Abstract
Background
To evaluate a new procedure in daily clinical practice, it might not be sufficient to rely exclusively on the findings of randomized clinical trials (RCTs). This is the first systematic review providing a synthesis of the most important RCTs and relevant retrospective cohort studies on short- and long-term outcomes of laparoscopic surgery in colon cancer patients.
Materials and methods
In a literature search, more than 1800 relevant publications on the topic were identified. Relevant RCTs and representative high-quality retrospective studies were selected based on the widely accepted Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria. Finally, 9 RCTs and 14 retrospective cohort studies were included.
Results
Laparoscopic surgery for colon cancer is associated with a slightly longer duration of surgery, but a variety of studies show an association with a lower rate of postoperative complications and a shorter duration of hospital stay. Particularly in older patients with more frequent comorbidities, laparoscopy seems to contribute to decreasing postoperative mortality. Concerning long-term oncologic outcomes, the laparoscopic and open techniques were shown to be at least equivalent.
Conclusion
The findings of the existing relevant RCTs on laparoscopic surgery for colon cancer are mostly confirmed by representative retrospective cohort studies based on real-world data; therefore, its further implementation into clinical practice can be recommended.
Zusammenfassung
Hintergrund
Um die Eignung eines neuen Behandlungsverfahrens im klinischen Alltag zu überprüfen, sollte man sich nicht ausschließlich auf die Ergebnisse randomisierter Studien (RCTs) verlassen. Dies ist die erste Übersichtsarbeit zum Thema laparoskopische Tumorresektion beim Kolonkarzinom, welche neben RCTs repräsentative retrospektive Kohortenstudien zu Kurz- und Langzeitergebnissen berücksichtigt.
Methoden
In einer Literaturrecherche wurden über 1800 relevante Publikationen identifiziert. Eine Selektion der relevanten pro- und retrospektiven Studien zum Thema Laparoskopie beim Kolonkarzinom fand auf Grundlage der STROBE-Kriterien statt. Schließlich wurden 9 RCTs und 14 retrospektive Studien eingeschlossen.
Ergebnisse
Laparoskopische Chirurgie beim Kolonkarzinom ist zwar mit einer etwas längeren Operationsdauer, jedoch auch mit einer niedrigeren postoperativen Komplikationsrate und einer kürzeren Krankenhausverweildauer assoziiert. Vor allem ältere Patienten mit mehr Komorbiditäten scheinen von einer niedrigeren postoperativen Mortalität zu profitieren. Was das onkologische Langzeitergebnis betrifft, ist das laparoskopische dem offenen Verfahren mindestens ebenbürtig.
Schlussfolgerung
Die Ergebnisse der existierenden relevanten RCTs zur Laparoskopie beim Kolonkarzinom werden größtenteils von repräsentativen retrospektiven Kohortenstudien aus dem Klinikalltag bestätigt. Daher kann die weitere Implementierung der Laparoskopie in den Klinikalltag empfohlen werden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Worldwide, laparoscopic surgery is becoming the new standard for curative resection of colon cancer. In recent decades, many studies were performed to analyze its advantages and disadvantages and, above all, its oncologic safety compared to the open technique.
Today, there exists quite extensive but also very heterogenous evidence on laparoscopic colorectal tumor surgery. Many publications are dedicated exclusively to postoperative endpoints such as duration of surgery, resection margins, or short-term mortality. Others report long-term outcomes including overall survival or recurrence rates. The study designs range from small case studies to large randomized controlled trials (RCTs), which are regarded as the gold standard in medical research. However, due to strict in- and exclusion criteria, RCTs often reflect the situation in a selected patient collective only; therefore, it might not be sufficient to rely exclusively on the findings of RCTs. In contrast to this, large population-based retrospective multicenter or registry-based studies use “real-word data”, offering insight into the efficiency in daily clinical practice. This renders them an indispensable part of the clinical evaluation process. To account for the lack of randomization, such studies employ adequate statistical methods like multivariable regression analysis, which needs to be considered when interpreting the corresponding outcomes. This paper is the first systematic review on the topic providing a synthesis of the most important RCTs and relevant retrospective trials, drawing a holistic picture of laparoscopic surgery in colon cancer patients.
