Abstract
Introduction:
The increasing relevance of 3D methods in orthodontic diagnostics and treatment planning calls for the development of new analysis methods and the definition of three-dimensional mean values.
Objective:
The aim of this study was to develop a reliable threedimensional (3D) analysis of facial soft tissues. Our objectives were to determine vertical 3D mean values and define the relationship between vertical skeletal parameters and digitally-recorded 3D soft tissue parameters.
Patients and Methods:
A total of 100 adult patients (♀ = 53, ♂ = 47) of Caucasian ethnic origin were included in the study. Patients with syndromes, cleft lip and palate, noticeable asymmetry or anomalies in the number of teeth were excluded. Arithmetic means for three vertical 3D soft tissue parameters were calculated. The parameters were analyzed biometrically in terms of their reliability and gender-specific differences. Furthermore, the 3D soft tissue values were analyzed with regard to any correlations with vertical cephalometric values. In addition, we employed stepwise discriminant analysis, a multivariate statistical method, to examine the extent to which correct assessment of craniofacial morphology is possible by referring to those 3D parameters.
Results:
We successfully defined reproducible 3D mean values for the 3D soft tissue parameters, demonstrating highly significant correlations between the vertical 3D soft tissue measurements and cephalometric measurements. 89.8% of the patients could be correctly assigned to a vertical or horizontal craniofacial morphology according to the 3D soft tissue values.
Conclusion:
3D soft tissue analysis provides information about vertical skeletal parameters, allowing assessment of vertical craniofacial morphology. Further investigation will be required so that 3D soft tissue diagnosis can be integrated into treatment planning and assessment as a supportive diagnostic tool in the future.
Zusammenfassung
Einleitung:
Die zunehmende Relevanz von 3D-Verfahren im Rahmen der kieferorthopädischen Diagnostik und Therapieplanung erfordert die Entwicklung neuer Analyseverfahren sowie die Definition dreidimensionaler Durchschnittswerte.
Zielsetzung:
Ziel dieser Untersuchung war die Entwicklung einer reliablen dreidimensionalen (3D) Analyse der Gesichtsweichteile. Es sollten vertikale 3D-Durchschnittswerte bestimmt werden und die Beziehung zwischen vertikalen skelettalen Parametern und digital erfassten 3D-Weichteilparametern dargestellt werden.
Patienten und Methodik:
In die Studie eingeschlossen wurden 100 erwachsene Probanden (♀ = 53, ♂ = 47) kaukasischer Herkunft. Ausgeschlossen wurden Probanden mit Syndromen, LKGS-Spalten, auffälligen Asymmetrien oder Anomalien der Zahnzahl. Es wurden arithmetische Mittelwerte für drei vertikale 3D-Weichteilparameter ermittelt. Die Parameter wurden biometrisch hinsichtlich ihrer Reliabilität und geschlechtsspezifischer Unterschiede analysiert. Des Weiteren wurden die 3D-Weichteilwerte bezüglich bestehender Korrelationen zu vertikalen kephalometrischen Werten untersucht. Darüber hinaus wurde mittels eines multivariaten statischen Verfahrens, der schrittweisen Diskriminanzanalyse, überprüft, inwieweit anhand der untersuchten 3DParameter eine korrekte Beurteilung des Gesichtsschädelaufbaus möglich ist.
Ergebnisse:
Für die 3D-Weichteilparameter konnten reproduzierbare 3D-Durchschnittswerte definiert werden. Es konnten hochsignifikante Korrelationen zwischen den vertikalen 3D-Weichteilmessungen und den kephalometrischen Messungen nachgewiesen werden. 89,8% der Patienten konnten anhand der 3D-Weichteilwerte korrekt vertikalem oder horizontalem Gesichtsschädelaufbau zugeordnet werden.
Schlussfolgerung:
Die 3D-Weichteilanalyse lässt Aussagen über vertikale skelettale Parameter zu und ermöglicht eine Beurteilung des vertikalen Gesichtsschädelaufbaus. Weitere Untersuchungen sind wünschenswert, um die 3D-Weichteildiagnostik zukünftig als unterstützendes diagnostisches Instrument in die Behandlungsplanung und -bewertung integrieren zu können.
