Abstract
A series of imines 5-amino-1,3,4-thiadiazol-2-[(N-substituted benzyol)]sulphonamide derivatives were synthesized from various aromatic aldehydes and substituted with benzoyl acetazolamides under different reaction conditions and were evaluated for their antioxidant and free radical scavenging, antimitotic activity by Allium cepa meristem root model and cytotoxicity activity against HEK 293 (human epidermal kidney cell line), BT474 (breast cancer cell line) and NCI-H226 (lung cancer cell line) by MTT assay. Some of the synthesized compounds showed moderately potent cytotoxicity compared to indisulam.
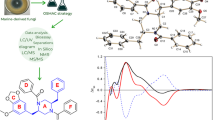
Graphical abstract
A series of imines 5-amino-1,3,4-thiadiazol-2-[(N-substituted benzyol)]sulphonamide derivatives (9a–j); 5-amino-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamide (4a–g); 5-(4-acetamido phenyl sulphonamido)-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamide (6a–g); and 5-(4-amino phenyl sulphonamido)-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamide (7a–g) were synthesized from acetazolamide and were investigated for the in vitro anticancer by MTT assay, free radical scavenging and antimitotic activity by Allium cepa root meristem model. Experimental observations indicate that synthesized compounds were moderately potent anticancer agents.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rapid spread of cancer has sparked an intense worldwide search for new compounds, which may be used in designing anticancer drugs. The search of more effective anticancer agent has focused to a large extent on the design of molecules capable of recognizing and binding to target DNA base sequences. Development of anticancer drugs with fewer or no side effects is important for the treatment for cancer. The search for such potential anticancer drugs has led to the discovery of synthetic small molecules with anti-carcinogenic activity and limited harmful side effects particularly with respect to the immune system. Research in this area is expanding rapidly, and some promising leads have emerged. Heterocyclic moieties can be found in a large number of compounds, which display biological activity. The biological activity of the compounds is mainly dependent on their molecular structures (Salimon et al., 2010). A vast number of 1,3,4-thiadiazoles have been reported as potential pharmacologically active compounds with antimicrobial (Patil and Biradar, 2001; Zamani et al., 2004; Sharma et al., 2006), antiviral (Pandey et al., 2004), antitubercular (Oruc et al., 2004; Desai et al., 1984), anticonvulsant (Shrivastava et al., 1999; Kumar et al., 2003; Gupta et al., 2008; Stillings et al., 1986; Jatav et al., 2008), CNS depressant (Jatav et al., 2008), hypoglycaemic (Hanna et al., 1995; Pattan et al., 2009), anti-inflammatory (Sharma et al., 2008; Varandas et al., 2005) and anticancer (Noolvi et al., 2011; Kumar et al., 2010) properties. At the same time, the 1,3,4-thiadiazole fragment appears in a number of clinically used drugs such as acetazolamide; methazolamide; butazolamide (diuretic); sulfamethiazole (antibacterial); cefazolin, cefazedone (antibiotic); atibeprone (anti-depressant); glybuthiazole, glybuzole (antidiabetic); and tebuthiuron (insecticide) (Wilson and Gisvold, 1991; Abrahum, 2003; Supran et al., 2003).
Schiff bases, contain an azomethine group, derived from aromatic aldehydes and aromatic amines, have potential for both chemical and biological activities (Dhar and Taploo, 1982; Pacheco et al., 1970). This is due to the presence of carbon–nitrogen double bond having potential receptor-binding ability. Schiff bases are also one of the intensively investigated classes of aromatic and heteroaromatic compounds. This class of compounds showed a variety of applications ranging from anticancer (Sharma et al., 1998; Kuzmin et al., 2005), antibacterial (More et al., 2002; Vaghasiya et al., 2004), diuretic (Supran et al., 1996), antifungal (Manrao et al., 1982, 1995, 2001) and antiparasitic activity (Rathelot et al., 2002). They have also medicinal importance and are used in drug design due to their activity against a wide range of organisms (Khan et al., 2002; Verma et al., 2004). Schiff bases are used as substrates in the preparation of a number of industrially and biologically active compounds via closure, cycloaddition and replacement reactions (Taggi et al., 2002).
Sulphonamides are a significant class of compounds in medicinal and pharmaceutical chemistry with several biological applications (Tilles, 2001; Slatore and Tilles, 2004; Brackett et al., 2004; Harrison, 1994; Eroglu, 2008).
There are many connections between carbonic anhydrase (CA) and cancer (Supuran, 2008; Supuran and Scozzafava, 2000; Pastorek et al., 1994; Pastorekova et al., 1997; Chegwidden et al., 2001). It is well known that some CA isozymes are predominantly found in cancer cells and are lacking from their normal counterparts (Pastorek et al., 1994; Pastorekova et al., 1997; Chegwidden et al., 2001), and these are two transmembrane isozymes CA IX and CA XII. Isozyme CA XIV was the last one to be discovered among the 15 CA isoforms of this widespread metalloprotein known up to now in human (Supuran et al., 2004). Kaunisto et al. (2002) and Parkkila et al., (2001, 2002) revealed CA XIV distribution in the human body as well as potential physiological/pathological roles. It has been observed that hCA XIV is highly abundant in the brain, kidney, colon, small intestine, urinary bladder, liver and spinal cord (Kaunisto et al., 2002; Parkkila et al., 2001, 2002; Fujikawa-Adachi et al., 1999; Ashida et al., 2002). Similar to isozymes CA IX and CA XII, CA XIV is a transmembrane protein with the active site oriented extracellularly, but unlike the first two proteins, isozyme XIV is not associated with tumour cells (Pastorek et al., 1994; Kaunisto et al., 2002; Parkkila et al., 2001, 2002; Ashida et al., 2002). Membrane-associated human carbonic anhydrase (hCAs) isozymes IX, XII and XIV (Fujikawa-Adachi et al., 1999; Tureci et al., 1998) like other hCAs regulate pH and carbon dioxide (CO2)–bicarbonate anion (HCO3) homoeostasis, through the catalysis of the reversible hydration of CO2 to give HCO3 and proton (Hþ). The expression level of isozymes hCA IX and XII is elevated in response to hypoxia, and research on the involvement of these isozymes in cancer has progressed considerably in recent years, particularly for hCA IX (Tureci et al., 1998; Wykoff et al., 2000; Parkkila et al., 2000; Svastova et al., 2004; Cecchi et al., 2005). It has been confirmed that hCA IX is a high-activity CA isozyme responsible for the extracellular acidification (pHe) of the tumour microenvironment. Multiple downstream effects of this reduced pHe are associated with tumour progression and poor prognosis (Parkkila et al., 2000; Svastova et al., 2004). Aromatic sulphonamide compounds have been shown to reverse the effect of tumour acidification, to inhibit the growth of cancer cells and to suppress tumour invasion mediated by these CAs (Tureci et al., 1998; Wykoff et al., 2000; Parkkila et al., 2000; Svastova et al., 2004; Cecchi et al., 2005; Brzozowski et al., 2010).
Thus, the data from these many physiological studies appear to have identified a CA-mediated, hypoxic tumour-specific pathway. This provides firm grounds for exploring the effects of this class of compounds as a novel approach to discriminate between healthy cells and cancerous cells, specifically targeting hypoxic tissues, an attractive attribute that is lacking in many existing cancer therapies (Minchinton and Tannock 2006; Kamb, 2005).
These findings prompted us to the synthesis of 5-arylidine amino-1,3,4-thiadiazol-2-[(N-benzoyl)]sulphonamide derivatives (9a–j) from carbonic anhydrase inhibitor drug acetazolamide. The synthesized compounds reported previously (Chhajed et al., 2007, 2013), such as 5-amino-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamide (4a–g), 5-(4-acetamido phenyl sulphonamido)-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamide (6a–g), and 5-(4-amino phenyl sulphonamido)-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamide (7a–g) from acetazolamide by modified Schotten–Bauman synthesis method, and compounds (9a–j) reported herein are evaluated for anticancer activity, having better therapeutic index for free radical scavenging, antimitotic activity and in vitro cytotoxic activity by MTT assay for establishing their possible therapeutic value. The synthesized molecules have been characterized by various techniques such as NMR, FTIR and LCMS.
Results and discussion
Chemistry
5-Amino-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamides (4a–g) were prepared by hydrolysis of the benzoylated acetazolamides (3a–g), which was prepared from the acetazolamide (1) by benzoylation with substituted benzoyl chlorides (2a–g). Compound (4) was refluxed with substituted aromatic aldehydes (8a–j) using concentrated sulphuric acid as a catalyst to obtain the Schiff bases (Scheme 1).
