Abstract
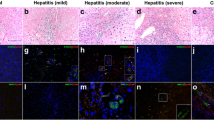
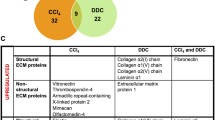
Both acute and chronic liver diseases are associated with ample re-modeling of the liver parenchyma leading to functional impairment, which is thus obviously the cause or the consequence of the disruption of the epithelial integrity. It was, therefore, the aim of this study to investigate the distribution of the adherens junction components E- and N-cadherin, which are important determinants of tissue cohesion. E-cadherin was expressed in periportal but not in perivenous hepatocytes. In contrast, N-cadherin was more enriched towards the perivenous hepatocytes. In agreement, β-catenin, which links both cadherins via α-catenin to the actin cytoskeleton, was expressed ubiquitously. This zonal expression of cadherins was preserved in acute liver injury after treatment with acetaminophen or partial hepatectomy, but disrupted in chronic liver damage like in non-alcoholic steatohepatitis (NASH) or α1-antitrypsin deficiency. Hepatocyte proliferation during acetaminophen-induced liver damage was predominant at the boundary between the damaged perivenous and the intact periportal parenchyma indicating a minor contribution of periportal hepatocytes to liver regeneration. In NASH livers, an oval cell reaction was observed pointing to massive tissue damage coinciding with the gross impairment of hepatocyte proliferation. In the liver parenchyma, metabolic functions are distributed heterogeneously. For example, the expression of phosphoenolpyruvate carboxykinase and E-cadherin overlapped in periportal hepatocytes. Thus, during liver regeneration after acute damage, the intact periportal parenchyma might sustain essential metabolic support like glucose supply or ammonia detoxification. However, disruption of epithelial integrity during chronic challenges may increase susceptibility to metabolic liver diseases such as NASH or vice versa. This might suggest the regulatory integration of tissue cohesion and metabolic functions in the liver.









Similar content being viewed by others
References
Colnot SPC (2011) Liver zonation. In: Monga SPS (ed) Molecular pathology of liver diseases, vol 5. Molecular Pathology Library, Springer, pp 7–16. doi:10.1007/978-1-4419-7107-4
Jungermann K, Katz N (1989) Functional specialization of different hepatocyte populations. Physiol Rev 69(3):708–764
Jungermann K, Kietzmann T (2000) Oxygen: modulator of metabolic zonation and disease of the liver. Hepatology 31(2):255–260. doi:10.1002/hep.510310201
Brosnan ME, Brosnan JT (2009) Hepatic glutamate metabolism: a tale of 2 hepatocytes. Am J Clin Nutr 90(3):857S–861S. doi:10.3945/ajcn.2009.27462Z
Benhamouche S, Decaens T, Godard C, Chambrey R, Rickman DS, Moinard C, Vasseur-Cognet M, Kuo CJ, Kahn A, Perret C, Colnot S (2006) Apc tumor suppressor gene is the “zonation-keeper” of mouse liver. Dev Cell 10(6):759–770. doi:10.1016/j.devcel.2006.03.015
Burke ZD, Reed KR, Phesse TJ, Sansom OJ, Clarke AR, Tosh D (2009) Liver zonation occurs through a beta-catenin-dependent, c-Myc-independent mechanism. Gastroenterology 136(7):2316–2324. doi:10.1053/j.gastro.2009.02.063 (e2311–2313)
Apte U, Zeng G, Thompson MD, Muller P, Micsenyi A, Cieply B, Kaestner KH, Monga SP (2007) Beta-catenin is critical for early postnatal liver growth. Am J Physiol Gastrointest Liver Physiol 292(6):G1578–G1585. doi:10.1152/ajpgi.00359.2006