Similar content being viewed by others
References
Battagel JM. The identification of Class III malocclusions by discriminant analysis. Eur J Orthod 1994;16:71–80.
Burstone CJ. Lip posture and its significance in treatment planning. Am J Orthod 1967;53:262–84.
Burstone CJ. The integumental profile. Am J Orthod 1958;44:1–25.
Dahlberg G. Statistical methods for medical and biological students. New York: Interscience Publications, 1940.
De Smit A, Dermaut L. Soft tissue profile preference. Am J Orthod Dentofacial Orthop 1986;67–73.
Fabré M, Mossaz C, Christou P, Kiliaridis S. Orthodontists’ and lay-persons’ aesthetic assessment of Class III subjects referred for orthognathic surgery. Eur J Orthod 2009;31:443–8.
Farkas LG. Anthropometry of the head and face. 2nd ed. New York: Raven Press, 1994.
Ferrario VF, Ciusa V, Tartaglia GM. The effect of sex and age on facial asymmetry in healthy subjects: a cross-sectional study from adolescence to mid-adulthood. J Oral Maxillofac Surg 2001;59:382–8.
Franchi L, Baccetti T, Tollaro I. Predictive variables for the outcome of early functional treatment of Class III malocclusion. Am J Orthod Dentofacial Orthop 1997;11:80–6.
Giddon DB. Orthodontic applications of psychological and perceptual studies of facial esthetics. Semin Orthod 1995;1:82–93.
Gruber M, Häusler G. Simple, robust and accurate phase-measuring triangulation. Optik 1992;89:118–22.
Hasund A. Klinische Kephalometrie für die Bergentechnik. Bergen: Norwegen 1976.
Holberg C. Erfassung von Gesichtsoberflächen durch ein lichtcodiertes Triangulationsverfahren. Med Diss, Universität Tübingen, 2002.
Holdaway RA. A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthod 1983;84:1–28.
Houston WJB. The analysis of error in orthodontic measurements. Am J Orthod 1983;83:382–90.
Jäger A, Zittlau O, Luhr HG. Zur differentialdiagnostischen Wertigkeit von skelettalen, dentalen und Weichteilanalysen bei der Planung der kieferorthopädisch-kieferchirurgischen Therapie. Fortschr Kieferorthop 1994;55:269–78.
Johnston DJ, Hunt O, Johnson CD, et al. The influence of lower face vertical proportion on facial attractiveness. Eur J Orthod. 2005;27:349–54.
Karbacher S. Rekonstruktion und Modellierung von Flächen aus Tiefenbildern. Diss, Friedrich-Alexander-Universität Erlangen-Nürnberg, 1997.
Keeling SD, Riolo ML, Martin RE, Ten Have TR. A multivariate approach to analyzing the relation between occlusion and craniofacial morphology. Am J Orthod Dentofacial Orthop. 1997;11:80–6.
Kiyak HA, Hohl T, Sherrick P, et al. Sex differences in motives for and outcomes of orthognathic surgery. J Or Surg 1981;39:757–64.
Knight H, Keith O. Ranking facial attractiveness. Eur J Orthod 2005;27:340–8.
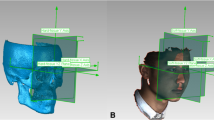
Kochel J, Meyer-Marcotty P, Strnad F, et al. 3D-soft tissue analysis — Part I: Sagittal parameters. J Orofac Orthop 2010;71:40–52.
Kowalski CJ, Nasjleti CE, Walker GF. Differential diagnosis of adult male black and white populations. Angle Orthod 1974;44:346–50.
Kowalski CJ, Nasjleti CE, Walker GF. Dentofacial variations within and between four groups of adult American males. Angle Orthod 1975;45:146–51.
Laufer D, Glick D, Gutman D, Sharon A. Patient motivation and response to surgical correction of prognathism. Oral Surg Oral Med Oral Path 1976;41:309–13.
Legan HL, Burstone CJ. Soft tissue cephalometric analysis for orthognathic surgery. J Oral Surg 1980;38:744–51.