Synthesis of 5-amino-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamide (4a–g), 5-(4-acetamido phenyl sulphonamido)-1,3,4-thiadiazole-2-[N-(substituted benzoyl)]sulphonamide (6a–g), 5-(4-amino phenyl sulphonamido)-1,3,4-thiadiazole-2-[N-(substituted benzoyl)]sulphonamide (7a–g), and 5-arylidine amino-1,3,4-thiadiazol-2-[N-(substituted benzoyl)]sulphonamide (9a–j)
The FT-IR spectra showed stretching at 3,485–3,265 cm−1 (sulphonamide N–H), 3,037.4 (Ar C–H), 1,676–1,645 (C=O), 1,625–1,594 cm−1 (C=N), 1,517–1,530.9 (Ar C–C), 1,270 cm−1 (C–N), 1,177–1,125 cm−1 (sulphonamide), 1,128–1,030 cm−1 (S=O) and 756–662 cm−1 (thiadiazole C–S). The 1H-NMR spectra of all compounds indicated expected peaks in the region of 1.249–1.254 δ ppm (s, Ar–SO2NH), 3.569–4.116 δ ppm (s, Schiff base CH=N) and 8.24–8.523 δ ppm (s, amide C(=O)N–H), while multiplets of aromatic ring are in the range of 6.6–8.2 δ ppm. Thin-layer chromatography (TLC) was run throughout the reaction to optimize the reaction for purity and completion.
Pharmacological evaluation
Antioxidant and free radical scavenging activity
ABTS·+ radical, lipid peroxidation, DPPH radical, superoxide anion and nitric oxide anion radical scavenging activity has been used as a quick and reliable parameter to assess the in vitro antioxidant activity. Each method relates to the generation of a different radical, acting through a variety of mechanisms and the measurement of a range of end points at a fixed time point or over a range (Miller and Rice-Evans, 1994, 1996). The different concentrations of the synthesized compounds showed antioxidant activities in a dose-dependent manner. Comparative IC50 (nM/mL) inhibitory concentrations of synthesized compounds against different free radicals are reported in Table 1. All the tested compounds showed statistically significant (P < 0.05) IC50 values. Among the tested compounds, (9c) is the most potent compound and had lowest IC50 (nM/mL) value against DPPH radical, nitric oxide anion and lipid peroxidation, while (9e) and (9f) showed maximum potency against ABTS ·+ radical and superoxide anion radical, respectively. The study also indicates that the compounds (9c), (9d) and (9f) showed the smaller IC50 (nM/mL) values even than respective standards, indicating that these compounds are more potent than the standard, and reveals that the electron-donating functional group like –OCH3 (9c and 9d) or the functional group like –OH having the ability to bind with free radical (9f) is responsible for the potency.
Antimitotic activity
The levels of the physicochemical parameters of Allium cepa (root number and root length) were recorded after treatment with various drugs at 0, 48 and 72 h and found to cause significant inhibition in the growth of roots in comparison with negative control and positive control. From the observations, it has been revealed that average root length in (9f) treatment group was decreased significantly (1.06 cm) compared with that of the negative control (3.93 cm) after 72 h of treatment. The root morphology was nearly normal during the negative control treatment, but at positive control and synthesized compound groups, the roots morphology showed an obvious difference in its appearance in that it turned to slightly yellowish to brownish in colour. Its cytotoxic effect was evident in the form of shortening and decaying of roots, while progressive increases in root length and root numbers were observed in control group. The cytotoxic effect of tested compounds inhibits root growth and mitosis to a significant extent. The compound 9f showed lowest mitotic index (0.41 %) with highest activity among all the treatment groups, and it was also observed that the number of non-dividing cells increased in all treatment groups other than negative control. As there is no antimitotic principle in water, it was considered as negative control. Ethyl methanesulphonate (EMS) was treated as positive control treatment group and induces DNA damage by a direct mechanism, acting at various sites as a monofunctional ethylating agent of nucleotides (Budavari, 1989; Sega, 1984).
Cytogenetic analysis
With the objective of investigating the possible mechanism involved in root growth inhibition, cytogenetic analysis was performed (Angayarkanni et al., 2007; Auti et al., 2010; Pavlica et al., 2000). All the tested compounds provoked strong inhibition of the mitotic index, where a statistically significant difference in relation to the control, and the decrease in the mitotic index was positively correlated with the electron-releasing group (Table 2). Changes in chromosome and cellular morphology were observed with increasing time. Partial c-mitosis (colchicine-like mitosis) and full c-mitosis, with partially functional spindles and completely normal mitotic phases, were seen in the various cells of the same root tip between 6- and 72-h time period. Cytogenetic alterations were investigated, and the results are depicted in Table 2. All the tested compounds induced chromosome and cytological alterations in treatment groups. An analysis of chromosome aberrations showed that most of the fragments detected in the different treatments were of chromosome type. The observation of chromosome breaks showed the clastogenic effect of tested compounds. The occurrence of chromosome fragments allows observation of statistically significant differences at tested synthesized compounds. In addition to the chromosome fragments, sticky metaphase and polar deviations (wrong directions of chromosome movement) were also observed. In general, it is possible to observe an increase in different abnormalities as the nucleophilic functional group concentration increased. In Allium test, a strong toxic effect of tested compounds was observed, supported by great occurrence of sticky metaphases, leading to cellular death (mitotic index decrease). All the tested compounds produced a significant decrease in mitotic index were time dependent at the treatment of 1 mg/mL. There was a statistically significant increase in total aberrant cells (P < 0.05) (aberrant cells include chromosome breaks, thickness and polar deviation) as compared with the negative control (Table 2); however, the highest value of aberrant cells is shown by the positive control. Statistical analysis showed that the genotoxic activities of the tested compounds induced micronuclei in the root tip meristem cells of A. cepa. Micronucleus formation in 1,000 cells per slide (‰MNC value) was also increased in tested compounds and in positive control EMS compared with negative control, which is statistically significant (P < 0.05).
In the light of the results obtained in the present study, these observations above may be due to the genotoxic and nucleotoxic action of the compounds or the disturbance of the formation of spindle fibres during cell division, which leads to chromosomal aberrations. Stickiness and clumping of the chromosomes were some of the most common effects of these tested compounds on the treated root tips. Stickiness usually leads to the formation of anaphase and telophase bridges, and this ends up inhibiting post-telophase, metaphase and cytokinesis, respectively, and thus hampering cell division.
In vitro cytotoxicity activity by MTT assay method
All the synthesized compounds prepared by Scheme I and previously reported (Chhajed et al., 2007, 2013) compounds were subjected to anticancer activity. CTC50 (cytotoxic concentration at which 50 % of the cells are dead after drug exposure) determined for test and standard compound with the help of MTT assay HEK 293 (epidermal kidney cell line), BT474 (breast cancer cell line) and NCI-H226 (lung cancer) cell lines by MTT method (Freshney, 2000; Edmondson et al., 1988; Prasad et al., 2005; Chiruvella et al., 2008). The viability of control cells was designated as 100 %, and the others were expressed as percentage compared to the control. The results were compared with standard drug indisulam (ISL). The results demonstrated a strong dose-dependent growth inhibition in treated cell lines. It showed that different cells had a different sensitivity to the inhibition effect of tested compounds. The results are given in Tables 3, 4 and 5 for HEK 293, BT474 and NCI-H226. Thus, from the data, it can be concluded that all test compounds are potent cytotoxic agents because of higher CTC50 at lower concentrations, and moreover, the compound (4b) (CTC50 = 0.922) and compound (7f) (CTC50 = 0.754) were found to be most potent agent among all the compounds tested against HEK 293. While compounds (9c) (CTC50 = 0.751) and (9j) (CTC50 = 0.913) were found to be most potent agent among all the compounds tested against BT474 and NCI-H226 cell lines, respectively. But none of tested compound was found to be potent compared to standard drug indisulam. From above all cell lines such as HEK 293, M468 and NCI-H226, it has been concluded that compounds (7f), (6f), (9b), (9c) and (9j) are more potent than all synthesized compounds. Compounds (6e) and (6b) have moderate activity than all synthesized compounds. Compounds (4a) and (9 g) have less activity than all synthesized compounds on all cell lines. Structure activity relationship of compounds showed that the presence of NH linker between aryl moiety which is substituted by electron-withdrawing group and 1,3,4-thiadiazole ring has been recognized as potent anticancer agent. Substitution on phenyl ring with chloro, methoxy and nitro group gives better anticancer activity.
The order of cytotoxic activity was electron-withdrawing group on phenyl > electron-donating group on phenyl > phenyl.
We can conclude that electron-releasing group on phenyl ring is responsible for less activity.