Materials and methods
To identify relevant literature on the topic, PubMed and Cochrane Central were searched [1, 2]. For this purpose, three fields of interest were defined:
-
Colorectal cancer: the corresponding MeSH term is “Colorectal Neoplasms” Moreover, a free-text search with the following (truncated) terms was performed: “colorectal cancer*”, “colorectal carcinoma*”, “colorectal tumor*”, “colorectal tumour*”, and “colorectal neoplasm*”. Local differences in spelling (e.g., “tumour” instead of “tumor”) were considered. To identify only relevant publications, the search was restricted to publications tagged with the subheading “surgery”. Moreover, the free-text search was limited to the title. In total, 91,597 hits were reached.
-
Laparoscopy: the corresponding MeSH term is “Laparoscopy”. Additionally, a free-text search with the truncated term “laparoscop*” in all available fields provided by PubMed was performed, leading to identification of 102,255 relevant publications.
-
Open surgery: the corresponding MeSH term is “Laparotomy”. To also identify relevant literature not tagged by this MeSH term, a free-text search with the truncated terms “laparotom*”, “celiotom*”, and “coeliotom*” in all fields was performed. Thus, 424,689 publications were identified.
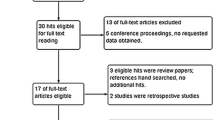
In total more than 1800 relevant publications address all three aspects simultaneously, of which more than 1600 were written in English or German (Fig. 1). To identify representative high-quality retrospective studies, a selection process based on the widely accepted Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)-criteria [3] was performed. Special focus was placed on the following aspects:
-
Study design: How was data acquisition performed? How many patients were included? What were the exact in- and exclusion criteria? Is the whole exclusion process transparent for the reader? Is the study collective representative for the population/setting it was gathered from?
-
Study variables: Is the set of predictor and outcome variables meaningful? Are the variable definitions clear and transparent?
-
Methods: Were adequate statistical methods applied to account for the lack of randomization? Are all analyses clearly described?
Finally, 14 retrospective studies met the standards for inclusion in the present literature review. A similar workflow was applied to identify 9 relevant RCTs on the topic. Table 1 and 2 give an overview of the included literature.
Endpoints in the focus of the current review were intraoperative blood loss and duration of surgery, lymphadenectomy and resection margins, postoperative morbidity and mortality, long-term overall survival, and tumor recurrence.
Results
Laparoscopy rate
According to the Arbeitsgemeinschaft Deutscher Tumorzentren (ADT; Working Group of German Tumor Centers), the share of laparoscopic resection procedures in Germany has increased from 3.4% in 2000 to 31.0% in 2018 (Fig. 2). These figures are based on reports from 30 clinical cancer registries representing approximately one quarter of all colon carcinoma cases in Germany based on data presented at the National Quality Conference of the German Cancer Congress 2020 [4].
Intraoperative blood loss and duration of surgery
In all included RCTs, the mean intraoperative blood loss was significantly lower after laparoscopic surgery. The reported mean values range between 46 and 105 ml compared to 127 to 193 ml after open surgery [5,6,7]. Similar results can be observed in the population-based trial of McKay et al. from Australia [8], which reports a significantly lower average need for intraoperative blood transfusions of 0.4 vs. 0.7 per patient in favor of the laparoscopic procedure.
Laparoscopic tumor resections take longer than those performed in the conventional technique. The mean duration of surgery in the included RCTs ranged between 142 and 213 min [5,6,7, 9, 10]. Again, these observations are supported by the findings of McKay et al. [8]. According to their retrospective study, laparoscopic procedures take on average 24 min longer (175 min vs. 151 min; p < 0.001).
Lymphadenectomy and resection margins
A sufficient number of removed and histologically evaluated lymph nodes is regarded as a positive quality indicator of successful tumor removal. For example, the German treatment guideline on colorectal carcinoma recommends a minimum count of 12 nodes, although there is no international consensus concerning the exact number [11]. Moreover, there exists no generally recognized standard for the pathological examination of lymph nodes, which has to be considered when comparing and analyzing results of different studies. A systematic review from Kuhry et al. [12] published by the Cochrane Collaboration in 2008 pools the results of five RCTs reporting on lymphadenectomy [5, 7, 13,14,15]. Compared to the open approach, the number of harvested lymph nodes after laparoscopic procedures is smaller by 1 lymph node (confidence interval, CI: [−1.65–−0.35]). The results of the retrospective trials on this endpoint are comparable (Kolfschoten et al. [16]: more than 10 harvested lymph nodes: odds ratio, OR: 0.87, CI: 0.76–1.00, reference: open; McKay et al. [5]: mean count of harvested lymph nodes per patient: laparoscopic intention-to-treat, itt: 17.4 vs. open: 18.2, p = 0.38; Völkel et al. [17]: more than 12 harvested lymph nodes: laparoscopic itt: 88.9% vs. open: 92.2%, p = 0.028).
