Abstract
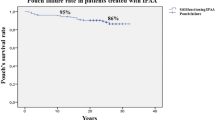
PURPOSE: The aim of this study was to understand better the cause and predictability of pouch failure requiring rediversion after ileal pouch-anal anastomosis and to assess the ultimate outcome of patients in a large ileal pouch series who required rediversion. METHODS: Data from 460 patients completing ileal pouch-anal anastomosis at one institution were recorded from both a prospectively accumulated ileal pouch registry and patient medical records. RESULTS: Of 460 patients, 21 (4.6 percent) who underwent ileal pouch-anal anastomosis required rediversion. Five of these patients subsequently had successful restoration of pouch continuity, leaving a permanent failure rate of 16 of 460 patients (3.5 percent). The most common reasons for rediversion were pouch fistula formation (12) and poor functional results (5). Preoperative factors, including age, previous colectomy, and indication for colectomy, did not predict eventual need for rediversion. Patients requiring rediversion had significantly higher rates of postoperative complications (95 vs.43 percent;P <0.001). Specifically, this group had a higher rate of postoperative pouch fistula (57 vs.3.4 percent;P <0.001). Additionally, a final diagnosis of Crohn's disease significantly predicted the need for rediversion. Permanent pouch failure occurred in 36.8 percent of patients with a final diagnosis of Crohn's disease compared with 1.4 percent of patients with a final diagnosis of ulcerative colitis ( P <0.001). All five salvaged patients had fistula formation in the absence of Crohn's disease. CONCLUSIONS: The overall rate of permanent pouch failure is low. The majority of failures were related to fistula formation associated with Crohn's disease or poor functional results. Pouches complicated by fistulas not associated with Crohn's disease can be salvaged with temporary rediversion.
Similar content being viewed by others
References
Wexner SD, Wong WD, Rothenberger DA, Goldberg SM. The ileoanal reservoir. Am J Surg 1990;159:178–85.
Dozois RR, Kelly KA, Welling DR,et al. Ileal pouch-anal anastomosis: comparison of results in familial adenomatous polyposis and chronic ulcerative colitis. Ann Surg 1989;210:268–73.
Nicholls RJ, Moskowitz RL, Shepard NA. Restorative proctocolectomy with ileal reservoir. Br J Surg 1985;72(Suppl):S76–9.
Galandiuk S, Scott NA, Dozois RR,et al. Ileal pouch-anal anastomosis: reoperation for pouch-related complications. Ann Surg 1990;212:446–54.
Gemlo BT, Wong WD, Rothenberger DA, Goldberg SM. Ileal pouch-anal anastomosis: patterns of failure. Arch Surg 1992;127:784–7.
Hyman NH, Fazio VW, Tuckson WB, Lavery IC. Consequences of ileal pouch-anal anastomosis for Crohn's colitis. Dis Colon Rectum 1991;34:653–7.
Becker JM, McGrath KM, Meagher MP, Parodi JE, Dunnegan DA, Soper NJ. Late functional adaptation after colectomy, mucosal proctectomy, and ileal pouch-anal anastomosis. Surgery 1991;110:718–25.
Author information
Authors and Affiliations
Additional information
Read in part at the meeting of The American Society of Colon and Rectal Surgeons, Chicago, Illinois, May 2 to 7, 1993.
About this article
Cite this article
Foley, E.F., Schoetz, D.J., Roberts, P.L. et al. Rediversion after ileal pouch-anal anastomosis. Dis Colon Rectum 38, 793–798 (1995). https://doi.org/10.1007/BF02049833
Issue Date:
DOI: https://doi.org/10.1007/BF02049833