Conclusion
Thiadiazoles are mesoionic system, a poly-heteroatomic system containing a five-membered heterocycle associated with a conjugation of p and π electrons and distinct regions of positive and negative charges leading to highly polarizable derivatives. This distinctive characteristic allows mesoionic compounds to effectively cross-cellular membranes and interact with biological molecules in unique ways. The good liposolubility of the sulphur atom in the heterocycle might also have a positive effect on the biological activity and pharmacokinetic properties of thiadiazole-containing compounds. The thiadiazole ring possesses similar chemical properties to the pyrimidine ring and can be considered a bioisostere. Given that the pyrimidine structure is found in nucleobases, components of nucleotides and the building blocks of DNA and RNA, it seems likely that thiadiazole could readily interact with DNA and RNA, potentially explaining the broad and often potent activity. Furthermore, this activity against DNA suggests that thiadiazoles derivatives could potentially be used for chemical intervention at the gene level. Compounds containing thiadiazole with high potency have been reported here, and some of them displayed excellent activities against a range of tumour cells. The ability of thiadiazoles to target DNA could explain their potential anticancer activity as uncontrolled DNA replication/cell division is a hallmark of neoplastic diseases. Furthermore, the heteroatoms of the thiadiazole are able to form interactions, such as hydrogen bonds, with biological targets that include key kinases that participate in tumorigenesis, such as CA IX and XII.
The sulfonyl group of sulphonamides is similar to the carbonate ion and can competitively inhibit CAs. Compounds containing a thiadiazole, a benzene bioisostere, should also possess high inhibitory activity when bonded with a sulphamide group. From lead compound, acetazolamide, some of the most potent compounds were synthesized and evaluated several sulphonamides as inhibitors of in vitro cancer cell growth compared with selective hCA IX inhibitor, indisulam. The affinity of 1,3,4-thiadiazole for hCA increases significantly when substituted with sulphonamides connected with Schiff base. These results indicate that the thiadiazole ring has receptor-binding ability in the context of hCA IX inhibition and in the prevention of cancer associated with CA.
Experimental section
Synthetic study
Melting points were determined in one-end-open capillary tubes on a Thermonik Precision melting point apparatus (C-PMP-2, Mumbai, India) and presented without any corrections. The IR spectra (\(\tilde{\nu}\) , cm−1) were recorded in KBr tablets using Shimadzu FT-IR 8400s spectrophotometer. 1H nuclear magnetic resonance (1H-NMR) spectra were recorded for the compounds on Varian EM-390 apparatus by using TMS as an internal standard. 13C-NMR spectra were recorded for the compounds on Bruker Avance II 400 NMR Spectrometer apparatus using TMS as an internal standard, and chemical shifts are reported in ppm (δ-scale).
Elemental analysis of the obtained compounds was performed for C, H, N, S using Elemental Vario EL III Carlo Erba 1106 analyzer. The maximum percentage differences between calculated and found values for each element were within the error and amounted to ±0.4 %. The completion of reaction and the purity of the obtained compounds were checked by TLC on aluminium oxide 60 F254 plates (Merck Co., Whitehouse Station, NJ, USA), in a CHCl3/C2H5OH (3:1, v/v) solvent system. The spots were developed in iodine chamber and visualized under ultra violet lamp (λ = 254 nm).
General procedure
N-[(5-Amino-1,3,4-thiadiazol-2-yl)sulfonyl]benzamide (4); 5-[(4-acetamido)benzene sulphonamido]-1,3,4-thiadiazol-2-(N-benzoyl)sulphonamide (6); and 5-[(4-amino)benzene sulphonamido]-1,3,4-thiadiazol-2-(N-benzoyl)sulphonamide (7) were synthesized, and their physicochemical and spectral data were reported previously (Chhajed et al., 2007, 2013). The synthesis outline is depicted in Scheme 1.
N-{[5-(Benzylidenamino)-1,3,4-thiadiazol-2-yl]sulphonyl} benzamide (9a)
Offwhitecrystals (EtOH) (this compound was prepared by refuxing 5-amino-1,3,4-thiadiazol-2-[N-(benzoyl)]sulphonamide (2.74 g, 0.01 mol) (4a) and benzaldehyde (8a) (1.06 g, 0.01 mol) in ethanol (20 mL) using 2–3 drops of sulphuric acid as catalyst, for 12 h. Pour it with thin stream into crushed ice. It was obtained as yellowish coloured solid and recrystallized by ethanol); yield: 63 %; Mp: 185–187 °C; UV (MeOH) λ max (log ε) 287 nm; R f = 0.62 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,625.1, 3,037.4, 1,693.4, 1,678.7, 1,624.32, 1,598.4, 1,557.7, 1,517–1,530.9, 1,369.6, 1,290.5, 907.25, 764.44, 756.54, 694.91 cm−1; 1H-NMR (DMSO, 400 MHz): δ = 1.257 (1H, s, –CH–), 2.134 (6H, m, CH–C6H5), 2.590 (6H, m, CO–C6H5), 3.965 (1H, s, CH=N), 4.18 (1H, s, N–H), 7.664–7.685 ppm (10H, m, Ar–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 171.46 (C, amide), 168.56 (C2, thiadiazole), 166.67 (C5, thiadiazole), 160.68 (C, imine), 137.78 (C1, Ar′–C-imine), 136.05 (C1, Ar–C-amide), 134.24 (C4, CH–Ar′), 132.52 (C3, CH–Ar), 131.71 (C3, CH–Ar′), 130.39 (C5, CH–Ar), 129.29 (C2, CH–Ar′), 129.15 (C6, CH–Ar′), 128.84 (C2, CH–Ar), 128.42 (C6, CH–Ar), 127.34 (C5, CH–Ar′); EIMS m/z [M]+ 370.9 (100); Anal. Calcd. for C16H12N4O3S2: C, 51.60; H, 3.25; N, 15.04; S, 17.22. Found: C, 51.61; H, 3.24; N, 15.05; S, 17.22.
N-({5-[(4-Chlorobenzylidene)amino]-1,3,4-thiadiazol-2-yl}sulfonyl)benzamide (9b)
Yield: 64.2 %: Mp: 212–214 °C; λ max (log ε) 305 nm; R f = 0.65 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,465.3, 3,417.47, 3,148.51, 1,673.2–1,668.7, 1,624.32–1,598.4, 1,545.9, 1,538.1–1,527.4, 1,368.9–1,358.8, 1,169.9, 968.07, 848–826.5, 764.43–674.43, 764.43 cm−1; 1H-NMR (DMSO, 400 MHz): δ = 1.359 (1H, s, –CH–), 2.342 (6H, m, CH–C6H5), 2.678 (6H, m, CO–C6H5), 3.623 (1H, s, CH=N), 4.41 (1H, s, N–H), 7.462–8.104 (10H, m, Ar–H) 8.24- 8.362 ppm (1H, s, C(=O)N–H); 13C–NMR ([D]6DMSO, 75 MHz): δ = 170.64 (C, amide), 168.41 (C5, thiadiazole), 166.58 (C2, thiadiazole), 161.68 (C, imine), 136.24 (C4, Cl–C–Ar′), 134.16 (C1, Ar–C-amide), 133.78(C1, Ar′–C-imine), 130.25 (C4, CH–Ar), 129.15 (C3, CH–Ar′), 129.29 (C5, CH–Ar′), 129.02 (C3, CH–Ar), 128.97 (C5, CH–Ar), 128.84 (C2, CH–Ar′), 128.42 (C6, CH–Ar′), 127.34 (C2, CH–Ar), 127.29 (C6, CH–Ar); EIMS m/z [M]+ 412.9 (100); Anal. calcd. for C16H11N4O3S2Cl: C, 47.23; H, 2.73; N, 13.77; S, 15.76. Found: C, 47.24; H, 2.72; N, 13.75; S, 15.77.
N-({5-[(2-Methoxybenzylidene)amino]-1,3,4-thiadiazol-2-yl}sulfonyl)benzamide (9c)
Yield: 62.8 %; Mp: 201–203 °C; UV (MeOH) λ max (log ε) 315 nm; R f = 0.57 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,625.4, 3,048.7, 2,915.3–2,903.2, 1,692.8, 1,681.1–1,665.4, 1,599.9–1,536.5, 1,426.5, 1,347.1, 1,290, 1,143.2–1,129.4, 930.13–923.7, 762.6–713.1, 762.6 cm−1 (thiadiazole C–N stretching); 1H-NMR (DMSO, 400 MHz): δ = 1.352 (1H, s, –CH–), 3.134 (1H, s, CH–C6H5), 3.417–3.487 (3H, m, –OCH3), 6.364 (1H, s, Ar′–H3,5), 6.84–7.16 (3H, J = 7.2 Hz, t, Ar–H3,4,5), 8.285 (2H, J = 2.4 Hz, d, Ar–H2,6), 8.58 ppm (1H, s, N–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 168.21(C, amide), 164.03 (C2, C–Ar′–OCH3), 163.77(C, imine), 162.32 (C2, thiadiazole), 162.28 (C5, thiadiazole), 134.25(C1, CH–Ar), 132.22 (C4, CH–Ar), 130.76 (C4, CH–Ar′), 130.32 (C6, CH–Ar′), 128.66 (C3, CH–Ar), 128.45 (C5, CH–Ar), 128.23 (C1, CH–Ar′), 127.55 (C2, CH–Ar), 127.46 (C6, CH–Ar), 120.84 (C3, CH–Ar′), 120.44 (C5, CH–Ar′), 62.32 (C, aliphatic, OCH3) ppm; EIMS m/z [M]+ 404.6 (100); Anal. calcd. for C17H14N4O4S2: C, 50.74; H, 3.51; N, 13.92; S, 15.93. Found: C, 50.74; H, 3.52; N, 13.95; S, 15.92.