Tumor-free resection margins are the primary goal of each tumor resection. In 2005, the randomized CLASICC trial reported a higher share of tumor-positive margins after laparoscopic procedures [9]. This outcome misses the significance level considerably (p = 0.45), but caused an extensive discussion on the topic anyway. Therefore, the real-world data publications are even more interesting. A population-based survey from the US by Zheng et al. [18] observed a significantly lower share of tumor-positive resection margins after laparoscopic procedures (laparoscopic 3.4% vs. open 5.5%; p < 0.001), although this advantage is mitigated after risk adjustment and propensity matching. In the study of Kolfschoten et al. [16] the advantage for the laparoscopic procedure remains constant even after risk adjustment (OR: 0.68, CI: 0.48–0.98, reference: open). According to a registry-based trial from southern Germany published in 2018, positive resection margins are less frequently associated with laparoscopic procedures [17]; however, due to a low absolute count of postoperatively tumor-positive patients, significance testing was not possible. Contrary to this, the Australian registry study of McKay et al. [8] reports a (non-significantly) smaller mean distance between tumor border and resection margin in laparoscopic patients.
Postoperative morbidity and mortality
Various trials have shown that laparoscopic patients suffer less from postoperative pain and wound infection, leading to faster convalescence and a shorter hospital stay [16, 19,20,21,22,23]. This was confirmed by a meta-analysis from Schwenk et al. [24] and a systematic review from Otani et al. [25].
There are different outcome measures to quantify postoperative mortality: depending on the trial, in-hospital-, 30-day, or 90-day mortality were evaluated. According to the randomized CLASICC trial, there is no significant difference between laparoscopy and laparotomy concerning in-hospital mortality (Table 3), but most registry-based studies show a lower risk of postoperative mortality in laparoscopic patients (OR after multivariable risk adjustment ranges between 0.49 and 0.63, Table 3; [5, 13,14,15,16,17,18,19,20]).
The trials of Panis et al. [26] and Völkel et al. [27] point towards an age- and partial comorbidity-dependent gradient: older patients and patients with a somewhat higher level of comorbidity benefit more from the laparoscopic approach in terms of postoperative mortality. Based on US registry data, Fox et al. [23] showed a significant association between a higher laparoscopy rate in a hospital and a shorter duration of stay and lower postoperative morbidity. However, postoperative mortality seems to be independent of this. However, it must be acknowledged that in all the studies it was adjusted for many but not all important confounders. Items such as intraabdominal adhesions or lipodistribution are often poorly documented and, thus, usually cannot be included in the statistical analyses.
In summary, it seems safe to postulate a positive influence of laparoscopy on postoperative morbidity. An association with lower postoperative mortality is also very likely, particularly in old and comorbid patients. Other aspects of perioperative management including establishment of an ostomy, limited resection, and failure-to-rescue situations supposedly play an even more important role in this context.
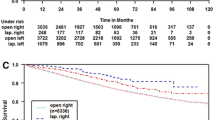
Long-term overall survival
“Mortality turned out to be equal in patients who had undergone laparoscopic surgery as compared to patients who underwent open surgery” (OR: 0.82, CI: 0.62–1.09, reference: open). This is the conclusion of the systematic Cochrane review by Kuhry et al. [12], which incorporated four RCTs in the corresponding meta-analysis on long-term survival after laparoscopic and open colon carcinoma resection [7, 13, 28, 29]. Concordantly, the renowned randomized COLOR trial reports almost identical 5‑year survival rates after laparoscopic (73.8%; standard deviation, sd: 69.7–77.9%) and open (74.2%, sd: 70.1–78.2%) resection [30]. After a very long observation time of 10 years, the situation has not changed much: “Laparoscopic surgery for non-metastatic colon cancer is associated with similar rates of disease-free survival, overall survival and recurrences as open surgery” [31].