Thompson MD, Capra V, Takasaki J, Maresca G, Rovati GE, Slutsky AS, Lilly C, Zamel N, McIntyre Burnham W, Cole DE, Siminovitch KA (2007) A functional G300S variant of the cysteinyl leukotriene 1 receptor is associated with atopy in a Tristan da Cunha isolate. Pharmacogenet Genomics 17(7):539–549. doi:10.1097/FPC.0b013e328012d0bf
Ray JG, Thompson MD, Vermeulen MJ, Meier C, Wyatt PR, Wong PY, Summers AM, Farrell SA, Cole DE (2007) Metabolic syndrome features and risk of neural tube defects. BMC Pregnancy Childbirth 7:21. doi:10.1186/1471-2393-7-21
Traweger A, Toepfer S, Wagner RN, Zweimueller-Mayer J, Gehwolf R, Lehner C, Tempfer H, Krizbai I, Wilhelm I, Bauer HC, Bauer H (2013) Beyond cell–cell adhesion: emerging roles of the tight junction scaffold ZO-2. Tissue Barriers 1(2):e25039. doi:10.4161/tisb.25039
You H, Lei P, Andreadis ST (2013) JNK is a novel regulator of intercellular adhesion. Tissue Barriers 1(5):e26845. doi:10.4161/tisb.26845
Lindner I, Hemdan NY, Buchold M, Huse K, Bigl M, Oerlecke I, Ricken A, Gaunitz F, Sack U, Naumann A, Hollborn M, Thal D, Gebhardt R, Birkenmeier G (2010) Alpha2-macroglobulin inhibits the malignant properties of astrocytoma cells by impeding beta-catenin signaling. Cancer Res 70(1):277–287. doi:10.1158/0008-5472.CAN-09-1462
Gumbiner BM (2005) Regulation of cadherin-mediated adhesion in morphogenesis. Nat Rev Mol Cell Biol 6(8):622–634. doi:10.1038/nrm1699
Halbleib JM, Nelson WJ (2006) Cadherins in development: cell adhesion, sorting, and tissue morphogenesis. Genes Dev 20(23):3199–3214. doi:10.1101/gad.1486806
Sekine S, Ogawa R, McManus MT, Kanai Y, Hebrok M (2009) Dicer is required for proper liver zonation. J Pathol 219(3):365–372. doi:10.1002/path.2606
Riehle KJ, Dan YY, Campbell JS, Fausto N (2011) New concepts in liver regeneration. J Gastroenterol Hepatol 26(Suppl 1):203–212. doi:10.1111/j.1440-1746.2010.06539.x
Hadem J, Tacke F, Bruns T, Langgartner J, Strnad P, Denk GU, Fikatas P, Manns MP, Hofmann WP, Gerken G, Grunhage F, Umgelter A, Trautwein C, Canbay A (2012) Etiologies and outcomes of acute liver failure in Germany. Clin Gastroenterol Hepatol 10(6):664–669. doi:10.1016/j.cgh.2012.02.016 (e662)
Lee WM, Stravitz RT, Larson AM (2012) Introduction to the revised American Association for the Study of Liver Diseases Position Paper on acute liver failure 2011. Hepatology 55(3):965–967. doi:10.1002/hep.25551
Stravitz RT, Kramer AH, Davern T, Shaikh AO, Caldwell SH, Mehta RL, Blei AT, Fontana RJ, McGuire BM, Rossaro L, Smith AD, Lee WM (2007) Intensive care of patients with acute liver failure: recommendations of the US. Acute Liver Failure Study Group. Crit Care Med 35(11):2498–2508. doi:10.1097/01.CCM.0000287592.94554.5F
Lee WM (2012) Recent developments in acute liver failure. Best Pract Res Clin Gastroenterol 26(1):3–16. doi:10.1016/j.bpg.2012.01.014
Younossi ZM (2008) Review article: current management of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis. Aliment Pharmacol Ther 28(1):2–12. doi:10.1111/j.1365-2036.2008.03710.x
Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA (2011) Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology 141(4):1249–1253. doi:10.1053/j.gastro.2011.06.061
Brunt EM (2004) Nonalcoholic steatohepatitis. Semin Liver Dis 24(1):3–20. doi:10.1055/s-2004-823098
Targher G, Day CP, Bonora E (2010) Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med 363(14):1341–1350. doi:10.1056/NEJMra0912063
Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G (2010) A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol 53(2):372–384. doi:10.1016/j.jhep.2010.04.008
Ekstedt M, Franzen LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S (2006) Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 44(4):865–873. doi:10.1002/hep.21327
Pan JJ, Fallon MB (2014) Gender and racial differences in nonalcoholic fatty liver disease. World J Hepatol 6(5):274–283. doi:10.4254/wjh.v6.i5.274
Kucukoglu O, Guldiken N, Chen Y, Usachov V, El-Heliebi A, Haybaeck J, Denk H, Trautwein C, Strnad P (2014) High-fat diet triggers Mallory-Denk body formation through misfolding and crosslinking of excess keratin 8. Hepatology 60(1):169–178. doi:10.1002/hep.27068
Pelz S, Stock P, Bruckner S, Christ B (2012) A methionine-choline-deficient diet elicits NASH in the immunodeficient mouse featuring a model for hepatic cell transplantation. Exp Cell Res 318(3):276–287. doi:10.1016/j.yexcr.2011.11.005
Carlson JA, Rogers BB, Sifers RN, Finegold MJ, Clift SM, DeMayo FJ, Bullock DW, Woo SL (1989) Accumulation of PiZ alpha 1-antitrypsin causes liver damage in transgenic mice. J Clin Invest 83(4):1183–1190. doi:10.1172/JCI113999
Rudnick DA, Liao Y, An JK, Muglia LJ, Perlmutter DH, Teckman JH (2004) Analyses of hepatocellular proliferation in a mouse model of alpha-1-antitrypsin deficiency. Hepatology 39(4):1048–1055. doi:10.1002/hep.20118
Stock P, Bruckner S, Winkler S, Dollinger MM, Christ B (2014) Human bone marrow mesenchymal stem cell-derived hepatocytes improve the mouse liver after acute acetaminophen intoxication by preventing progress of injury. Int J Mol Sci 15(4):7004–7028. doi:10.3390/ijms15047004
Strnad P, Zhou Q, Hanada S, Lazzeroni LC, Zhong BH, So P, Davern TJ, Lee WM, Omary MB (2010) Keratin variants predispose to acute liver failure and adverse outcome: race and ethnic associations. Gastroenterology 139(3):828–835. doi:10.1053/j.gastro.2010.06.007 (835, e821–823)
Martins PN, Theruvath TP, Neuhaus P (2008) Rodent models of partial hepatectomies. Liver Int 28(1):3–11. doi:10.1111/j.1478-3231.2007.01628.x
Anty R, Lemoine M (2011) Liver fibrogenesis and metabolic factors. Clin Res Hepatol Gastroenterol 35(Suppl 1):S10–S20. doi:10.1016/S2210-7401(11)70003-1
Takaki A, Kawai D, Yamamoto K (2013) Multiple hits, including oxidative stress, as pathogenesis and treatment target in non-alcoholic steatohepatitis (NASH). Int J Mol Sci 14(10):20704–20728. doi:10.3390/ijms141020704
Vonghia L, Michielsen P, Francque S (2013) Immunological mechanisms in the pathophysiology of non-alcoholic steatohepatitis. Int J Mol Sci 14(10):19867–19890. doi:10.3390/ijms141019867
Aurich H, Sgodda M, Kaltwasser P, Vetter M, Weise A, Liehr T, Brulport M, Hengstler JG, Dollinger MM, Fleig WE, Christ B (2009) Hepatocyte differentiation of mesenchymal stem cells from human adipose tissue in vitro promotes hepatic integration in vivo. Gut 58(4):570–581. doi:10.1136/gut.2008.154880
Ueberham E, Bottger J, Ueberham U, Grosche J, Gebhardt R (2010) Response of sinusoidal mouse liver cells to choline-deficient ethionine-supplemented diet. Comp Hepatol 9:8. doi:10.1186/1476-5926-9-8
Straub BK, Rickelt S, Zimbelmann R, Grund C, Kuhn C, Iken M, Ott M, Schirmacher P, Franke WW (2011) E–N-cadherin heterodimers define novel adherens junctions connecting endoderm-derived cells. J Cell Biol 195(5):873–887. doi:10.1083/jcb.201106023