N-({5-[(4-Methoxybenzylidene)amino]-1,3,4-thiadiazol-2-yl}sulfonyl)benzamide (9d)
Yield: 65.3 %; Mp: 215–217 °C; λ max (log ε) 287 nm; R f = 0.45 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,659.8–3,625.4, 2,915.3–2,903.2, 2,884.5, 1,692.8, 1,681.1–1,665.4, 1,599.9–1,536.5, 1,426.5, 1,347.1, 1,290–1,274.4, 1,143.2–1,013.4, 930.13–923.7, 786.79–762.6, 762.6 cm−1; 1H-NMR (DMSO, 400 MHz): δ = 3.721 (3H, s, –OCH3), 6.463 (2H, s, Ar′–H3,5), 7.331–7.62 (5H, J = 3.0 Hz, d, Ar–H), 8.125 (3H, s, Ar–H2,6), 8.24 ppm (1H, s, C(=O)N–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 170.34 (C, amide), 165.29 (C4, C–Ar′-OCH3), 163.51 (C, imine), 162.85 (C2, thiadiazole), 162.34 (C5, thiadiazole), 134.29(C1, CH–Ar), 134.01 (C4, CH–Ar), 130.49 (C6, CH–Ar′), 130.11 (C2, CH–Ar′), 128.94 (C3, CH–Ar), 128.22 (C5, CH–Ar), 128.11 (C1, CH–Ar′), 127.42 (C2, CH–Ar), 127.16 (C6, CH–Ar), 114.33 (C5, CH–Ar′), 114.08 (C3, CH–Ar′), 69.41 (C, OCH3) ppm; EIMS m/z [M]+ 403.9 (100); Anal. calcd. for C17H14N4O4S2: C, 50.74; H, 3.51; N, 13.92; S, 15.93. Found: C, 50.72; H, 3.52; N, 13.96; S, 15.94.
N-({5-[(4-Hydroxybenzylidene)amino]-1,3,4-thiadiazol-2-yl}sulfonyl)benzamide (9e)
Yield: 68.2 %; Mp: 178–180 °C; UV (MeOH) λ max (log ε) 375 nm; R f = 0.59 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,769–3,719.8, 3,671.56–3,523.8, 2,884.5, 1,713.8, 1,673.7–1,665.4, 1,599.9–1,549, 1,454.6–1,424.2, 1,317.8, 1,292–1,174.8, 1,174.8–1,052.1, 931.21–921.7, 786.79–762.6, 761.6–725.58 cm−1; 1H-NMR (400 MHz, DMSO): δ = 3.569 (1H, s, CH=N), 4.684 (1H, s, –OH), 6.547–8. 623 (9H, m, Ar–H), 8.31 ppm (1H, s, C(=O)N–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 169.43 (C, imine), 167.11(C, amide), 161.32 (C4, C–Ar′–OH), 161.02 (C2, thiadiazole), 160.98 (C5, thiadiazole), 134.52 (C1, CH–Ar), 131.17 (C4, CH–Ar), 130.62 (C6, CH–Ar′), 130.26 (C2, CH–Ar′), 128.82 (C3, CH–Ar), 128.29 (C5, CH–Ar), 127.34 (C1, CH–Ar′), 127.55 (C2, CH–Ar), 127.21 (C6, CH–Ar), 114.83 (C5, CH–Ar′), 114.12 (C3, CH–Ar′), ppm; EIMS m/z [M]+ 386.6 (100); Anal. calcd. for C16H12N4O4S2: C, 49.48; H, 3.11; N, 14.42; S, 16.51. Found: C, 49.50; H, 3.12; N, 14.40; S, 16.51.
N-({5-[(2-Hydroxybenzylidene)amino]-1,3,4-thiadiazol-2-yl}sulfonyl)benzamide (9f)
Yield: 64.6 %; Mp: 220–222 °C; UV (MeOH) λ max (log ε) 478 nm; R f = 0.64 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,489.1, 3,261.43, 2,948.5–2,884.5, 1,731.22–1,635.4, 1,614.217–1,589, 1,436.06–1,505.64, 1,330.70, 1,232.41–1,093.86, 1,093.86, 974.20–841.7, 822.2–780.44, 761.6–725.58 cm−1; 1H-NMR (400 MHz, DMSO): δ = 3.582 (1H, s, CH = N), 4.237 (1H, s, –OH), 6.413–8.548 (9H, m, Ar–H), 8.41 ppm (1H, s, C(=O)N–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 166.14 (C, imine), 165.26 (C, amide), 164.21 (C, C2–Ar′–OH), 160.72 (C5, thiadiazole), 160.19 (C2, thiadiazole), 134.82 (C1, CH–Ar), 132.77 (C4, CH–Ar′), 131.38 (C4, CH–Ar), 130.15 (C6, CH–Ar′), 128.81 (C3, CH–Ar), 128.49 (C5, CH–Ar), 128.09 (C5, CH–Ar′), 127.40 (C2, CH–Ar), 127.12 (C6, CH–Ar), 114.52 (C1, CH–Ar′), 114.33 (C3, CH–Ar′), ppm; EIMS m/z [M]+ 389.4 (100); Anal. calcd. for C16H12N4O4S2: C, 49.48; H, 3.11; N, 14.42; S, 16.51. Found: C, 49.47; H, 3.12; N, 14.43; S, 16.52.
N-({5-[(4-Hydroxy-3-methoxy benzylidene)amino]-1,3,4-thiadiazol-2-yl}sulfonyl)benzamide (9g)
Yield: 64.2 %; Mp: 252–254 °C; UV (MeOH) λ max (log ε) 268 nm; R f = 0.67 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,537.42, 3,371.43, 2,927.5–2,853.4, 1,692.8–1,681.1, 1,665.4–1,599.9, 1,536.05–1,426.5, 1,347.1–1,290, 1,274.4–1,182.6, 1,013.4, 930.13–923.7, 844.17–762.6, 762.6–713.1 cm−1; 1H-NMR (400 MHz, DMSO): δ = 3.069 (3H, s, –OCH3), 3.659 (1H, s, CH=N), 4.428 (1H, s, –OH), 6.126–8.262 (8H, m, Ar–H), 8.523 ppm (1H, s, C(=O)N–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 170.43 (C, imine), 167.67(C, amide), 165.09 (C5, thiadiazole), 164.18 (C2, thiadiazole), 154.32 (C3, C–Ar′–OCH3), 145.13 (C4, C–Ar′–OH), 135.14 (C1, CH–Ar), 134.02 (C4, CH–Ar), 128.83 (C3, CH–Ar), 128.41 (C5, CH–Ar), 127.34 (C1, CH–Ar′), 127.21 (C2, CH–Ar), 121.62 (C6, CH–Ar′), 117.61 (C6, CH–Ar), 117.26 (C5, CH–Ar′), 114.31 (C2, CH–Ar′), 65.17 (C, Ar–OCH3), ppm; EIMS m/z [M]+ 420.1 (100); Anal. calcd. for C17H14N4O5S2: C, 48.80; H, 3.37; N, 13.39; S, 15.33. Found: C, 48.78; H, 3.38; N, 13.41; S, 15.34.
N-[(5-{[4-(Dimethylamino)benzylidene]amino}-1,3,4-thiadiazol-2-yl)sulfonyl]benzamide (9h)
Yield: 67.7 %; Mp: 236–238 °C; UV (MeOH) λ max (log ε) 305 nm; R f = 0.42 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,652.4, 3,532.12, 3,114.7, 2,985.3–2,896.4, 1,614.2–1,591.4, 1,413.1, 1,238.52–1,174.7, 804.2–783.6, 743.9–719.2 cm−1; 1H-NMR (400 MHz, DMSO): δ = 2.547 (6H, s, –NCH3), 3.956 (1H, s, CH=N), 4.114 (1H, s, N–H), 6.466–7.824 (9H, m, Ar–H), 8.511 ppm (1H, s, C(=O)N–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 169.42 (C, imine), 165.21 (C, amide), 162.15 (C2, thiadiazole), 162.11 (C5, thiadiazole), 154.32 (C4, C–Ar′–N(CH3)2), 134.63 (C1, CH–Ar), 132.46 (C4, CH–Ar), 132.23 (C2, CH–Ar′), 132.18 (C3, CH–Ar), 131.65 (C6, CH–Ar′), 128.12 (C2, CH–Ar), 128.03 (C6, CH–Ar), 127.37 (C1, CH–Ar′), 127.11 (C3, CH–Ar′), 117.52 (C5, CH–Ar), 117.11 (C5, CH–Ar′), 52.84 (C, Ar–NCH3, Aliphatic), 52.47 (C, Ar–NCH3, Aliphatic) ppm; EIMS m/z [M]+ 415.7 (100); Anal. calcd. for C19H18N4O3S2: C, 55.06; H, 4.38; N, 13.52; S, 15.47. Found: C, 55.07; H, 4.38; N, 13.53; S, 15.46.
