 137:425–428
Yamanaka T, Matsumoto S, Teramukai S et al (2007) The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology 73:215–220
Gomez D, Farid S, Malik HZ et al (2008) Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J Surg 32:1757–1762
Walsh SR, Cook EJ, Goulder F et al (2005) Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 91:181–184
Cho H, Hur HW, Kim SW et al (2009) Pre-treatment neutrophil to lymphocyte ratio is elevated in epithelial ovarian cancer and predicts survival after treatment. Cancer Immunol Immunother 58:15–23
Tian N, Penman AD, Mawson AR et al (2010) Association between circulating specific leukocyte types and blood pressure: the atherosclerosis risk in communities (ARIC) study. J Am Soc Hypertens 4:272–283
Compliance with ethical guidelines
Conflict of interest. S. Karakoyun, M.O. Gürsoy, T. Akgün, L. Öcal, M. Kalçık, M. Yesin, E. Erdoğans, S. Külahçıoğlu, R.B. Bakal, C. Köksal, M. Yıldız, and M. Özkan state that there are no conflicts of interest. All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karakoyun, S., Gürsoy, M., Akgün, T. et al. Neutrophil–lymphocyte ratio may predict in-hospital mortality in patients with acute type A aortic dissection. Herz 40, 716–721 (2015). https://doi.org/10.1007/s00059-014-4121-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-014-4121-2