Butz S, Larue L (1995) Expression of catenins during mouse embryonic development and in adult tissues. Cell Adhes Commun 3(4):337–352
Greve KW, Bianchini KJ, Stickle TR, Love JM, Doane BM, Thompson MD (2007) Effects of a community toxic release on the psychological status of children. Child Psychiatry Hum Dev 37(4):307–323. doi:10.1007/s10578-006-0036-3
Capra V, Thompson MD, Sala A, Cole DE, Folco G, Rovati GE (2007) Cysteinyl-leukotrienes and their receptors in asthma and other inflammatory diseases: critical update and emerging trends. Med Res Rev 27(4):469–527. doi:10.1002/med.20071
Gouw AS, Clouston AD, Theise ND (2011) Ductular reactions in human liver: diversity at the interface. Hepatology 54(5):1853–1863. doi:10.1002/hep.24613
Roskams TA, Theise ND, Balabaud C, Bhagat G, Bhathal PS, Bioulac-Sage P, Brunt EM, Crawford JM, Crosby HA, Desmet V, Finegold MJ, Geller SA, Gouw AS, Hytiroglou P, Knisely AS, Kojiro M, Lefkowitch JH, Nakanuma Y, Olynyk JK, Park YN, Portmann B, Saxena R, Scheuer PJ, Strain AJ, Thung SN, Wanless IR, West AB (2004) Nomenclature of the finer branches of the biliary tree: canals, ductules, and ductular reactions in human livers. Hepatology 39(6):1739–1745. doi:10.1002/hep.20130
Kietzmann T, Immenschuh S, Katz N, Jungermann K, Muller-Eberhard U (1995) Modulation of hemopexin gene expression by physiological oxygen tensions in primary rat hepatocyte cultures. Biochem Biophys Res Commun 213(2):397–403 (pii: S0006291X85721456)
Hespeling U, Jungermann K, Puschel GP (1995) Feedback-inhibition of glucagon-stimulated glycogenolysis in hepatocyte/Kupffer cell cocultures by glucagon-elicited prostaglandin production in Kupffer cells. Hepatology 22(5):1577–1583 (pii: S0270913995004113)
Gebhardt R, Matz-Soja M (2014) Liver zonation: novel aspects of its regulation and its impact on homeostasis. World J Gastroenterol 20(26):8491–8504. doi:10.3748/wjg.v20.i26.8491
Monga SP (2011) Role of Wnt/beta-catenin signaling in liver metabolism and cancer. Int J Biochem Cell Biol 43(7):1021–1029. doi:10.1016/j.biocel.2009.09.001
Gumbiner BM (1993) Proteins associated with the cytoplasmic surface of adhesion molecules. Neuron 11(4):551–564
Hartsock A, Nelson WJ (2008) Adherens and tight junctions: structure, function and connections to the actin cytoskeleton. Biochim Biophys Acta 1778(3):660–669. doi:10.1016/j.bbamem.2007.07.012
Schmelz M, Schmid VJ, Parrish AR (2001) Selective disruption of cadherin/catenin complexes by oxidative stress in precision-cut mouse liver slices. Toxicol Sci 61(2):389–394
Wickline ED, Awuah PK, Behari J, Ross M, Stolz DB, Monga SP (2011) Hepatocyte gamma-catenin compensates for conditionally deleted beta-catenin at adherens junctions. J Hepatol 55(6):1256–1262. doi:10.1016/j.jhep.2011.03.014
Troxell ML, Gopalakrishnan S, McCormack J, Poteat BA, Pennington J, Garringer SM, Schneeberger EE, Nelson WJ, Marrs JA (2000) Inhibiting cadherin function by dominant mutant E-cadherin expression increases the extent of tight junction assembly. J Cell Sci 113(Pt 6):985–996
Yap AS, Crampton MS, Hardin J (2007) Making and breaking contacts: the cellular biology of cadherin regulation. Curr Opin Cell Biol 19(5):508–514. doi:10.1016/j.ceb.2007.09.008
Puschel GP, Nolte A, Schieferdecker HL, Rothermel E, Gotze O, Jungermann K (1996) Inhibition of anaphylatoxin C3a- and C5a- but not nerve stimulation- or noradrenaline-dependent increase in glucose output and reduction of flow in Kupffer cell-depleted perfused rat livers. Hepatology 24(3):685–690. doi:10.1002/hep.510240335