N-({5-[(3-Nitrobenzylidene)amino]-1,3,4-thiadiazol-2-yl}sulfonyl)benzamide (9i)
Yield: 61.3 %; Mp: 258–260 °C; UV (MeOH) λ max (log ε) 352 nm; R f = 0.51 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,537.9–3,427.2, 3,128.2–3,022.3, 3,075–3,007.4, 2,341.6–2,331.1, 1,445.8, 1,456.8–1,531.7, 827, 1,022.8–1,078.2, 713.1–619.5 cm−1; 1H-NMR (400 MHz, DMSO): δ = 3.239 (1H, s, CH=N), 4.751 (1H, s, –OH), 6.872–8.421 (9H, m, Ar–H), 8.645 ppm (1H, s, C(=O)N–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 168.27 (C, imine), 165.61 (C, amide), 162.23 (C5, thiadiazole), 162.18 (C2, thiadiazole), 154.32 (C3, C–Ar′–NO2), 135.71 (C6, CH–Ar′), 134.67 (C1, CH–Ar′), 134.46 (C1, CH–Ar), 132.49 (C4, CH–Ar), 129.37 (C5, CH–Ar′), 128.35 (C3, CH–Ar), 128.22 (C5, CH–Ar), 126.13 (C4, CH–Ar′), 117.11 (C2, CH–Ar′), 116.37 (C2, CH–Ar), 116.16 (C6, CH–Ar) ppm; EIMS m/z [M]+ 416.9 (100); Anal. calcd. for C16H11N5O5S2: C, 46.04; H, 2.66; N, 16.78; S, 15.36. Found: C, 46.05; H, 2.68; N, 16.80; S, 15.36.
N-({5-[(Furan-2-ylmethylidene)amino]-1,3,4-thiadiazol-2-yl}sulfonyl)benzamide (9j)
Brownish crystals (EtOH) (this compound was prepared by refuxing 5-amino-1,3,4-thiadiazol-2-[N-(benzoyl)]sulphonamide (2.74 g, 0.01 mol) (4a) and Furfuldehyde (8j) (0.96 g, 0.01 mol) in ethanol (20 mL) using 2–3 drops of sulphuric acid as catalyst, for 7 h. Pour it with thin stream into crushed ice. It was obtained as dark brown coloured solid and recrystallized by ethanol); Yield: 53.04 %; Mp: 261–263 °C; UV (MeOH) λ max (log ε) 412 nm; R f = 0.69 (CHCl3/EtOH, 3/1); FT-IR (KBr): v max 3,634.9, 3,581.22, 3,054.2, 1,635.34, 1,622.4–1,595.9, 1,432.4, 1,254.31–1,197.7, 824.3–776.9, 741.3–711.4 cm−1; 1H-NMR (400 MHz, DMSO): δ = 2.547 (6H, s, –NCH3), 4.116 (1H, s, CH=N), 6.724–7.211 (3H, m, furfuryl-H), 7.446–7.918 (5H, m, Ar–H), 8.426 ppm (1H, s, C(=O)N–H); 13C-NMR ([D]6DMSO, 75 MHz): δ = 148.22 (C, imine), 167.19 (C, amide), 154.32 (C2, C-furfuryl), 152.13 (C2, thiadiazole), 150.84 (C5, thiadiazole), 135.71 (C5, CH-furfuryl), 134.63 (C1, CH–Ar), 132.46 (C4, CH–Ar), 128.12 (C3, CH–Ar), 128.03 (C5, CH–Ar), 117.11 (C3, CH-furfuryl), 111.24 (C2, CH–Ar), 111.06 (C6, CH–Ar), 106.10 (C4, CH-furfuryl) ppm; EIMS m/z [M]+ 364.3 (100); Anal. calcd. for C14H10N4O4S2: C, 46.40; H, 2.78; N, 15.46; S, 17.70. Found: C, 46.42; H, 2.79; N, 15.45; S, 17.39.
Pharmacological evaluation
Antioxidant and free radical scavenging activity
Total antioxidant activity
The ability of the test sample to scavenge 2,2′-azinobis-(3-ethylbenzothiazoline-6-sulphonic acid) (ABTS·+) radical cation was compared with 6-hydroxy-2,5,7,8-tetramethylchroman-2-carboxylic acid (trolox) standard (Chang et al., 2007; Erel, 2004; Re et al., 1999). The ABTS·+ radical cation was pregenerated by mixing ABTS stock solution (7 mM) with potassium persulphate (2.45 mM) (final concentration) and incubating for 12–16 h in the dark at room temperature until the reaction was complete and the absorbance was stable. The absorbance of the ABTS·+ solution was equilibrated to 0.70 (±0.02) by diluting with water at room temperature, then 1 mL of solution was mixed with 10 μL of the test sample (0.05–10 mg/mL), and the absorbance was measured at 734 nm after 6 min. All experiments were repeated three times. The percentage inhibition of absorbance was calculated and plotted as a function of the concentration of standard and sample to determine the trolox equivalent antioxidant concentration (TEAC). To calculate the TEAC, the gradient of the plot for the sample was divided by the gradient of the plot for trolox. The IC50 inhibitory concentration (nM/mL) values of tested compounds are depicted in Table 1. The ABTS·+ radical scavenging activity of the samples was expressed as
where A control is the absorbance of the blank control (ABTS·+ solution without test sample), and A sample is the absorbance of the test sample.
Lipid peroxidation inhibitory activity
Egg lecithin (3 mg/mL phosphate buffer, pH 7.4) was sonicated in an ultrasonic sonicator for 10 min to ensure proper liposome formation. Test samples or standard, ascorbic acid (100 μL) of different concentrations (10, 20, 30, 40 50 and 100 μg/mL) was added to liposome mixture (1 mL); the control was without test sample. Lipid peroxidation was induced by adding ferric chloride (10 μL, 400 mM) and L-ascorbic acid (10 μL, 200 mM). After incubation for 1 h at 37 °C, the reaction was stopped by adding hydrochloric acid (2 mL, 0.25 N) containing trichloroacetic acid (150 mg/mL), thiobarbituric acid (3.75 mg/mL) and butylated hydroxy anisole (0.50 mg/mL). The reaction mixture was subsequently boiled for 15 min, cooled and centrifuged at 1,000 rpm for 15 min, and the absorbance of the supernatant was measured at 532 nm (Duh and Yen, 1997). The IC50 values of all tested compounds are reported in Table 1. The % inhibition at different concentrations was calculated by the following formula
where V t = mean absorption of test compound, V c = mean absorption of control.
The IC50 (nM/mL) value was derived from the % inhibition at different concentrations.
DPPH radical scavenging activity
Compounds of SC series were evaluated for their in vitro free radical scavenging activities by 2,2-diphenyl-1-picrylhydrazyl (DPPH) assay method (Blois, 1958; Shishoo et al., 1999; Chhajed et al., 2007). To determine the free radical scavenging activity, a method based on the reduction of a methanolic solution of the coloured DPPH radical was used. To a set of test tubes containing methanol (3 mL), DPPH reagent (2 mg/mL) (50 μL) was added. The initial absorbance was measured. To these test tubes, methanolic solution of different test solutions (1 mg/mL) were added (10–50 μL). Ascorbic acid (0.5 mg/mL) was also added in the concentration of 10, 20, 30, 40, 50 and 100 μL. After 20 min, absorbance was recorded at 516 nm. The experiment was performed in triplicate. The percentage reduction in absorbance was calculated from the initial and final absorbance of each solution (Dhar and Taploo, 1982). The IC50 (nM/mL) values are shown in Table 1.
Superoxide anion radical scavenging effect
Measurement of superoxide anion scavenging activity of the synthesized compound was taken based on the method described by Nishimiki et al. (1972) and slightly modified. About 1 mL of nitroblue tetrazolium (NBT) solution (156 μM NBT in 100 mM phosphate buffer, pH 7.4), NADH solution (1 mL) (reduced form of β-nicotinamide adenine dinucleotide) (468 μM in 100 mM phosphate buffer, pH 7.4) and sample solution (0.1 mL) of compounds (10, 20, 30, 40, 50 and 100 μg) in distilled water were mixed and the reaction started by adding phenazine methosulphate (PMS) solution (100 μL) (60 μM PMS in 100 mM phosphate buffer, pH 7.4). The reaction mixture was incubated at 25 °C for 5 min, and the absorbance at 560 nm was measured against blank samples. Catechin was used as reference compound. All the experiments were performed in triplicate, and the results were averaged. The percentage of inhibition was determined by comparing the results of control and test samples. The IC50 (nM/mL) value are depicted in Table 1.