High-quality retrospective studies on long-term survival are scarce. Based on Norwegian cancer registry data, Stormark et al. did not find significant differences between the two surgical techniques concerning overall survival in Union for International Cancer Control (UICC) stage I–III patients (relative survival after 5 years: laparoscopic 77.7% vs. open: 80.6%, p = 0.54) [32]. Sammour et al. used Australian registry data and observed superior 5‑year survival rates after laparoscopic resection (laparoscopic itt: 75.9% vs. open: 69.2%, p = 0.015), although the significance level was no longer reached after risk adjustment [21]. Kube et al. analyzed data of the An-Institut Magdeburg and also saw a significant advantage for the laparoscopic procedure (5-year overall survival: laparoscopic as treated: 82.8% vs. open: 66.9%, p = 0.005), although it must be noted that participation in this retrospective cohort study performed 15 years ago in Germany was voluntary [22].
A more recent study of Benz et al. [33] analyzes cancer registry data from the Arbeitsgemeinschaft Deutscher Tumorzentren (ADT; Working Group of German Tumor Centers), which gathers patient-, diagnosis-, and treatment-related medical records in approximately 30% of German tumor patients on a legal basis. It stratified the patients into four groups: “laparoscopic left”, “laparoscopic right”, “open left”, and “open right”. According to this study, tumor location does not serve as an effect modifier for the surgical approach. In both the Kaplan–Meier and the multivariable analyses, there was a significant survival benefit for the laparoscopic technique, regardless of tumor location and UICC stage (only stages I–III were included in the analysis).
These findings are in contrast to an earlier analysis of the National Cancer Database (NCDB) registry by Bilimoria et al. [34], who did not observe a positive influence of the laparoscopic approach on overall survival. In the study of Völkel et al., the advantage for the laparoscopic approach was also restricted to low-risk situations (T1–3, N0), while high-risk patients (T4 or N1) did not benefit significantly from the minimally invasive technique [35].
Taking all of the presented evidence (Table 4) into account, the laparoscopic and the open approach seem to be equivalent in terms of overall survival. There might perhaps be a slight advantage for the laparoscopic approach. Future studies on this topic should focus on the standardization of certain surgical standards such as the extent of lymphadenectomy, since this has been neglected by virtually all existing pro- and retrospective trials.
Tumor recurrence
Colorectal tumor resection aims to maximize tumor-free survival. According to the Cochrane meta-analysis by Kuhry et al., laparoscopy and laparotomy do not differ significantly in terms of local and distant metastasis rates [12].
Since local recurrence events are not common in colon cancer patients, most studies simply report disease-free survival. For example, the COLOR study reports a disease-free survival rate of 66.5% (sd 62.2–70.7) in patients with laparoscopic and 67.9% (sd 63.6–72.2) in patients with open resection [30]. Despite the randomized study design, it was decided to additionally perform multivariable Cox regression to adjust for age, sex, and UICC stage, resulting in a hazard ratio (HR) of 0.92 (CI 0.74–1.15, reference: open) in favor of the laparoscopic approach. This figure is almost perfectly matched by the cancer registry study of Völkel et al.: HR 0.94 (CI 0.74–1.19, reference: open). However, in the older study by Kube et al., there was no significant difference between the surgical approaches in terms of disease-free survival ([35]; Table 5).
Conclusion
Laparoscopic surgery for colon carcinoma is associated with a slightly longer duration of surgery, but a variety of studies show that it is also associated with a lower rate of postoperative complications and a shorter duration of hospital stay. Particularly in older patients with more comorbidities, laparoscopy seems to contribute to decreasing postoperative mortality. Concerning long-term oncologic outcomes, the laparoscopic and the open techniques were shown to be at least equivalent with regards to overall and recurrence-free survival. Depending on the characteristics of the observed patient collective, laparoscopy might be slightly superior if the same surgical standards are applied.