Elamin E, Masclee A, Dekker J, Jonkers D (2014) Ethanol disrupts intestinal epithelial tight junction integrity through intracellular calcium-mediated Rho/ROCK activation. Am J Physiol Gastrointest Liver Physiol 306(8):G677–G685. doi:10.1152/ajpgi.00236.2013
Miele L, Valenza V, La Torre G, Montalto M, Cammarota G, Ricci R, Masciana R, Forgione A, Gabrieli ML, Perotti G, Vecchio FM, Rapaccini G, Gasbarrini G, Day CP, Grieco A (2009) Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology 49(6):1877–1887. doi:10.1002/hep.22848
Munukka E, Pekkala S, Wiklund P, Rasool O, Borra R, Kong L, Ojanen X, Cheng SM, Roos C, Tuomela S, Alen M, Lahesmaa R, Cheng S (2014) Gut-adipose tissue axis in hepatic fat accumulation in humans. J Hepatol 61(1):132–138. doi:10.1016/j.jhep.2014.02.020
Ulluwishewa D, Anderson RC, McNabb WC, Moughan PJ, Wells JM, Roy NC (2011) Regulation of tight junction permeability by intestinal bacteria and dietary components. J Nutr 141(5):769–776. doi:10.3945/jn.110.135657
Fausto N, Campbell JS, Riehle KJ (2006) Liver regeneration. Hepatology 43(2 Suppl 1):S45–S53. doi:10.1002/hep.20969
Michalopoulos GK (2013) Principles of liver regeneration and growth homeostasis. Compr Physiol 3(1):485–513. doi:10.1002/cphy.c120014
Doi Y, Tamura S, Nammo T, Fukui K, Kiso S, Nagafuchi A (2007) Development of complementary expression patterns of E- and N-cadherin in the mouse liver. Hepatol Res 37(3):230–237. doi:10.1111/j.1872-034X.2007.00028.x
Behari J, Zeng G, Otruba W, Thompson MD, Muller P, Micsenyi A, Sekhon SS, Leoni L, Monga SP (2007) R-Etodolac decreases beta-catenin levels along with survival and proliferation of hepatoma cells. J Hepatol 46(5):849–857. doi:10.1016/j.jhep.2006.11.017
Wei Y, Van Nhieu JT, Prigent S, Srivatanakul P, Tiollais P, Buendia MA (2002) Altered expression of E-cadherin in hepatocellular carcinoma: correlations with genetic alterations, beta-catenin expression, and clinical features. Hepatology 36(3):692–701. doi:10.1053/jhep.2002.35342
Prange W, Breuhahn K, Fischer F, Zilkens C, Pietsch T, Petmecky K, Eilers R, Dienes HP, Schirmacher P (2003) Beta-catenin accumulation in the progression of human hepatocarcinogenesis correlates with loss of E-cadherin and accumulation of p53, but not with expression of conventional WNT-1 target genes. J Pathol 201(2):250–259. doi:10.1002/path.1448
Matsumura T, Makino R, Mitamura K (2001) Frequent down-regulation of E-cadherin by genetic and epigenetic changes in the malignant progression of hepatocellular carcinomas. Clin Cancer Res 7(3):594–599
Rao RK, Basuroy S, Rao VU, Karnaky KJ Jr, Gupta A (2002) Tyrosine phosphorylation and dissociation of occludin-ZO-1 and E-cadherin-beta-catenin complexes from the cytoskeleton by oxidative stress. Biochem J 368(Pt 2):471–481. doi:10.1042/BJ20011804
Kim WD, Kim YW, Cho IJ, Lee CH, Kim SG (2012) E-cadherin inhibits nuclear accumulation of Nrf2: implications for chemoresistance of cancer cells. J Cell Sci 125(Pt 5):1284–1295. doi:10.1242/jcs.095422
Naidu S, Vijayan V, Santoso S, Kietzmann T, Immenschuh S (2009) Inhibition and genetic deficiency of p38 MAPK up-regulates heme oxygenase-1 gene expression via Nrf2. J Immunol 182(11):7048–7057. doi:10.4049/jimmunol.0900006