Nitric oxide radical scavenging effect
Nitric oxide generated from sodium nitroprusside in aqueous solution at physiological pH interacts with oxygen to produce nitrite ions, which were measured by the Griess reaction (Marcocci et al., 1994; Green et al., 1982). Scavenger of nitric oxide competes with oxygen leading to reduced production of nitric oxide (Mondal et al., 2006). The reaction mixture (3 mL) containing sodium nitroprusside (10 mM) in phosphate-buffered saline (PBS) and the compounds in different concentrations (10, 20, 30, 40, 50 and 100 μg) were incubated at 25 °C for 150 min. At every 30-min interval, the incubated sample (0.5 mL) was removed and Griess reagent (1 % sulphanilamide, 0.1 % naphthylethylene diamine dihydrochloride in 2 % H3PO4) (0.5 mL) was added. The absorbance of the chromophore formed was measured at 546 nm. All the analyses were performed in triplicate, and the results were averaged. The percentage inhibition of nitric oxide generated was measured by comparing the absorbance values of control and test. Curcumin was used as a reference compound. The IC50 (nM/mL) values are reported in Table 1.
In vitro antimitotic activity by Allium cepa (onion) meristem root model
Small bulbs (1.5–2.0 cm in diameter) of the common onion, A. cepa (2n = 16), were purchased from vendor at a local market. Prior to initiating the test, the outer scales of the bulbs and the dry bottom plate were removed without destroying the root primordia. The roots of A. cepa were grown in distilled water in Erlenmeyer flasks (200 mL capacity) under laboratory conditions (dark 24 °C). For each synthesized compound sample, after reaching a length of 3 cm (±0.5 cm), a series of six bulbs were placed in distilled water (pH 7.3) for 48 h and then onion roots were treated with the synthesized compound at 1 mg/mL concentrations of each tested compound. The test tubes were kept in an incubator at 22 ± 1 °C, and the test samples were changed daily at the same time. Several of the newly formed root tips were then cut from each bulb and examined for any visible morphological abnormalities. The bulbs with satisfactory root lengths (2–2.5 cm) were used in the study, while those with exceptionally long or short roots were discarded (on average 2–3 bulbs). Therefore, individual sets of five bulbs were used for each extract sample.
Distilled water (pH 7.3) was used as a negative control, and EMS (2 × 10−2 M) used as a positive control mutagen (Fiskesjo, 1993, 1997). After 24 h of exposure, several root tips were removed from the bulbs, fixed in 3:1 (v/v) ethanol (90 %)/glacial acetic acid (45 %) and stored overnight at 4 °C. The next day, they were placed in 70 % (v/v) aqueous alcohol and refrigerated until used. Allium roots were softened by digesting with HCl and rinsed the roots in water. After removing the water from the third rinse, the roots were covered with the orcein acetate stain. The roots were incubated in the stain for 12 min. During this time, the very tip of the root begins to turn red as the DNA stains the numerous small actively dividing cells at the tip. A root was transferred to the centre of a clean microscope slide, and a drop of water was added. Using a razor blade most of the unstained part of the root was cut off and discarded. The root tip was covered with a cover slip and then carefully pushed down on the cover slide with the wooden end of a dissecting probe. Care should be taken to push hard, but do not twist or push the cover slide sideways. The root tip should spread out to a diameter about 0.5–1 cm. Five slides were prepared per bulb.
Determination of cytotoxicity and genotoxicity
The following parameters were used for the determination of cytotoxicity and genotoxicity:
-
(i)
the mitotic index (MI) was calculated as the ratio between the number of mitotic cells and the total number of cells scored and expressed as percentage using following formula as per standard procedures.
$${\text{Mitotic}}\,{\text{index}} = \frac{{{\text{Number}}\,{\text{of}}\,{\text{dividing}}\,{\text{cells}}}}{{{\text{Total}}\,{\text{number}}\,{\text{of}}\,{\text{cells}}}} \times 100$$ -
(ii)
Chromatin aberrations (stickiness, breaks and polar deviation) were used as end points for the determination of cytogenetic effects, and micronuclei (MNC) were scored in interphase cells per 1,000 cells (‰ MNC) (Freshney, 2000).
-
(iii)
The most frequent abnormalities are shown in microphotographs. After 72 h of exposure to the test samples, the root lengths were measured and used as an index of general toxicity. The results for mitotic index and root length are expressed as percentage of the negative and positive controls. Visible morphological modifications, such as changes in root consistency and colour as well as the presence of swelling (c-tumours), hooks or twists in the roots, were also observed.
In vitro cytotoxicity activity by MTT assay method
Cell line and culture medium
The cancer cell line cultures of HEK 293 (epidermal kidney cell line), BT474 (breast cancer cell line) and NCI-H226 (lung cancer) were obtained from Pasteur Institute of India, Coonoor, India, and were cultured in RPMI-1640 and 10 % heat-activated New born calf serum with antibiotics [penicillin (1,000 I.U./mL), streptomycin (100 μg/mL) and amphotericin B (25 μg/mL)]. The cells were maintained at 37 °C in a humidified atmosphere with 5 % CO2 and were subcultured twice a week.
Determination of cytotoxicity by microculture tetrazolium (MTT) assay
The monolayer cell culture (100 μL) was trypsinized, and the cell count was adjusted to 3.0 × 105 cells/mL using medium containing 10 % new born calf serum. To each well of the 96-well microtitre plate, the diluted cell suspension (approximately 10,000 cells) (0.1 mL) was added and kept for 24 h in incubator at 37 °C in 5 % CO2 atmosphere for cell monolayer formation. After 24 h, when a partial monolayer was formed at the bottom of the well, the supernatant was flicked off, the monolayer was washed once, and different drugs, i.e. synthesized compounds (100 μL), were added to the cells in microtitre plates. The plates were then incubated at 37 °C for 3 days in 5 % CO2 atmosphere, and microscopic examination was carried out and observations recorded every 24 h. After 72 h, the sample solution in the wells was flicked off; MTT dye (50 mL) was added to each well; plates were gently shaken and incubated for 4 h at 37 °C in 5 % CO2 incubator. The supernatant was removed and propanol (50 μL) was added; the plates were gently shaken to solubilize the formed formazan. The absorbance was measured using a microplate reader at a wavelength of 490 nm (Edmondson et al., 1988; Prasad et al., 2005; Chiruvella et al., 2008; Chang et al., 2007).