References
National Center for Biotechnology Information (2020) U.S. National library of medicine. https://www.ncbi.nlm.nih.gov/pubmed/. Accessed 3 Apr 2020
Cochrane Central Register of Controlled Trials (CENTRAL) (2020) Cochrane central register of controlled trials (CENTRAL). https://www.cochranelibrary.com/central/about-central. Accessed 3 Apr 2020
von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Arbeitsgemeinschaft Deutscher Tumorzentren e. V. ADT – für Qualitätssicherung in der Onkologie (2019) Arbeitsgemeinschaft Deutscher Tumorzentren e. V. ADT – für Qualitätssicherung in der Onkologie. https://www.tumorzentren.de/. Accessed 12 Feb 2019
Braga M, Frasson M, Vignali A et al (2005) Laparoscopic vs. open colectomy in cancer patients: long-term complications, quality of life, and survival. Dis Colon Rectum 48:2217–2223. https://doi.org/10.1007/s10350-005-0185-7
Veldkamp R, Kuhry E, Hop WCJ et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484. https://doi.org/10.1016/S1470-2045(05)70221-7
Lacy AM, Garcia-Valdecasas JC, Delgado S et al (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229. https://doi.org/10.1016/S0140-6736(02)09290-5
McKay GD, Morgan MJ, Wong S‑KC et al (2012) Improved short-term outcomes of laparoscopic versus open resection for colon and rectal cancer in an area health service: a multicenter study. Dis Colon Rectum 55:42–50. https://doi.org/10.1097/DCR.0b013e318239341f
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726. https://doi.org/10.1016/S0140-6736(05)66545-2
Fleshman JW, Nelson H, Peters WR et al (1996) Early results of laparoscopic surgery for colorectal cancer. Retrospective analysis of 372 patients treated by Clinical Outcomes of Surgical Therapy (COST) Study Group. Dis Colon Rectum 39:8
Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF): S3-Leitlinie Kolorektales Karzinom, Langversion 1.1, 2014, AWMF Registrierungsnummer: 021-007OL, http://leitlinienprogramm-onkologie.de/Leitlinien.7.0.html [Stand: 08.2014]
Kuhry E, Schwenk WF, Gaupset R et al (2008) Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003432.pub2
Kaiser AM, Kang J‑C, Chan LS et al (2004) Laparoscopic-assisted vs. open colectomy for colon cancer: a prospective randomized trial. J Laparoendosc Adv Surg Tech A 14:329–334. https://doi.org/10.1089/lap.2004.14.329
Leung KL, Kwok SPY, Lam SCW et al (2004) Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet 363:1187–1192. https://doi.org/10.1016/S0140-6736(04)15947-3
Liang J-T, Huang K-C, Lai H-S et al. (2007) Oncologic results of laparoscopic versus conventional open surgery for stage II or III left-sided colon cancers: a randomized controlled trial. Ann Surg Oncol 14(1):109–117. https://doi.org/10.1245/s10434-006-9135-4
Kolfschoten NE, van Leersum NJ, Gooiker GA et al (2013) Successful and safe introduction of laparoscopic colorectal cancer surgery in Dutch hospitals. Ann Surg 257:916–921. https://doi.org/10.1097/SLA.0b013e31825d0f37
Völkel V (2018) Langzeitüberleben nach laparoskopischer und offener Resektion des Kolon-Karzinoms – eine bevölkerungsbezogene Analyse. https://epub.uni-regensburg.de/37757/. Accessed 17 June 2019
Zheng Z, Jemal A, Lin CC et al (2015) Comparative effectiveness of laparoscopy vs open colectomy among nonmetastatic colon cancer patients: an analysis using the National Cancer Data Base. J Natl Cancer Inst. https://doi.org/10.1093/jnci/dju491
Taylor EF, Thomas JD, Whitehouse LE et al (2013) Population-based study of laparoscopic colorectal cancer surgery 2006–2008. Br J Surg 100:553–560. https://doi.org/10.1002/bjs.9023
Steele SR, Brown TA, Rush RM et al (2008) Laparoscopic vs open colectomy for colon cancer: results from a large nationwide population-based analysis. J Gastrointest Surg 12:583–591. https://doi.org/10.1007/s11605-007-0286-9
Sammour T, Jones IT, Gibbs P et al (2015) Comparing oncological outcomes of laparoscopic versus open surgery for colon cancer: analysis of a large prospective clinical database. J Surg Oncol 111:891–898. https://doi.org/10.1002/jso.23893