Kietzmann T, Gorlach A (2005) Reactive oxygen species in the control of hypoxia-inducible factor-mediated gene expression. Semin Cell Dev Biol 16(4–5):474–486. doi:10.1016/j.semcdb.2005.03.010
Dimova EY, Kietzmann T (2008) Metabolic, hormonal and environmental regulation of plasminogen activator inhibitor-1 (PAI-1) expression: lessons from the liver. Thromb Haemost 100(6):992–1006
Day CP, Saksena S (2002) Non-alcoholic steatohepatitis: definitions and pathogenesis. J Gastroenterol Hepatol 17(Suppl 3):S377–S384
Koo SH, Flechner L, Qi L, Zhang X, Screaton RA, Jeffries S, Hedrick S, Xu W, Boussouar F, Brindle P, Takemori H, Montminy M (2005) The CREB coactivator TORC2 is a key regulator of fasting glucose metabolism. Nature 437(7062):1109–1111. doi:10.1038/nature03967
Osawa Y, Seki E, Kodama Y, Suetsugu A, Miura K, Adachi M, Ito H, Shiratori Y, Banno Y, Olefsky JM, Nagaki M, Moriwaki H, Brenner DA, Seishima M (2011) Acid sphingomyelinase regulates glucose and lipid metabolism in hepatocytes through AKT activation and AMP-activated protein kinase suppression. Faseb J 25(4):1133–1144. doi:10.1096/fj.10-168351
Winnick JJ, An Z, Ramnanan CJ, Smith M, Irimia JM, Neal DW, Moore MC, Roach PJ, Cherrington AD (2011) Hepatic glycogen supercompensation activates AMP-activated protein kinase, impairs insulin signaling, and reduces glycogen deposition in the liver. Diabetes 60(2):398–407. doi:10.2337/db10-0592
Kubo K, Sekine S, Saito M (2006) Induction of multidrug resistance-associated protein MRP3 in the liver of rats fed with docosahexaenoic acid. Biosci Biotechnol Biochem 70(7):1672–1680. doi:10.1271/bbb.60019
Peng GP, Sun W, Wu W, Sun Z, Tan XF, Li SP, Chen Z (2008) PD-L1 expression in circulating dendritic cells of patients with chronic hepatitis B. Zhejiang Da Xue Xue Bao Yi Xue Ban 37(4):364–372
Shackelford DB, Shaw RJ (2009) The LKB1-AMPK pathway: metabolism and growth control in tumour suppression. Nat Rev Cancer 9(8):563–575. doi:10.1038/nrc2676
Tan XD, Duan RS, Shi CW, Qu X (2008) Effect of dehydroepiandrosterone on cellular immune response in experimental autoimmune neuritis in Lewis rats. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 24(8):760–763
Nollet EAMC (2013) Integrin and adhesion regulation of autophagy and mitophagy. In: Bailly Y (ed) Autophagy—a double-edged sword—cell survival or death? InTech, pp 1–22. doi:10.5772/55398
Eneling K, Brion L, Pinto V, Pinho MJ, Sznajder JI, Mochizuki N, Emoto K, Soares-da-Silva P, Bertorello AM (2012) Salt-inducible kinase 1 regulates E-cadherin expression and intercellular junction stability. Faseb J 26(8):3230–3239. doi:10.1096/fj.12-205609
Acknowledgments
This study was supported by grants to B. Christ from the German Research Council (CH 109/15-1). Parts of the work presented in this paper were made possible by funding from the German Federal Ministry of Education and Research (BMBF, 1315883 and 315733). S. Winkler was supported through the eALTA Award 2010 (Talecris). C.M. Niessen is supported by the German Cancer Aid, DFG grants SFB829 A1 and SFB832 A3 and Köln Fortune.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Hempel and A. Schmitz contributed equally to the work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hempel, M., Schmitz, A., Winkler, S. et al. Pathological implications of cadherin zonation in mouse liver. Cell. Mol. Life Sci. 72, 2599–2612 (2015). https://doi.org/10.1007/s00018-015-1861-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-015-1861-y