References
Abrahum DJ (2003) Burger’s medicinal chemistry and drug discovery: principle and practice, vol 1, 6th edn. Wiley, New York
Angayarkanni J, Ramkumar KM, Poornima T, Priyadarshini U (2007) Cytotoxic activity of Amorphophallus paeoniifolius tuber extract in vitro. Am Eurasian J Agri Environ Sci 2(4):395–398
Ashida S, Nishimori I, Tanimura M, Onishi S, Shuin T (2002) Effects of von Hippel–Lindau gene mutation and methylation status on expression of transmembrane carbonic anhydrases in renal cell carcinoma. J Cancer Res Clin Oncol 128(10):561–568
Auti S, Pagare R, Ahire D, Sawale V (2010) Cytogenetical studies on the effect of omnacortil on root tip cells of Allium cepa L. J Cell Tissue Res 10(3):2331–2335
Blois MS (1958) Antioxidant determination by the use of a stable free radical. Nature 181(4617):1199–1200. doi:10.1038/1811199a0
Brackett CC, Singh H, Block JH (2004) Likelihood and mechanisms of cross-allergenicity between sulfonamide antibiotics and other drugs containing a sulfonamide functional group. Pharmacotherapy 24(7):856–870
Brzozowski Z, Slawinski J, Saczewski F, Innocenti A, Supuran CT (2010) Carbonic anhydrase inhibitors: synthesis and inhibition of the human cytosolic isozymes I and II and transmembrane isozymes IX, XII (cancer-associated) and XIV with 4-substituted 3-pyridinesulfonamides. Eur J Med Chem 45(6):2396–2404
Budavari S (1989) The Merck Index: an encyclopedia of chemicals, drugs, and biologicals, 11th edn. Merck Research Laboratories, Whitehouse Station, p 3782
Cecchi A, Hulikova A, Pastorek J, Pastorekova S, Scozzafava A, Winum JY, Montero JL, Supuran CT (2005) Carbonic anhydrase inhibitors. Design of fluorescent sulfonamides as probes of tumour-associated carbonic anhydrase IX that inhibit isozyme IX-mediated acidification of hypoxic tumours. J Med Chem 48(15):4834–4841
Chang HY, Ho YL, Sheu MJ, Lin YH, Tseng MC, Wu SH, Huang GJ, Chang YS (2007) Antioxidant and free radical scavenging activities of Phellinus merrillii extracts. Bot Stud 48:407–417
Chegwidden WR, Spencer IM, Supuran CT (2001) The roles of carbonic anhydrase in cancer. In: Xue G, Xue Y, Xu Z, Hammond GL, Lim AH (eds) Gene families: studies of DNA, RNA, enzymes, and proteins. World Scientific, Singapore, pp 157–169
Chhajed MR, Khedekar PB, Mundhey AS (2007) Synthesis and free radical scavenging activity of some 1,3,4-thiazole derivatives. Indian J Heterocycl Chem 16:259–262
Chhajed MR, Shrivastava AK, Taile VS (2013) Design and syntheses of some new 5-[benzene sulphonamido]-1,3,4-thiadiazol-2-sulphonamide as potent antiepileptic agent. Macroheterocycles 6(2):199–209. doi:10.6060/mhc130116c
Chiruvella KK, Kari V, Choudhary B, Nambiar M, Ghanta RG, Raghavan SC (2008) Methyl angolensate, a natural tetranortriterpenoid induces intrinsic apoptotic pathway in leukemic cells. FEBS Lett 582(29):4066–4076. doi:10.1016/j.febslet.2008.11.001
Desai NC, Shukla HK, Astik RR, Thaker KA (1984) Studies on some thiosemicarbazones and 1,3,4-thiadiazolines as potential anti-tubercular and antibacterial agents. J Indian Chem Soc LXI:168–196
Dhar DN, Taploo CL (1982) Schiff bases and their applications. J Sci Ind Res 41:501–506
Duh PD, Yen GH (1997) Antioxidative activity of three herbal water extracts. Food Chem 60:639–645
Edmondson JM, Armstrong LS, Martinez AO (1988) A rapid and simple MTT-based spectrophotometric assay for determining drug sensitivity in monolayer cultures. J Tissue Cult Methods 11:15–17
Erel O (2004) A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin Biochem 37(4):277–285
Eroglu E (2008) Some QSAR studies for a group of sulfonamide Schiff base as carbonic anhydrase CA II inhibitors. Int J Mol Sci 9:181–197
Fiskesjo G (1993) Allium test I: a 2–3 day plant test for toxicity assessment by measuring the mean root growth of onions (allium cepa L.). Environ Toxicol Water Qual 8(4):461–470. doi:10.1002/tox.2530080410
Fiskesjo G (1997) Allium test for screening chemicals; Evaluation of cytological parameters. In: Wang W, Gorsuch JW, Hughes JS (eds) Plants for environmental studies. CRC Lewis Publishers, New York, pp 308–333
Freshney RI (2000) Cytotoxicity. In: Liss AR (ed) Cultures of animal cells, a manual of basic technique. Wiley, New York
Fujikawa-Adachi K, Nishimori I, Taguchi T, Onishi S (1999) Human carbonic anhydrase XIV (CA14): cDNA cloning, mRNA expression, and mapping to chromosome 1. Genomics 61(1):74–81
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JK, Tannenbaum SR (1982) Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal Biochem 126(1):131–138
Gupta A, Mishra P, Kashaw SK, Jatav V, Stables JP (2008) Synthesis of 3-aryl amino/amino-4-aryl-5-imino-D2-1,2,4-thiadiazoline and evaluated for anticonvulsant activity. Eur J Med Chem 43(4):749–754
Hanna MA, Girges MM, Rasala D, Gawinecki R (1995) Synthesis and pharmacological evaluation of some novel 5-(pyrazol-3-yl)-thiadiazole and oxadiazole derivatives as potential hypoglycemic agents. Arzneim-Forsch- Drug Res 45(10):1074–1078
Harrison TR (1994) Harrison’s principles of internal medicine, 13th edn. McGraw-Hill, New Delhi, p 604
Jatav V, Mishra P, Kashaw S, Stables JP (2008) CNS depressant and anticonvulsant activities of some novel 3-[5-substituted-1,3,4-thiadiazole-2-yl]-2-styryl quinazoline-4(3H)-ones. Eur J Med Chem 43(9):1945–1954
Kamb A (2005) Opinion: what’s wrong with our cancer models? Nat Rev Drug Discov 4(2):161–165
Kaunisto K, Parkkila S, Rajaniemi H, Waheed A, Grubb J, Sly WS (2002) Carbonic anhydrase XIV: luminal expression suggests key role in renal acidification. Kidney Int 61(6):2111–2118
Khan SA, Siddiqui AA, Shibeer B (2002) Analgesic activity of isatin derivatives. Asian J Chem 14:1117–1118
Kumar A, Shrivastava VK, Archana (2003) Synthesis of newer indolyl thiadiazoles and their thiazolidinones and formazans as potential anticonvulsant agents. Indian J Pharm Sci 65(4):358–362
Kumar D, Kumar MN, Chang KH, Shah K (2010) Synthesis and anticancer activity of 5-(3-indolyl)-1,3,4-thiadiazoles. Eur J Med Chem 45(10):4664–4668
Kuzmin VE, Artemenko AG, Lozytska RN, Fedtchouk AS, Lozitsky VP, Muratov EN, Mescheriakov AK (2005) Investigation of anticancer activity of macrocyclic Schiff bases by means of 4D-QSAR based on simplex representation of molecular structure. Environ Res 16(3):219–230
Manrao MR, Kaur B, Shrma RC, Kalsi PS (1982) Reaction of active methylene compounds with veratraldehyde Schiff bases and antifungal activity of products. Ind J Chem 21:1054–1060
Manrao MR, Singh B, Shrma JR, Kalsi PS (1995) Effect o hydroxyl group on antifungal activity of Schiff bases. Pestic Res J 7:157–159
Manrao MR, Goel M, Shrma JR (2001) Synthesis and fungitoxicity of ketimines of acetophenone. Ind J Agric Chem 34:86–88
Marcocci L, Maguire JJ, Droy-Lefaix MT, Packer L (1994) The nitric oxide scavenging property of Ginkgo biloba extract EGb 761. Biochem Biophys Res Comm 201(2):748–755
Miller NJ, Rice-Evans CA (1994) Total antioxidant status in plasma and body fluids. Methods Enzymol 234:279–293
Miller NJ, Rice-Evans CA (1996) Spectrophotometric determination of antioxidant activity. Redox Rep 2:161–171
Minchinton AI, Tannock IF (2006) Drug penetration in solid tumours. Nat Rev Cancer 6(8):583–592
Mondal SK, Chakraborty G, Gupta M, Muzumdar UK (2006) In vitro antioxidant activity of Diospyros malabarika kostel bark. Indian J Exp Biol 44:39–44
More SV, Dongarkhadekar DV, Chavan RN, Jadhav WW, Bhusare SR, Pawar RP (2002) Synthesis and antibacterial activity of new Schiff bases, 4-thiazolidinones and 2-azetidinones. J Ind Chem Soc 79:768–769
Nishimiki M, Rao NA, Yagi K (1972) The occurrence of superoxide anion in the reaction of reduced phenazine methosulphate and molecular oxygen. Biochem Biophys Res Comm 46(2):849–853
Noolvi MN, Patel HM, Singh N, Gadad AK, Cameotra SS, Badiger A (2011) Synthesis and anticancer evaluation of novel 2-cyclopropylimidazo[2,1-b][1,3,4]-thiadiazole derivatives. Eur J Med Chem 46(9):4411–4418
Oruc EE, Rollas S, Kandemirli F, Shvets N, Dimoglo AS (2004) 1,3,4-Thiadiazole derivatives. Synthesis, structure elucidation, and structure-antituberculosis activity relationship investigation. J Med Chem 47:6760–6767