Kube R, Ptok H, Steinert R et al (2008) Clinical value of laparoscopic surgery for colon cancer (Stellenwert der laparoskopischen Chirurgie des Kolonkarzinoms in der klinischen Routine). Chirurg 79:1145–1150. https://doi.org/10.1007/s00104-008-1585-8
Fox JP, Desai MM, Krumholz HM et al (2012) Hospital-level outcomes associated with laparoscopic colectomy for cancer in the minimally invasive era. J Gastrointest Surg 16:2112–2119. https://doi.org/10.1007/s11605-012-2018-z
Schwenk W, Neudecker J, Haase O (2015) Evidenzlage der laparoskopischen Chirurgie beim Kolonkarzinom. coloproctology 37:381–390. https://doi.org/10.1007/s00053-015-0026-7
Otani T, Otani T, FIsohata N et al (2016) An evidence-based medicine approach to the laparoscopic treatment of colorectal cancer. Fukushima J Med Sci. https://doi.org/10.5387/fms.2016-4
Panis Y, Maggiori L, Caranhac G et al (2011) Mortality after colorectal cancer surgery: a French survey of more than 84,000 patients. Ann Surg 254:738. https://doi.org/10.1097/SLA.0b013e31823604ac
Völkel V, Draeger T, Schnitzbauer V et al (2019) Surgical treatment of rectal cancer patients aged 80 years and older—a German nationwide analysis comparing short- and long-term survival after laparoscopic and open tumor resection. Eur J Surg Oncol. https://doi.org/10.1016/j.ejso.2019.05.005
(2004) Laparoscopically assisted colectomy is as safe and effective as open colectomy in people with colon cancer Abstracted from: Nelson H, Sargent D, Wieand HS, et al; for the Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004; 350: 2050–2059. Cancer Treat Rev 30: 707–709. https://doi.org/10.1016/j.ctrv.2004.09.001
Curet MJ, Putrakul K, Pitcher DE et al (2000) Laparoscopically assisted colon resection for colon carcinoma: perioperative results and long-term outcome. Surg Endosc 14:1062–1066
Buunen M, Veldkamp R, Hop WCJ et al (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52. https://doi.org/10.1016/S1470-2045(08)70310-3
FDeijen CL, Deijen CL, FVasmel JE et al (2016) Ten-year outcomes of a randomised trial of laparoscopic versus open surgery for colon cancer. Surg Endosc. https://doi.org/10.1007/s00464-016-5270-6
Stormark K, Stormark K, FSoreide K et al (2016) Nationwide implementation of laparoscopic surgery for colon cancer: short-term outcomes and long-term survival in a population-based cohort. Surg Endosc. https://doi.org/10.1007/s00464-016-4819-8
Benz S, Barlag H, Gerken M et al (2016) Laparoscopic surgery in patients with colon cancer: a population-based analysis. Surg Endosc. https://doi.org/10.1007/s00464-016-5266-2
Bilimoria KY, Bentrem DJ, Nelson H et al (2008) Use and outcomes of laparoscopic-assisted colectomy for cancer in the United States. Arch Surg 143:832. https://doi.org/10.1001/archsurg.143.9.832
Völkel V, Draeger T, Gerken M et al (2018) Long-term oncologic outcomes after laparoscopic vs. open colon cancer resection: a high-quality population-based analysis in a southern German district. Surg Endosc. https://doi.org/10.1007/s00464-018-6158-4
Acknowledgements
The authors thank all participating registries (Augsburg, Berlin, Dresden, Stuttgart OSP, Zwickau, Chemnitz, Dessau, Koblenz, Halle, Leipzig, Bayreuth, Göppingen OSP, Erfurt, Westfalen-Lippe, Magdeburg, Erlangen-Nürnberg, Gera, Nordhausen, Jena, Brandenburg, Suhl, Regensburg, Ulm-CCC, Reutlingen, Ravensburg, Wiesbaden, Hamburg, Schleswig-Holstein, Hanau Klinikum, Hannover, and Mecklenburg-Vorpommern) for their cooperation.
Funding
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
V. Völkel, T. Draeger, M. Gerken, M. Klinkhammer-Schalke, S. Benz, and A. Fürst declare that they have no competing interests.
This publication does not contain any experiments with patients or animals.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Völkel, V., Draeger, T., Gerken, M. et al. Laparoscopic surgery for colon cancer. coloproctology 42, 413–420 (2020). https://doi.org/10.1007/s00053-020-00481-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00053-020-00481-6
Keywords
- Minimally invasive surgical procedures
- Registries
- Cohort studies
- Randomized controlled trial
- Evidence-based medicine