Lines PA, Lines RR, Lines CA. Profilemetrics and facial esthetics. Am J Orthod 1978;73:648–57.
Nkenke E, Vairaktaris E, Kramer M, et al. Three-dimensional analysis of changes of the malar-midfacial region after LeFort I osteotomy and maxillary advancement. Oral Maxillofac Surg 2008;12:5–12.
O'Grady KF, Antonyshyn OM. Facial asymmetry: three-dimensional analysis using laser surface scanning. Plast Reconstr Surg 1999;104:928–37.
Peck H, Peck S. A concept of facial esthetics. Angle Orthod 1970;40:284–318.
Plooij JM, Swennen GR, Rangel FA, et al. Evaluation of reproducibility and reliability of 3D soft tissue analysis using 3D stereophotogrammetry. Int J Oral Maxillofac Surg 2009;38:267–73.
Powel N, Humphreys B. Proportions of the aesthetic face. In: Smith JD, ed. New York: Thieme-Stratten Inc, 1984:72.
Rakosi T, Jonas I. Kieferorthopädie, Diagnostik. Farbatlanten der Zahnmedizin. Bd. 8. Stuttgart: Thieme, 1989.
Rakosi T. Atlas und Anleitung zur praktischen Fernröntgenanalyse. München: Hanser Fachbuch, 1988.
Ricketts RM, Bench RW, Gugino CF, et al. Bioprogressive therapy. Book I. Denver, CO: Rocky Mountain Orthodontics, 1979.
Riolo ML, Moyers RE, TenHave TR, Mayers CA. Facial soft tissue changes during adolescence. In: Carlson DS, Ribbens KA, eds. Craniofacial growth during adolescence. Monograph 20, Craniofacial Growth Series. Ann Arbor, MI: Center for Human Growth and Development; University of Michigan, 1987.
Sandler PJ. Reproducibility of cephalometric measurements. Br J Orthod 1988;15:105–10.
Schopf P. Zur Prognose des vertikalen Wachstumstyps. Fortschr Kieferorthop 1982;43:271–81.
Staudt C B, Kiliaridis S. A nonradiographic approach to detect Class III skeletal discrepancies. Am J Orthod Dentofacial Orthop 2009;136:52–8.
Stoner MM. A photometric analysis of the facial profile. A method of assessing facial change induced by orthodontic treatment. Am J Orthod 1955;41:453–69.
Subtelny JD. A longitudinal study of soft tissue facial structures and their profile characteristics defined in relation to underlying skeletal structures. Am J Orthod 1959;45:453–507.
Swennen GRJ, Schutyser F, Barth E, et al. A new method of 3-D cephalometers Part I: The anatomic cartesian 3-D reference system. J Craniofac Surg 2006;17:314–25.
Swennen GRJ, Schutyser F, Lemaitre A, et al. Accuracy and reliability of 3-D CT versus 3-D stereo photogrammetry based facial soft tissue analysis. Int J Oral Maxillofac Surg 2005;34:73.
Tahmina K, Tanaka E, Tanne K. Cranifacial morphology in orthodontically treated patients of Class III malocclusion with stable and unstable treatment outcomes. Am J Orthod Dentfac Orthop 2000;117:681–90.
Toma AM, Zhurov A, Playle R, et al. Reproducibility of facial soft tissue landmarks on 3D laser scanned facial images. Orthod Craniofac Res 2009;12:33–42.
Veit K. Verringerung systematischer Messfehler bei der phasenmessenden Triangulation. Med Diss, Friedrich-Alexander-Universität Erlangen-Nürnberg, 2003.
Wictorin L, Hillerström K, Sörensen S. Biological and psycho-social factors in patients with malformation of the jaws. I. A study of 95 patients prior to treatment. Scand J Plast Reconstr Surg 1969;3:138–43.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kochel, J., Meyer-Marcotty, P., Kochel, M. et al. 3D Soft Tissue Analysis – Part 2: Vertical Parameters. J Orofac Orthop 71, 207–220 (2010). https://doi.org/10.1007/s00056-010-9943-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-010-9943-9