Pacheco H, Correnberger L, Pillon D, Thiolliere JT (1970) Chem Abstr 72:111001–111002
Pandey VK, Tusi S, Tusi Z, Raghubir R, Dixit M, Joshi MN, Bajpai SK (2004) Thiadiazolyl quinazolones as potential antiviral and antihypertensive agents. Indian J Chem 43B:180–183
Parkkila S, Rajaniemi H, Parkkila AK, Kivelä J, Waheed A, Pastorekova S, Pastorek J, Sly WS (2000) Carbonic anhydrase inhibitor suppresses invasion of renal cancer cells in vitro. Proc Natl Acad Sci USA 97:2220–2224
Parkkila S, Parkkila AK, Rajaniemi H, Shah GN, Grubb JH, Waheed A, Sly WS (2001) Expression of membrane-associated carbonic anhydrase XIV on neurons and axons in mouse and human brain. Proc Natl Acad Sci USA 98(4):1918–1923
Parkkila S, Kivela AJ, Kaunisto K, Parkkila AK, Hakkola J, Rajaniemi H, Waheed A, Sly WS (2002) The plasma membrane carbonic anhydrase in murine hepatocytes identified as isozyme XIV. BMC Gastroenterol 2:13. doi:10.1186/1471-230X-2-13
Pastorek J, Pastorekova S, Callebaut I, Marnon JP, Zelnik V, Opavsky R, Zatovicova M, Liao S, Portetelle D, Stanbridge EJ, Zavada J, Burny A, Kettmann R (1994) Cloning and characterization of MN, a human tumor-associated protein with a domain homologous to carbonic anhydrase and a putative helix-loop-helix DNA binding segment. Oncogene 9(10):2877–2888
Pastorekova S, Parkkila S, Parkkila AK, Opavsky R, Zelnik V, Saarnio J, Pastorek J (1997) Carbonic anhydrase IX, MN/CA IX: analysis of stomach complementary DNA sequence and expression in human and rat alimentary tracts. Gastroenterology 112(2):398–408
Patil R, Biradar JS (2001) Synthesis and pharmacological evaluation of Substituted–2-triazolo(3,4-b)[1,3,4,]-thiadiazoles. Indian J Pharm Sci 63(4):299–305
Pattan SR, Kekare P, Dighe NS, Nirmal SA, Musmade DS, Parjane SK, Daithankar AV (2009) Synthesis and biological evaluation of some 1,3,4-thiadiazoles. J Chem Pharm Res 1(1):191–198
Pavlica M, Besendorfer V, Rosa J, Papes D (2000) The cytotoxic effect of wastewater from the phosphoric gypsum depot on common oak (Quercus robur L.) and shallot (Allium cepa var. ascalonicum). Chemosphere 41(10):1519–1527
Prasad KN, Ashok G, Raghu C, Shivamurthy GR, Vijayan P, Ardhya SM (2005) In vitro cytotoxic properties of Ipomoea aquatica leaf. Indian J Pharmacol 37(6):397–398. doi:10.4103/0253-7613.19079
Rathelot P, Azas N, El-Kashef H, Delmas F, Di Giorgio C, Timon-David P, Maldonado J, Venelle P (2002) 1,3-Diphenylpyrazoles: synthesis and antiparasitic activities of azomethine derivatives. Eur J Med Chem 37(8):671–679
Re R, Pellegrini N, Proteggente A, Pannala A, Yang M, Rice-Evans C (1999) Antioxidant activity applying an improved ABTS radical cation decolorization assay. Free Radic Biol Med 26(9/10):1231–1237
Salimon J, Salih N, Yousif E, Hameed A, Ibraheem H (2010) Synthesis and antibacterial activity of some new 1,3,4-oxadiazole and 1,3,4-thiadiazole derivatives. Aus J Basic Appl Sci 4(7):2016–2021
Sega GA (1984) A review of the genetic effects of ethyl methanesulfonate. Mutat Res 134(2–3):113–142
Sharma KP, Jolly VS, Pathak P (1998) Schiff base and their derivatives as potential anticancer agents. Ultra Sci Phys Sci 10:263–266
Sharma R, Talesara GL, Nagda DP (2006) Synthesis of various isoniazidothiazolidinones and their imidoxy derivatives of potential biological interest. Arkivoc i:1–12
Sharma R, Sainy J, Chatuvedi SC (2008) 2-Amino-5-sulfanyl-1,3,4-thiadiazoles: a new series of selective cyclooxygenase-2 inhibitors. Acta Pharm 58(3):317–326
Shishoo CJ, Ravikumar T, Jain KS, Rathod IS, Gandhi TP, Satia MC (1999) Synthesis of novel 1,2‐(un)substituted‐3‐amino‐5‐aryl‐6‐arylaminopyrazolo[3,4‐d]pyrimidin‐4(5H)‐ones and their biological activities. Indian J Chem 38(9):1075–1085
Shrivastava SK, Shrivastava S, Shrivastava SD (1999) Synthesis of new carbazolyl-thiadiazole-2-oxoazetidines: antimicrobial, anticonvulsant and anti-inflammatory agents. Indian J Chem 38B:183–187
Slatore CG, Tilles SA (2004) Sulfonamide hypersensitivity. Immunol Allergy Clin N Am 24(3):477–490
Stillings MR, Welbourn AP, Walter DS (1986) Substituted 1,3,4-thiadiazoles with anticonvulsant activity. 2. Aminoalkyl derivatives. J Med Chem 29:2280–2284
Supran CT, Barboiu M, Luca C, Pop E, Brewster ME, Dinculescu A (1996) Carbonic anhydrase activators, part 4, synthesis of mono and bis pyridinium salt derivatives of 2-amino-5-(2-aminoethyl)-and 2-amino-5-(3aminopropyl)-1,3.4-thiazole and their Interaction with isoenzyme (II). Eur J Med Chem 31:597–606
Supran CT, Scozzafava A, Casini A (2003) Carbonic anhydrase inhibitors. Med Res Rev 23(2):146–189
Supuran CT (2008) Carbonic anhydrases: novel therapeutic applications for inhibitors and activators. Nat Rev Drug Discov 7(2):168–181
Supuran CT, Scozzafava A (2000) Carbonic anhydrase inhibitors and their therapeutic potential. Expert Opin Ther Pat 10:575–600
Supuran CT, Scozzafava A, Conway I (2004) Carbonic anhydrase, its inhibitors and activators. CRC, New York, pp 1–363
Svastova E, Hulikova A, Rafajova M, Zatovicova M, Gibadulinova A, Casini A, Cecchi A, Scozzafava A, Supuran CT, Pastorek J, Pastorekova S (2004) Hypoxia activates the capacity of tumour-associated carbonic anhydrase IX to acidify extracellular pH. FEBS Lett 577(3):439–445
Taggi AE, Hafez AM, Wack H, Young B, Lectka D (2002) The development of the first catalyzed reaction of ketenes and imines: catalytic, asymmetric synthesis of β-lactams. J Am Chem Soc 124:6626–6635
Tilles SA (2001) Practical issues in the management of hypersensitivity reactions: sulfonamides. South Med J 94(8):817–824
Tureci O, Sahin U, Vollmar E, Siemer S, Gottert E, Seitz G, Parkkila AK, Shah GN, Grubb JH, Pfreundschuh M, Sly WS (1998) Human carbonic anhydrase XII: cDNA cloning, expression, and chromosomal localization of a carbonic anhydrase gene that is overexpressed in some renal cell cancers. Proc Natl Acad Sci USA 95(13):7608–7613. doi:10.1073/pnas.95.13.7608
Vaghasiya YK, Nair RS, Baluja M, Chanda S (2004) Synthesis, structural determination and antibacterial activity of compounds derived from vanillin and 4-aminoantipyrine. J Serb Chem Soc 69:991–998
Varandas LS, Fraga CAM, Miranda ALP, Barreiro EJ (2005) Design, synthesis and pharmacological evaluation of new nonsteroidal anti-inflammatory 1,3,4-thiadiazole derivatives. Lett Drug Des Discov 2(1):62–67
Verma M, Pandya SN, Singh KN, Stables JP (2004) Anticonvulsant activity of Schiff bases of isatin derivatives. Acta Pharm 54(1):49–56
Wilson CO, Gisvold O (1991) Anti-infective agents, antibacterial antibiotics. In: Swarbrick EA (ed) Textbook of organic medicinal and pharmaceutical chemistry, 9th edn. Wiley, New York
Wykoff CC, Beasley JN, Watson PH, Turner KJ, Pastorek J, Sibtain A, Wilson DG, Turley H, Talks KL, Maxwell HP, Pugh WC, Ratcliffe JP, Harris LA (2000) Hypoxia-inducible expression of tumor-associated carbonic anhydrases. Cancer Res 60:7075–7083
Zamani K, Faghihi K, Tofighi T, Shariatzadeh MR (2004) Synthesis and antimicrobial activity of some pyridyl and naphthyl substituted 1,2,4-triazole and 1,3,4-thiadiazole derivatives. Turk J Chem 28:95–100
Acknowledgments
The authors are highly thankful to Director, Sophisticated Analytical Instrumentation Facility (SAIF), Panjab University, Chandigarh; Department of Chemistry, Pune University, Pune, and Director, Sophisticated Analytical Instrumental Laboratory (SAIL), School of Pharmaceutical Sciences, Rajiv Gandhi Proudyogiki Viswavidyalaya, Bhopal for providing for providing the necessary spectral analysis facilities to carry out this research work.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Chhajed, M., Shrivastava, A.K. & Taile, V. Synthesis of 5-arylidine amino-1,3,4-thiadiazol-2-[(N-substituted benzyol)]sulphonamides endowed with potent antioxidants and anticancer activity induces growth inhibition in HEK293, BT474 and NCI-H226 cells. Med Chem Res 23, 3049–3064 (2014). https://doi.org/10.1007/s00044-013-0890-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-013-0890-z